This is the second part of a two-part review of diabetes mellitus. This increasingly common condition has many complications that affect many different systems in the body. Management of diabetes requires collaboration between a wide range of medical professionals. This second part of the review covers how patients suffering with diabetes monitor their condition and the different options for management.
Monitoring
Blood glucose concentration
[CaptionComponent="2694"]
Measurement of blood glucose level is often referred to as BM, which stands for Boehringer Mannheim. This was the name of the company, now called Roche, that produced the test strips for the measuring devices. Glucose monitoring gives a reading of the approximate concentration of glucose in the patient’s blood at the time of testing. The glucose meters are small devices that patients will carry with them and use to take regular readings (Figure 1). The glucose reading allows the patient to make appropriate adjustments to their insulin doses throughout the day. It is also extremely useful for identifying emergency conditions such as hypoglycaemia and DKA.
There are many varieties of glucose meters. Some are adapted for patients with visual impairment by having a talking function or a larger and bolder display.
Blood glucose monitoring has been the basis of the definitions for diabetes and its related conditions for many years.
Patients should aim for a blood glucose level of:
? 4.0-7.0mmol/litre before meals
? <9.0mmol/litre after meals1,2,3,4
HbA1c (glycated haemoglobin)
HbA1c is a form of haemoglobin created after prolonged exposure to glucose. The proportion of HbA1c in the blood therefore gives an indication of the average plasma glucose levels over the preceding 2-3 months. This test gives a much better indication of the quality of a patient’s glycaemic control than isolated blood glucose readings. This is a laboratory blood test and should be performed every 2-6 months, and usually more frequently following a treatment intervention.
Patients will agree a target HbA1c with their doctor but it is usually:
HbA1c of between 6.5 and 7.5 per cent (this represents 48-58 mmol/mol)
Patients should be advised that any improvement in HbA1c will be beneficial even if they do not reach their target, and that the greater the improvement, the greater the benefit.1,2,3,4
Urine testing
[CaptionComponent="2695"]
Urine is tested using dipstick strips that contain coloured squares that will react and change colour in response to the composition of the urine (Figure 2). The change is compared to a chart on the strip container to give a measurement. Glucose can be detected using these strips, but this is a less accurate method to blood testing since there is usually no glucose in the urine until blood concentrations reach 10mmol/l, which is already considered high. Also, they cannot detect hypoglycaemia which is very important, especially for patients using insulin. Nevertheless urine testing can be useful, particularly as a screening tool in GP practices.
Urine testing can also be used to detect protein in the urine. This can be a simple way of checking for signs of diabetic renal impairment.
Regular review5
Diabetic eye screening
Patients should have their eyes screened on an annual basis with visual acuity, and digital photography after mydriasis with tropicamide.6 Review may be more frequent if clinically indicated. Although the gold standard for diabetic assessment is slit lamp indirect ophthalmoscopy, this is not practical for mass screening, so where this is not available, the national retinopathy photographic screening programme tries to ensure that most diabetics are photographed and graded annually. Unfortunately, many type 2 diabetics are too obese to sit at a slit lamp or fundus camera. In these cases, portable fundus cameras such as DIO (digital indirect ophthalmoscope from Carleton Optical) or even direct ophthalmoscopy can be used. Complications of diabetes should be referred depending on severity – see later article in this series on diabetic retinopathy.
Foot checks
[CaptionComponent="2696"]
Diabetic patients have annual structured foot surveillance. These are appointments with a diabetic specialist who will check for skin condition, shape and deformity, impaired sensory nerve function, vascular supply, peripheral pulses and will check the patient’s shoes. An important part of these sessions is also to educate the patient of the risks of foot ulcers in diabetes and the importance of regular and thorough checking of the feet (Figure 3).7,8
Diabetic renal monitoring
All diabetic patients with or without identified diabetic nephropathy should have albumin to creatinine ratio measured from a first-pass morning urine sample once a year. If the result is found to be abnormal, then the test should be repeated at the next two clinic appointments, which should be within the next 3-4 months. The estimated glomerular filtration rate (eGFR) should also be calculated and used to stage the level of kidney disease.
