In the fifth article in our series looking at refraction, Tina Patel describes some variations on distance refraction including binocular assessment and assessment of those with high ametropia and reduced vision. Module C36775, one distance learning point for optometrists and dispensing opticians
So far in this series we have concentrated on objective and subjective techniques aimed primarily at gathering data from one eye at a time. There are many occasions, however, when it is beneficial to refract a patient in the binocular state. I will then finish this section on distance assessment with a look at the refraction of those with reduced acuity, those with communication or cognitive difficulties, and a brief discussion of the pinhole and the phoropter head.
Binocular refraction
Binocular refraction is the method of assessing the refractive error of the eyes without the use of an occluder. As mentioned previously in this series, a binocular refraction provides the most ‘normal’ viewing conditions, helps to relax accommodation by means of the ‘fogging’ lens used during the test and speeds up the routine, as there is no need to carry out binocular balancing.
Binocular refraction is not advised on patients whose acuities are unequal or one eye is strongly dominant.
Procedure for binocular refraction
? Following retinoscopy, check the visual acuity monocularly to ensure the visual acuity that has been attained is equal or almost equal in both eyes
? Inform the patient that you will be inserting a lens in front of one eye that will blur the distance vision slightly. Insert a +1.00DS lens in front of the right eye (left eye occluded) and ask the patient what the lowest line of letters is that they can read clearly. The visual acuity should blur back by three lines
? Repeat the ‘+1.00DS blur check’ for the left eye and ensure that blur back is to the same level. In the case of unequal acuities, refract the better eye first with the worst eye fogged
? Leave the +1.00DS lens in front of the left eye and remove the occluder from the right eye. Inform the patient that you have ‘blurred’ or ‘fogged’ the left eye intentionally but they should keep both eyes open during this test. Check that the patient is not experiencing diplopia before continuing. Stop the procedure if they report diplopia
? Determine the best vision sphere (BVS), and cylinder axis and power as for a monocular refraction
? Record the visual acuity in the right eye
? Remove the +1.00DS blur lens from the left eye and place it in front of the right eye. Repeat the procedure described above for the left eye
? Record the visual acuity in the left eye. If a marked change in the BVS or cross-cyl power has been made during the binocular refraction, the practitioner may wish to repeat the +1.00DS blur check at the end of the refraction to ensure that equal blur back is still evident
? Remove the fogging lens from the right eye and record the binocular visual acuity. Binocular balancing is not required as it can be assumed that accommodative balance exists
? Binocular addition can still be checked at this stage to ensure that maximum plus can be given to the patient binocularly.
Refracting patients with reduced acuity
For patients with reduced visual acuity, simple adjustments can be made to the tests conducted during the subjective refraction. This helps the patient and practitioner appreciate and differentiate changes in lens power and acuity that may not otherwise be seen using the standard testing procedures for patients with normal acuity.
? Checking the vision/visual acuity
– Measure the vision/visual acuity of the poorer eye first to avoid the patient memorising the letters on the chart
– When vision/visual acuity is markedly reduced, consider using an alternative chart such as a logMAR (Figure 1) which provides a logarithmic progression for the assessment of vision. ‘Just noticeable differences’ may be recorded and a logMAR provides a greater number of larger letters for patients with poorer acuity
[CaptionComponent="2698"]
– Patients who cannot read the largest letters on the letter chart can be asked to move closer (where possible) to the letter chart for example to 3m for ease of recording the results
– Where a below expected measure of vision/visual acuity is seen, a pinhole disc may be used to determine if the cause is refractive or pathological. (See procedure for using a pinhole later)
– Where the vision/visual acuity is markedly reduced at the closest test distance, the following method of recording the vision can be followed:
- Counting fingers at distance specified (CF @ xm)
- Hand movements at distance specified (HF @ xm)
- Light perception only (LP)
- No perception to light (NLP).
