This is the third of four articles where you can decide on the best strategy when presented with different binocular vision challenges
Your quest continues. Do you accept a third challenge to help enlighten your knowledge of binocular vision? Do you have the skills and courage to solve your patient’s problems and create a loyal patient for life… take the test now!
Your challenge
Your last patient of the day is a 60-year-old builder who has come for an eye examination as he has experienced ‘something unusual’ with his vision. For the past three days he has found it difficult to read close print with his glasses and he has noticed that words appear to be going double. They are ‘one of top of the other’ and ‘slightly to one side’. He then noticed there was more doubling if he looks to the right at his wing mirror when driving. He has since found it more comfortable to shut one eye. He thought it would go away as he has had some very busy days ‘working on an extension’ and has felt very tired for the past month. His general health is fair; he jokes that, although he does manual work, he still needs to lose weight! He has taken blood pressure tablets for the past two years and, when measured a year ago, it was controlled. He denies any injuries and has only had foreign bodies removed from eye casualty in the past. There is no known family history of ocular or systemic disease.
Walkthrough
For each step of the process, decide on the option you wish to take. Then go to the step indicated. When you make the correct choice, you will be helped towards the next step. Once you have completed the challenge it should become clear which is the most systematic approach to investigate the child with reduced vision in one eye.
STEP 1 You measure his VAs. He reads R 6/6 L 6/6 and N5 with his current spectacles. He cannot do binocular VAs as he can see two images. What do you do next?
a) You decide to look at the patient to observe his head posture – go to 2
b) focimeter his spectacles – go to 3
STEP 2 His head posture appears normal but he is clearly trying to shut his LE. Go to 4
STEP 3 That is not a bad idea, especially if new spectacles have recently been collected. It reads R+2.00DS L+2.25DS, there is no induced prism. You also observe his head posture in case there is a compensatory head posture. It looks normal. Go to 4
STEP 4 You check pupil reactions which appear normal. You breathe a little easier and you remember this usually means something less serious. You decide to check cover test. Which will you do?
a) Cover and uncover test and alternating cover test ? – go to 5
b) Both tests in all directions of gaze ? – go to 6
STEP 5 You see he has a L moderate hypertropia with good recovery. You remember he mentioned the diplopia was worse on right gaze. Go to 6
STEP 6 You pick up your pen torch and watch his eyes carefully and perform cover test in the directions he reports diplopia (figure 1). You see that he has a L hypertropia which is worse on R gaze, up to the R and down to the R. Do you
a) check this cover test on head tilting to the left – go to 7
b) right shoulder – go to 8

Figure 1: Cover test in extreme gaze
STEP 7 As he tilts his head to the left, the hypertropia is evident. You check there is no hypertropia when tilting to the right. Go to 9
STEP 8 There appears to be no hypertropia on head tilt to the right. Go to 7
STEP 9 You dig out your binocular vision text book and look at the anatomy diagrams. Which muscle(s) do you think are underacting (figure 2)?
a) R superior rectus – go to 10
b) R superior oblique – go to 11
c) L inferior rectus – go to 12
d) L superior oblique – go to 13

Figure 2: Extraocular muscles
STEP 10 A right superior rectus under action would result in a L hypertropia as seen here. The deviation would also be maximal in right gaze as that is the direction where the superior rectus has maximum action. However, you would expect the L eye to be the fixating eye (R hypotropia). You reconsider. Go back to 9
STEP 11 The R superior oblique pulls the eye ball down so, if this was underacting, the eye would be elevated and give a R hypertropia. You reconsider. Go back to 9
STEP 12 The L inferior rectus underaction would result in a L hypertropia. However, its action would be maximal in L gaze not right gaze as seen here. You go back to reconsider your options. Go back to 9
STEP 13 That is correct. The L superior oblique is a depressor and its under action would result in a L hypertropia. Its action is maximal in adduction (on R gaze) which results in the hypertropia being worse on R gaze. On head tilting, the L superior rectus is unopposed by the L superior oblique which would lead to the LE shooting up. How do you determine if this is a L superior oblique palsy or L 4th cranial nerve palsy? Go to 14
STEP 14 You do a forced duction test Go to 15
Look for secondary sequelae. Go to 16
STEP 15 A forced duction test would determine whether this was a mechanical (in which case there would be no movement in the down and left gaze) as opposed to a neurogenic cause. Go to 16
STEP 16 Secondary sequelae would not appear within a few days of the original palsy and none are found here. Go to 17
STEP 17 What is the likely aetiology?
