Contact lenses constructed in rigid gas permeable (RGP) materials are classified by their predominant bearing surface. Those that rest their weight on the cornea are known as corneal RGP contact lenses (corneal for short) while those that are sufficiently large and fit in such a way that the lens bears on both the conjunctiva and cornea are termed corneo-scleral RGP contact lenses (corneo-scleral for short). Lenses that vault the cornea and rest on the conjunctiva are known as scleral RGP contact lenses (scleral for short) and it is these lenses which are the focus of this series of articles.
While scleral lenses are generally larger than corneo-sclerals, which in turn are generally larger than corneal lenses, a fixation on lens size can cause confusion. A lens which is 14.8mm in diameter for example may be sufficiently large to be fitted ‘as a scleral’ and therefore vault a small cornea, while a similar 14.8mm lens may barely reach the limbus when placed on a larger cornea.

Figure 1: Microvault on a scleral lens
Originally blown from glass, the first scleral lenses (and the first contact lenses for that matter) were poorly tolerated, dangerously fragile and gas-impermeable. Not unsurprisingly they failed to catch on. The basic concept, however, had merit and with advances in lens design, gas permeable lens materials, surface treatment and improvements in manufacturing techniques the majority of the original pitfalls have been overcome.

Figure 2: Without microvault
Proper insertion of a scleral lens traps a layer of saline (or other suitable fluid) between the cornea and lens back surface which is known as the tear reservoir. Without this the corneal refractive power is not adequately neutralised making refractive correction impossible. Without this hydrating tear reservoir the cornea will also quickly dehydrate which causes discomfort and makes the lens unwearable. The peripheral portion of the lens (known as the scleral landing zone) is responsible for maintaining this reservoir of saline by aligning sufficiently with the conjunctiva. Too steep/tight and the lens will indent the ocular surface and occlude the conjunctival vessels (vessel blanching, figure 4) causing redness and discomfort. Peripheral curves which are too flat/loose will cause a leak and introduce tear film debris or bubbles. A well-fitting scleral lens exhibits little to no movement on eye and is comfortable all day. Table 1 summarises some terms used in scleral lens practice.

Table 1: Summarises a number of terms relating to scleral lens design
Scleral lens indications
Scleral lenses have a unique set of optical and therapeutic benefits which makes them invaluable to our contact lens arsenal. Their rigid optics and stability can provide excellent optical correction even on the most irregular of corneas. While other lens types force the practitioner to directly fit any corneal irregularity, the success of a scleral lens is reliant the practitioner’s ability to fit the sclera/conjunctiva while selecting a lens of optimal vault. The degree of corneal irregularity becomes much less important.

Table 2: Summarises currently available scleral lenses
Irregular cornea
The current primary use for scleral lenses is the visual correction of corneal irregularity. The unique design and fitting characteristics of scleral lenses make them an excellent choice for patients with all types of distorted and diseased corneas. Scleral lenses provide the irregularity masking properties of rigid materials on a stable and well centred platform. The lid-lens interaction and foreign body problems inherent in corneal RGP contact lens wear is avoided in scleral lens wear. Scleral lenses prevent corneal desiccation and cannot dehydrate, which make them particularly useful to patients who are intolerant to other lens types. Patients with conditions such as keratoconus, pellucid marginal degeneration, corneal scarring, keratectasia, post-lasik and post-radial keratotomy oblate corneas and corneal grafts often make ideal scleral lens wearers, providing their endothelium has adequate cell density to prevent hyopoxia.

Figure 3: Clearance between the lens and optical surface
Therapeutic
The tear reservoir makes scleral contact lenses useful to the management of corneas that need constant hydration or protection from the shearing forces of the lids. Patients with severe dry eye, ocular cicatricial pemphigoid, Stevens-Johnson syndrome or persistent epithelial defects (for example) can therefore receive therapeutic benefits and pain relief from scleral lens wear.