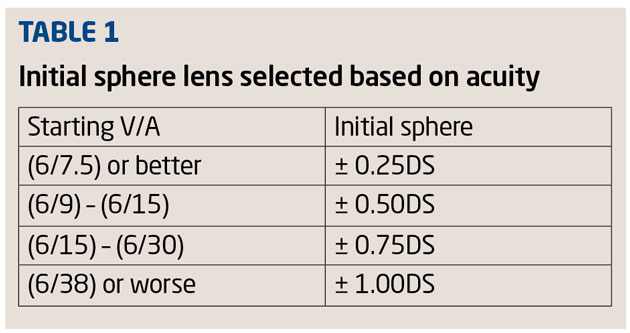
If any of these results are abnormal, renal disease other than diabetic nephropathy must be considered and fully investigated, especially if there are few other signs of progressive disease or if there are other symptoms such as haematuria. The severity of impairment of a patient’s renal function is graded according to the criteria outlined in Table 1.
If renal function continues to deteriorate, then the patient may be referred to a renal specialist for regular review and management.9
Psychological problems
All professionals involved in the care of diabetic patients need to be alert to the signs of psychological conditions which can often be associated with diabetes. Depression and/or anxiety are the most common. These problems can have a severe impact of the patient’s life and it is important that they are identified and managed. First-line measures such as counselling and appropriate pharmacological management are usually overseen by the patient’s GP. Referral to relevant psychological and psychiatric specialists can be made if necessary.
Blood pressure
Blood pressure should be measured regularly and as part of the annual diabetes review. Target blood pressure for a normal patient is <140/85mmHg, but a diabetic patient should have a target of <130/80mmHg at rest. Blood pressure is not an indicator of the severity of diabetes, but it does dramatically increase the risk of diabetic complications if raised.1,3
Lipid profile
A full lipid profile including cholesterol levels should be performed after diagnosis and then be monitored regularly. If the results are raised and the patient also has a high cardiovascular risk then they may be started on a statin (eg simvastatin) by their GP.
Smoking
Smoking also greatly increases the risk of developing diabetic complications. If the patient requires help stopping, referral should be made to the local smoking cessation services. Optometrists are increasingly involved in such programmes (Optician will be publishing a feature about this in the coming weeks).
Associated medical conditions
(type 1)
Type 1 diabetes is often associated with other autoimmune conditions. Serological testing for coeliac disease should be offered. Healthcare professionals should be alert to, and investigate signs of thyroid disease, Addison’s disease, pernicious anaemia and other autoimmune conditions.1
Management of diabetes
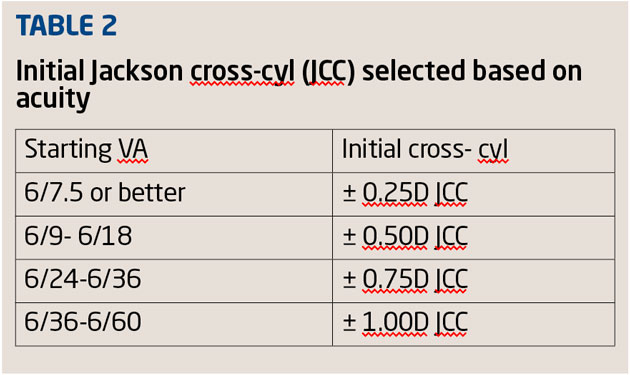
There are many different choices of medications to manage diabetes that are adjusted depending on the response of the individual patient. However, the management broadly speaking follows the pathway in Table 2.2,4
Diet and lifestyle advice
This is the first step in management of diabetes and if implemented well is often the most effective. Patients are advised to increase the amount of physical exercise they are doing each week and to modify their diet to reduce the fat and sugar content. For type 1 diabetics, it is important that they closely monitor their food intake and exercise so that they can anticipate how much insulin they will need to administer. For type 2 diabetics, reaching a normal BMI and having a healthy lifestyle can greatly slow the process of the disease, and in many cases, lifestyle and diet changes alone will be enough to control it.1,3
Metformin