? Determining the best vision sphere and cross-cyl
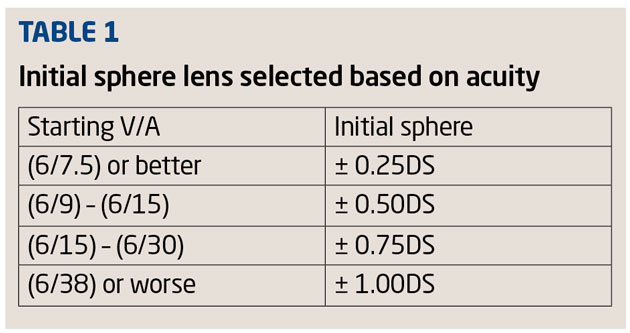
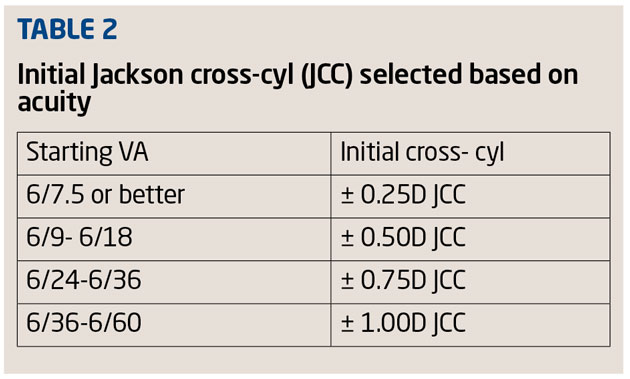
– Large dioptric changes in the sphere and higher-powered cross-cyls should be used to help the patient determine changes in the clarity of vision (Tables 1 and 2)
– Use a bracketing technique to aid the patient in differentiating a change in the lens power presented. The lens giving the better vision can be added and the technique repeated. As the vision improves, reduce the bracketing lens power
– For cross-cyl, use a larger letter on the letter chart relative to the patient’s acuity instead of the Verhoeff circles, which only provides good results with acuities of 6/12 or better
– Don’t carry out tests that are not necessary and will not provide useful or give a definitive end result, for example, the duochrome.
Refracting patients giving poor subjective response – confused, elderly and paediatric patients
To refine the measurement of the refractive error, subjective refraction relies heavily on active patient participation. There will, however, be a small group of patients where communication is limited or not reliable, for example, patients giving poor subjective responses, patients who become easily confused, elderly patients and children.
In all these examples, communication, simplifying the subjective routine and patience is key to ensuring the most accurate result is elicited.
? Use large dioptric intervals in lens power to help the patient discriminate changes in image clarity. Eg use ±0.50D JCC instead of ±0.25D JCC
? Simplify your questions during the refraction so as not to confuse the patient. Repeat the question in a different manner, simplifying it further, if the patient does not understand you or respond well the first time. Eg: ‘What is the lowest line of letters you can read on the letter chart?’ which may be simplified: ‘Can you see the line I am pointing to? Can you read this for me?’
? Don’t use scientific jargon or give complex descriptions of the test to be conducted, such as ‘I’m going to check the binocular status of your eyes’. Better to say: ‘I’m going to check how well your eyes work together’
? Reassure the patient that certain tests will give an expected result, eg ‘This lens will blur the letters on the chart but don’t worry this is quite normal,’ or ‘There is no right or wrong answer, just tell me what you see’
? Encourage the patient and help them to feel that they are doing well (but don’t patronise them). ‘What is the lowest line of letters you can read on the letter chart?’ might be said with encouragement: ‘That’s great you’re doing well! Can you read the line below; it might be tricky but have a go anyway’
? Be patient with the patient. A patient who is confused or elderly may become more confused, defensive or distracted if they sense your frustration at the lack of patient participation. Go slowly when needed and make the test choices easier for the patient.
? Boredom and fatigue can affect the subjective response. Carry out a routine that allows the patient to make choices but expect not to repeat them again and again to reach the ‘ideal’ end-stage result. Be quick but be methodical
? Use different test targets to elicit results
– Use a letter on the Snellen chart rather than the Verhoeff circles to perform cross-cyl in confused/poor responsive patients
– If possible, change the test type to pictures, numbers; letter ‘E’, letter ‘C’ if the patient is struggling with the standard Snellen type
– If a Sheridan-Gardiner test chart is not available, write the letters from the test chart on paper for the patient to point to instead of reading out
? Make the tests enjoyable and fun when refracting a child. Use targets/pictures that are recognisable, colourful and stimulating (Figure 2)
[CaptionComponent="2699"]
? Be prepared to change your working distance and adapt your test and results accordingly. An elderly patient in a wheelchair will most likely not be tested at the standard 6m distance
? For children, be prepared to carry out the refraction without the trial frame fitted; the child may not be comfortable wearing one or perhaps it simply does not fit them. The child may need to sit on the parent’s lap to help them feel more comfortable and reassured
? Don’t be afraid to get help. Where necessary, use the parent/guardian/carer of the patient to encourage, translate, entertain and communicate with the patient during the refraction.
Refracting patients with high refractive errors
When refracting patients with high ametropia, special consideration and adjustments need to be made during the refraction to obtain the most accurate results possible.
? Checking the vision/visual acuity
– Patients who cannot read the largest letters on the letter chart, can be asked to move closer to (where possible) to the letter chart for example to 3m for ease of recording the results
? Determining the best vision sphere and cross-cyl
– Large dioptric changes in the sphere and high-powered cross-cyls should be used to help the patient determine changes in the clarity of vision
– Use a bracketing technique to aid the patient in differentiating a change in the lens power presented. The lens giving the better vision can be added and the technique repeated, reducing the lens power as the vision improves
? Record the back vertex distance
– The back vertex distance is defined as the distance between the back surface of the corrective lens and the front surface of the cornea. The back vertex distance is recorded in high ametropic prescriptions usually taken as >±4.00DS at the time of the refraction so that any spectacles that are dispensed are fitted as close as possible to the lenses used at the time of the refraction.