a) not enough information to ascertain.
b) aneurysm – go to 18
c) microvascular disease, eg undiagnosed diabetes type 2 – go to 19
STEP 18 An aneurysm would most likely cause incomplete or complete 3rd nerve palsies. Go to 19
STEP 19 For his age group and symptoms of tiredness, you may suspect systemic disease. Go to 20
STEP 20 This is a possible cause given his symptoms, age group and presentation. More commonly, the 6th nerve is affected but any of the cranial nerves can be included. What is your management of this patient?
a) refer via GP to rule out diabetes and blood tests. Go to 21
b) refer to eye casualty department within one week. Go to 22
c) Monitor this patient. Go to 23
STEP 21 This patient may need imaging to rule out further neurological pathologies. They would need to have blood tests to rule our diabetes but also onward referral to a hospital eye service.
STEP 22 This may seem extreme but potentially he may need imaging to rule out any other pathology in the brain. If referred via the GP, you would need to consider would he be seen within a week or two? Could he in the meantime suffer a more serious neurological/ischaemic/life-threatening incident? Indeed, it would be best to err on the side of caution. He could go the next day but it would be in his best interest to rule out life-threatening disease as soon as possible. Well done and continue below for more information about diplopia.
STEP 23 All new incomitancies would require further investigation to rule out systemic and ocular disease. Go back to 19.
You have completed this level – congratulations!
Differential diagnosis of diplopia
When a patient presents with diplopia we need to decide if this is normal, or would warrant further investigation and referral. The first few causes to rule out would be: monocular diplopia and whether there is an incomitancy.
A good history and symptoms is required to aid diagnosis:
1 Onset – a vague onset especially from childhood or from ‘years ago’ would indicate a long standing condition and less likely to be sight or life-threatening. Recent onset or a change in diplopia would be more suspicious.
2 Monocular or binocular – does the diplopia go if one eye is occluded? If it is monocular, likely causes include media opacities (figure 3). Some patients refer to ‘blur’ as double vision therefore careful questioning is required. For the rest of the article we will deal with binocular diplopia.

Figure 3: Cataract is a possible cause of monocular diplopia
3 Description of diplopia – more in distance and near, horizontal or vertical, does it change in direction of gaze, associated with any particular visual task?
4 Pain – a painful eye associated with 3rd nerve palsy can be caused by an aneurysm at the posterior communicating artery and life-threatening.
5 Any recent injury– trauma such as blow out fractures, can cause incomitancies as can recent eye surgery (either strabismic, retinal detachment repair and insertion of a scleral buckle).
6 Presence of ill health or common systemic illnesses or, in cases of non-diagnosed diseases, their symptoms. This would include, microvascular disease, eg diabetes/hypertension/hypercholesterolemia, malignant disease (including those caused by metastases), myasthenia gravis, Parkinson’s, Alzheimer’s, orbital inflammatory diseases, eg hyperthyroidism.
7 Medication – especially a change or new prescription with the onset of symptoms.
Concomitant and incomitant strabismus
Patients with well controlled or long standing strabismus rarely complain about diplopia. They will have adaptive strategies such as suppression of one image, abnormal head postures or inform you they ‘can ignore’ the second image. Concomitant strabismus describes a deviation that does not change in magnitude dependent on the direction of gaze. These usually include all the congenital heterotropias, such as esotropia, exotropia and heterophoria that can break down to heterotropia. The only suspicious diplopia reports are related to pathologies that can cause existing well controlled phoria or tropia to break down as they extend beyond the fusional ranges.