For type 2 diabetes only, metformin is from the biguanide class of drugs and originates from French Lilac (Galega officinalis). It has been used in folk medicine for centuries but was first described in medical literature by Emil Werner and James Bell in 1922.10,11 It is normally the first-line treatment for type 2 diabetes. Its primary method of action is to suppress glucose production in the liver (hepatic gluconeogenesis), and so reduce the level of glucose in the blood. Metformin has been known to cause diarrhoea in some patients and must be used with caution in those with severe renal impairment due to a risk of lactic acidosis.12,13 However, it is generally considered to be a very safe and effective drug and is now the most commonly prescribed anti-diabetic drug in the world.10
Sulphonylurea
Sulphonylureas (eg gliclazide) are used in type 2 diabetes only. They act by increasing the release of insulin from pancreatic beta cells. They were discovered by accident when Marcel Janbon and his colleagues were studying sulphonamide antibiotics and noticed that the compound caused hypoglycaemia in their animal studies.14 Sulphonylureas are normally used with Metformin as part of dual therapy, or can be as an alternative if metformin is contraindicated, if the patient is not overweight, or if a rapid response is required to control hyperglycaemic symptoms. Unlike metformin, sulphonylureas can cause hypoglycaemia and the patient must be made aware of this.12,15
Dipeptidyl peptidase-4 (DPP-4) Inhibitors
DPP-4 inhibitors (eg sitagliptin) are a newer class of anti-diabetic drug that act by increasing the levels of the hormone incretin. Incretin inhibits the release of glucagon, which in turn increases the release of insulin, slows gastric emptying and decreases blood sugars. DPP-4 inhibitors are currently used as part of triple therapy with Metformin and Sulphonylureas as an alternative to insulin therapy. The first of these drugs was only licensed in 2006. They have been shown to give extremely good glycaemic control. As their effects are increasingly recognised and the cost is reduced it is likely that they will become a far more common part of diabetic treatment.12,15
Insulin therapy
[CaptionComponent="2697"]
The name insulin comes from the Latin insula meaning island, and refers to the Islets of Langerhans in the pancreas where the insulin is produced. Solving the problem of how to produce and extract insulin in a usable form is a fascinating story and one which earned Frederick Banting and JJR Macleod the Nobel Prize in Physiology or Medicine in 1923. Insulin therapy revolutionised our understanding and treatment of diabetes and remains the basis of treatment of diabetic patients.16
Insulin regimens in type 1 diabetics are very much built around the individual patient. They can be multiple injection regimens or twice-daily regimens for those who find adherence to lunchtime injections difficult. Baseline and nocturnal glycaemic control is maintained using neutral protamine Hagedorn (NPH) (eg humalin I) or long-acting insulins, with rapid acting insulin (eg Novarapid) before meals. Patients will adjust their doses of insulin according to the amount of food they have eaten, exercise they have done, and the BM measurement.
Excess insulin can cause hypoglycaemia. The patient will feel shaky, sweaty and it can cause a coma. Patients must be educated on these risks and taught to be aware of the early signs so they can correct the hypoglycaemia by eating something sugary. Severe hypoglycaemia is a medical emergency and may require hospital admission.1,2
Insulin is only used in type 2 diabetes when there has been poor glycaemic control despite the use of first and second line treatments. Most type 2 diabetics are started on NPH insulin (eg humalin I) twice a day. These are intermediate-acting forms of insulin that the patient will self-administer by subcutaneous injection. If the patient needs assistance or their lifestyle makes twice daily insulin difficult, it may be appropriate to choose a long-acting insulin (eg insulin glargine) instead which can be given once a day.