The pinhole
The pinhole can be used to detect if a reduction in vision/visual acuity is refractive or pathological in origin. The pinhole disc admits only central rays of light that do not need to be refracted by the cornea or lens to fall to a point on the retina as opposed to a circle of blur. If a patient’s visual acuity improves by two or more lines with the pinhole, a refractive error is most likely present, and refraction should be performed before any further testing. If the acuity is not improved with pinhole evaluation, it is likely that the cause of the decreased visual acuity is not refractive, and further ophthalmologic evaluation is indicated.
Procedure for using pinhole
? Position the patient with their corrective lenses in place (if corrective lenses are worn). Explain to the patient that you will be placing a small pinhole in front of the eye being checked
? Occlude the eye not being tested and ask the patient to read the lowest line they can read clearly on the letter chart
? Position the pinhole in front of the eye being checked and ask the patient to look through the pinhole at the distance letter chart
? Instruct the patient that they may need to adjust their head position slightly to view the chart through the pinhole
? Ask the patient if they can read any more of the letters on the chart below the clearest line they read previously without the pinhole
– If a patient is confused or unsure of the test procedure, remove the pinhole and ask them to re-read the clearest line of letters and then replace the pinhole to repeat the process described above
? If an improvement in the vision/visual acuity is seen, an uncorrected refractive element can be suspected and the subjective refraction rechecked
? Record the results of the pinhole test following the visual acuity recorded eg VA 6/12, PH 6/12 or No improvement in pinhole (NIPH).
The phoropter vs trial frame
[CaptionComponent="2700"]
Compared to the trial frame, the use of the phoropter and its automated form has increased in popularity in optometric practice for conducting a subjective refraction. Choosing which to use will be dependent largely on the patient, their mobility, their communicative ability and subjective reliability.
The phoropter
Advantages
? Provides a quicker refraction, due to speed of presentation of trial lens contained within the unit
? Easier to conduct the bracketing technique
? Lightweight in the case of high and complex prescriptions requiring several lenses in a trial frame
? Lenses do not become dirty
? Binocular function tests can be checked easily
? Appeals to patients who like modern/computerised equipment.
Disadvantages
? Vertex distance inaccuracy for high prescription
? Uncooperative and low vision patients may experience discomfort, moving their heads back and changing vertex distances
? Psychologically off-putting – patient does not see change in lenses or what the practitioner is doing.
? Patient and practitioner can’t see each other’s faces – this may cause problems with those with a hearing impairment or those of an anxious disposition
? Elderly patients my have difficulty being aligned behind the phoropter
? Proximal accommodation.
[CaptionComponent="2701"]
[CaptionComponent="2702"]
The trial frame
Advantages
? More reliable in low vision patients who may tend to rely on eccentric viewing
? Better for carrying out over-refractions on bifocal/multifocal CL patients
? Patients who present with large ametropias (particularly astigmatism)
? Enhances accurate vertex distance in patients with high refractive errors
? Allows for the presentation of greater increments in lens power compared to a phoropter.
Disadvantages
? Uncomfortable
? Lenses become dirty/smudgy
? Increase in weight with the addition of several lenses
? Limited space to add lenses in high refractive errors.
The next part in this series will focus on near vision assessment and measurement.
? Tina Patel is an optometrist working in hospital and private clinics and is an examiner and assessor for the College of Optometrists
Model answers
(Correct answer is in bold text)
1 For which of the following patients would binocular refraction be unlikely to confer a distinct advantage for accuracy
A Low latent hyperope
B Child aged 12
C Young adult with accommodative spasm
D Bilateral pseudophake
2 Which of the following regarding the unilateral blur used in binocular refraction is true?
A It should be around one line of blur
B Uneven amounts of blur mean that binocular refraction is not possible
C It renders post-refraction binocular balancing obsolete
D It may help when refracting a patient with diplopia
3 Which of the following statements regarding a logMAR chart is true?
A The 1,0 line is easier to see than the 6/60 Snellen equivalent
B It allows for equivalence of target resolution requirement at varying working distances
C It is only available as a handheld chart as it is for use at different working distances
D logMAR charts all require a patient to know the alphabet
4 For a patient with distance acuity of 1.02logMAR, which might be the best first choice of Jackson cross-cyl?
A +/- 0.25 D JCC
B plus/minus 0.50D JCC
C plus/minus 0.75D JCC
D plus/minus 1.00D JCC
5 Which of the following assessments would best be done with a trial frame as opposed to a phoropter head?
A Binocular refraction
B Comparison of previous prescription with new prescription
C Assessing impact of small cylinders increase
D Over-refraction of a centre near multifocal contact lens
6 What might be indicated by a decrease in acuity with a pinhole?
A Residual uncorrected sphere
B Early maculopathic changes
C Residual cylinder after corneal surgery
D Impact of light scatter by media