Congenital v acquired
An incomitancy would be described when the diplopia varies in magnitude in different directions of gaze. Incomitancies can be congenital in origin, either due to abnormal insertions of muscles anatomically such as in Brown’s syndrome or due to nerve pathway anomalies such as in Duane’s retraction syndrome. In young children, these would benefit from routine referral on first presentation for the parents to know the diagnosis. With nerve pathway anomalies, other sensory deficit might also be usefully screened for. Patients presenting with congenital incomitancy in later life are usually less aware or bothered that they have diplopia and are often asymptomatic. They may remember that they have had diplopia since childhood and may have photos showing compensatory head postures. Recent onset incomitancy symptoms normally indicate it is acquired and usually is accompanied by pathology or trauma. The patient is usually able to pinpoint exactly when they first noticed it. They may also be aware that, if they close one eye or adopt an abnormal head posture, they can get rid of their symptoms.
Mechanical v neurogenic
The aetiology of incomitancy also plays a factor in determining the management of diplopia. Mechanical causes include the anatomical anomalies, such as the Brown’s nodule at the pulley of the superior oblique muscle, injury caused by forceps delivery, whiplash injury, blow out fractures, and systemic diseases (such as thyroid eye disease causing physical obstruction to the extra ocular muscle movement). Neurogenic causes refer to the stopping of the signal along the nerve pathway to the extraocular muscle resulting in limiting movement, which can be partial (paresis) or complete (palsy) and caused by some of the factors listed above.
Investigation of the diplopia and its management
Tests required:
- VA.
- Motility.
- Ductions (forced) and versions.
- Cover test in all direction of gaze, at distance and near.
- Maddox rod/wing.
- Pupil reactions.
- Fixation disparity (aligning prism on Mallet unit).
- Bielschowsky head tilt test/Parks three step test.
- Hess Screen (figure 4).
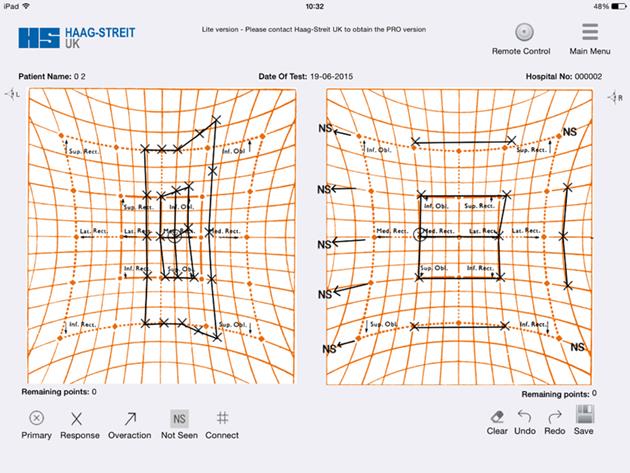
Figure 4: A Hess chart reading showing loss of abduction in one eye and sequelae – what might cause this?
Possible causes:
Non-urgent
a) Refractive error/spectacle dispensing/contact lenses.
b) Decompensated heterophoria or heterotropia.
c) Physiological/malingering /non-organic causes.
More urgent
d) Ocular pathology.
e) Systemic causes.
f) Trauma.
a) Refractive error
A refractive error uncorrected may lead to diplopia if a pre-existing muscle imbalance breaks down. A large change in refractive error prescribed may also lead to similar problems. Be aware of the relationship especially in pre presbyopes of how accommodation and accommodative convergence can alter the control of deviations. For example, prescribing less hypemetropia would increase the accommodative convergence and could break down a controlled esotropia. Contact lens fitting off centre or multifocal contact lens can induce monocular diplopia. Patients with prescribed prism in the spectacles switching to contact lens may find their control breaking down.
Tests required:
- Refraction (including cycloplegia if required).
- Cover test.
- Fixation disparity.
- Focimetry.
Management:
Always check ocular motor balance with cover test and or fixation disparity after refraction to compare with results obtained with patient’s existing spectacles.