If, despite these measures, the patient continues to have poor glycaemic control then it may be necessary to add in a short-acting insulin (eg Novarapid) before meals or a mixed preparation. Insulin regimens and the doses administered vary greatly between patients. They are often adjusted and titrated when the insulin therapy is being started until a suitable regimen is reached.2,3,15
Conclusion
Diabetes mellitus is a condition that requires input from a wide variety of healthcare professionals to be managed effectively. It is becoming increasingly common largely due to the increasing prevalence of obesity and subsequently type 2 diabetes. With rapid urbanisation, this is true on a global scale and not just in Western countries. While diabetes mellitus has many complications that affect many different systems in the body, the primary focus of treatment is to maintain good glycaemic control. When blood sugar levels are consistently stable, most of these complications can be largely prevented. It is an important part of the role of all healthcare professionals involved in a patient’s care to ensure that they are aware of the importance of this, and to offer any support they can.
References
1 National Institute for Health and Care Excellence. Type 1 Diabetes: Diagnosis and management of type 1 diabetes in children, young people and adults. NICE clinical guideline 15. 2004.
2 National Institute for Health and Care Excellence. Managing Type 1 Diabetes in Adults. NICE Pathways. November 2013.
3 National Institute for Health and Care Excellence. CG66 Type 2 diabetes: full guideline, 2008.
4 National Institute for Health and Care Excellence. Managing Type 2 Diabetes in Adults. NICE Pathways. November 2013.
5 National Institute for Health and Care Excellence. Ongoing Care For Adults With Type 1 Diabetes. NICE Pathways, November 2013.
6 Royal College of Ophthalmologists. Diabetic Retinopathy Guidelines. December 2012.
7 National Institute for Health and Care Excellence. Foot care for people with diabetes. NICE Pathways. November 2013-12-09.
8 National Institute for Health and Care Excellence. Type 2 diabetes – footcare. NICE clinical guideline 10 (2004).
9 Delli A, Kong A. Type 1 Diabetes, in R Holt, C Cockram, A Flyvbjerg, B Goldstein. Textbook of Diabetes, 4th Edition. Wiley-Blackwell Publishing. 2010.
10 C Bailey. Metformin: its botanical background. Practical Diabetes International. April 2004. Volume 21. Issue 3, p115-117.
11 L Witters. The blooming of the French lilac. Journal of Clinical Investigation. October 2001. 108(8): 1105-1107.
12 National Institute for Health and Care Excellence. Blood-glucose-lowering Therapy for Type 2 Diabetes. NICE Pathways. November 2013.
13 British National Formulary 63. BMJ Group, Pharmaceutical Press. March 2012.
14 J C Henquin. The 50th anniversary of hypoglycaemic sulphonamides. How did the mother compound work? Diabetologia, Oct 1992. Volume 35. Issue 10 P907-912.
15 National Institute for Health and Care Excellence. Type 2 diabetes – newer agents (partial update of CG66) NICE clinical guideline 87 (2009).
16 M Worek. Nobel: A Century of Prize Winners, Second Edition. Firefly Books, 2010.
? Dr Andy Want is a doctor with a special interest in diabetes and is based at Wexham Park and Heatherwood NHS Trust, Berkshire
Model answers
(Correct answer is in bold text)
1 Which of the following gives the most temporally stable result?
A Glucose fasting test
B Glucose tolerance test
C HbA1c
D Urine testing
2 Which of the following statements about the blood pressure of a diabetic patient is true?
A Blood pressure has no influence on the risk of diabetic complications
B A target pressure of 140/85 mmHg is ideal
C Blood pressure should be monitored biannually
D Blood pressure is not an indicator of severity of diabetes
3 Which of the following is never appropriate in the management of type 1 diabetes?
A Smoking cessation advice
B Metformin
C Dietary advice
D Insulin
4 Which of the following inhibits release of glucagon?
A Insulin
B Gliclazide
C Metformin
D Sitagliptin
5 Which of the following may cause hypoglycaemia?
A Reduced insulin levels
B Sulphonylurea overdose
C Reduced metformin intake
D Excessive carbohydrate intake
6 Which of the following may be a side effect of metformin use?
A Roseate skin rash
B Diarrhoea
C Light sensitivity
D Coma