Figure 4: Conjunctival vessel blanching
High Rx
Historically, patients with a very high prescription or astigmatism (for example over +/- 15DS or over 6DC) had few options when it came to contact lens wear. RGP lenses are generally the recommended method of vision correction due to the superior optics they offer. If these were not well tolerated, soft lenses could be fitted, but frequently the visual acuity will suffer, particularly with high levels of astigmatism. Scleral lenses can now be fitted with great success for patients who require good comfort (without the peccadillos of corneal RGPs such as dust under lenses), and sharp, stable vision. If a front surface toric is needed these can be well stabilised with peripheral toric curves.
Sport
The size and stability of scleral lenses make them a great choice for people wishing to wear contact lenses for sports, particularly if there is a concurrent indication such as a high Rx or corneal disease. They are highly unlikely to fall out, even in contact sports, and will not move or dislodge during rapid eye movements.
Recent advances and increasing usefulness
Historically, fitting scleral lenses has been the domain of a handful of experienced specialist lens fitters, reserved for the most extreme corneal distortions and ‘problem cases’. There have always been a number of notable drawbacks of fitting sclerals, but a better understanding of the benefits of these lenses has led to an increasing demand for scleral lenses. This in turn has prompted a revolution in modern manufacturing techniques for large diameter lenses which has made many of these issues a thing of the past.
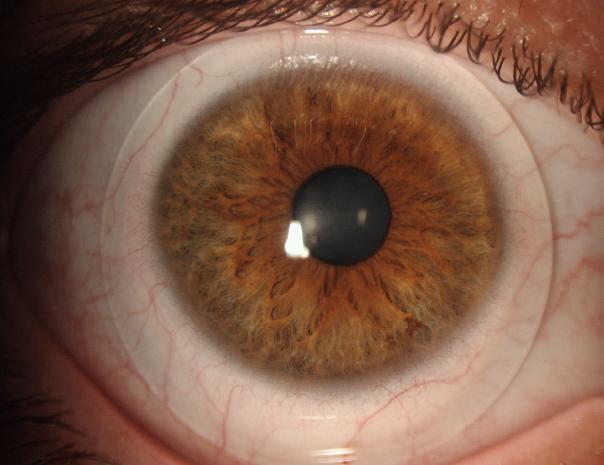
Figure 5: Mini scleral
Cost
Due to increasing demand for scleral lenses, more competition among lens manufacturers, and computerised lathes allowing for quick, repeatable production, the cost of fitting them has become significantly lower and therefore less prohibitive for both practitioner and patient to embark upon.
Many suppliers offer two or more exchanges free of charge, and will often provide a full refund (subject to handling charge) if the fitting is unsuccessful. Lathed, non-impression sclerals vary in price from around £50 to £130 depending on design, though impression moulded lenses may be significantly more. Many suppliers will provide a fitting set free of charge providing a certain number of orders are placed.
Handling
Although in reality a 23mm lens can be easier to handle for someone with poor dexterity than a smaller diameter lens, they were perceived by patients and practitioners alike as being a bit ‘scary’. These large ‘full sclerals’ may also be unsuitable for those with small eyes or tight lids. Scleral lenses are now readily available in a wide range of diameters, to suit the requirements of the patient’s condition, corneal size and depth, palpebral aperture and handling ability.
Corneal impression moulds
If a standard rotationally symmetrical trial scleral lenses did not provide adequate conjunctival alignment (allowing leakage and bubble formation) it used to be necessary to take an impression of the front of the eye using dental putty, so an impression scleral lens could be made to fit the eye precisely. Although this is still required in some cases, the availability of toric scleral curves allows even the most irregular sclerals to be fitted with good 360º alignment. A toric periphery fitting set and good knowledge of your preferred design is advisable.
Residual astigmatism
As a general rule, when fitting an irregular cornea the very presence if a rigid lens surface is, the majority of the time, sufficient to correct the irregular astigmatism present. In these cases, a spherical powered lens will do an excellent job of correcting the full prescription. However, there are times when the patient reports their vision is still ‘shadowy’, and we find a residual cylinder in careful over-refraction. In the past, this meant either the patient putting up with slightly blurry vision, or top-up spectacles worn over the lenses. It is now possible with many designs of scleral lens (notably the ICD16.5, Zenlens and Maxim CV) to add a front-surface toric power to the lens in order to provide the full correction. This is usually stabilised with a toric periphery, prism ballast or dynamic stabilisation.
Oxygen permeability
Larger sclerals of 22mm or greater diameter have historically been thick lenses, up to around 1mm thickness in some cases. Oxygen permeability of such lenses is therefore fairly low, which can be of concern in some cases. This is particularly relevant in ocular surface disease and post-graft corneas, where oxygen requirements may be higher than usual. Modern scleral lenses are around 0.3-0.4mm thick, and made from materials with a Dk over 100. Providing the lens is fitted without excessive clearance, the oxygen reaching the cornea is usually sufficient to prevent hyopoxia (in the author’s experience). It should be borne in mind that corneal grafts often have higher oxygen requirements than a non-grafted eye (due to a compromised endothelium), so it is important to make sure scleral lenses for such eyes are not unduly thick (minimising the plus power by flattening the base curve can help). It is essential to monitor these patients regularly and ensure wearing times are not excessive.

Figure 6: Tear reservoir. Image courtesy of Dr Vijay Anand
Manufacturing repeatability
Scleral lenses are cut using computerised lathed precision software, and are therefore highly repeatable. Many designs incorporate special algorithms so that when the scleral landing area is adjusted or the base curve is modified, the overall sagittal depth of the lens remains the same.
Pingueculae (and other conjunctival lumps and bumps)
Large diameter scleral lenses may be able to vault pingueculae and raised lesions lying close to the limbus, and some lens designs can be ‘notched’ to skirt around these lesions. However, they can still be a major obstacle or indeed a contraindication when considering fitting a scleral lens on an eye. If the lens edge lands directly on a pinguecula it can quickly become red and inflamed, and can sometimes disrupt the sealing of a lens and cause it to move excessively or allow bubbles to form under the lens. One scleral lens design in particular has a novel way to overcome these issues – the Zenlens Mini-Scleral has the option to add a ‘Microvault’ (MV) to the lens profile. This is a precisely defined flute or ripple in the edge of the lens to vault it over the raised area (figure 1). It is possible to specify the axis of the MV at the edge of the lens, where the highest point of the MV sits, and both the height and width of the ‘ripple’. Figure 2 shows how an MV of 300 microns was employed to alleviate the pressure on a pinguecula to improve comfort and redness (the image actually shows slightly excessive clearance but there was no visible stand-off and comfort was excellent).
Conclusion
In this article we have highlighted the increasing popularity and availability of scleral lenses, and discussed their various indications and benefits in the management of a wide range of contact lens patients.
Sophie Taylor-West is a contact lens specialist working in private practice in Brighton. Matthew Carter is a Principle Optometrist in the Contact Lens department at Moorfields Eye Hospital and also works in private practice in Kent.