Existing prisms in spectacles are easily missed by focimetry. Refit with contact lenses if suitable.
b) Decompensating heterophoria or tropia
Details of patient’s previous records would always be useful here for comparison purposes. These could include change in visual demand, ill health or change in spectacles.
Tests required:
- cover test.
- motility.
- fixation disparity.
- near point of convergence.
- stereo-acuity.
Management:
Find out what has caused the decompensation and remove if possible.
c) Physiological/malingering/non-organic
Some patients, especially very observant children, may report physiological diplopia. This can manifest if one is focused, eg on a finger and they are aware things in the distance appear horizontally diplopic. For malingerers, they can report any variety of symptoms, especially if the practitioner asks in history and symptoms ‘do you get headaches/double vision, flashes or floaters?’. They may just reply positively to everything.
Tests required:
A careful history taking is required here. All of the above binocular vision tests should be normal.
Management:
Reassurance may all that is required and only refer to GP to treat underlying cause of ‘lying’ as appropriate.
d) Ocular pathology
Most pathologies that occur within the eye are linked to systemic disease. Those which restrict eye movements for example by enlargement of the extra ocular muscles would cause mechanical restriction. These would include orbital inflammatory disease caused by hyperthyroidism, Hashimoto’s thyroiditis, sarcoidosis and granulomatosis. Orbital inflammation or meningioma, carotid-cavernous fistula may affect all three cranial nerves.
Tests required:
- Observation – to look for proptosis, lid lag.
- Measurement of exophthalmos.
- History – systemic symptoms or diagnosis.
Management:
Compression of the optic nerve can lead to blindness and requires prompt referral ophthalmological opinion for orbital wall decompression. Also rule out systemic disease if not already diagnosed.
e) Systemic disease
The supernuclear pathway is responsible for saccades, vergences and gaze and these palsies often do not result in diplopia, eg both eyes cannot look to the right. The infranuclear pathway which comprises the cranial nerves and extra ocular muscles and can be affected by a variety of systemic diseases. They can be subdivided into vascular, tumour, and neurological causes.
Vascular diseases, such as diabetes or hypertension, can lead to individual extraocular muscles being affected, eg painless 3rd nerve without pupil involvement.
The higher centres for eye movement in the brain can be affected by a stroke. Aneurysm of the posterior communicating artery and internal carotid can lead to painful palsies with pupil involvement.
Brain tumours may first be noticed as they impact upon a nerve, such as an acoustic neuroma affecting the 6th nerve (causing a lateral rectus palsy). Raised intracranial pressure can also cause stretching of the 6th nerve over the petrous bone causing a palsy.
Demyelinating diseases such as multiple sclerosis may affect 6th nerve.
Tests required:
All binocular vision tests should be undertaken to determine which cranial nerve affected.
Management:
Urgent referral for ophthalmological or neurological
investigation.
f) Trauma
The fourth nerve is a very long nerve and has a long pathway from the brain stem to the superior oblique muscle. Therefore, trauma can cause fourth nerve palsies, eg whiplash in road traffic accidents.
Tests required:
The history of injury and the presence of a nerve palsy determined by all binocular vision tests. Bilateral 4th nerve palsies also common in injury.
Management:
Urgent referral for hospital investigation. In children who cannot/do not give a history presenting with obvious injury (bruising, bleeding), child protection (safeguarding) procedures may need to be considered.
Summary
In this case, recent onset incomitancy which was diagnosed as a left fourth nerve palsy needs urgent referral for ophthalmological and medical assessment. The features are:
- recent onset diplopia.
- hypertropia in the affected eye (left eye).
- vertical diplopia worse on contralateral gaze (right).
- increased hypertropia on head tilt to the ipsilateral (same) side (left).
Ms Sosena TW Tang practises at Aves Optometrists, Ware, Herts and at the QEII Hospital East and North Herts NHS Trust.
Useful reading
David Newsham and Meritxell Cristino Amenos. Recent advances in the management of amblyopia, OIP, Volume 12, Issue 3, 2011.
