Once the general type of correction has been established, single vision, progressive etc, we can begin to consider the lens design, material and form. Although lens selection was discussed in Parts 7, 8 and 9, it is necessary to stress the importance of considering spectacle lenses and frame as a whole, and not as individual components. In the author’s opinion it is important that practitioners can visualise the appearance of the finished appliance before it is ordered. Optical technicians are usually better at this than dispensing opticians and optometrists, so develop good working relationships with your laboratory and speak to the technicians who are working with the lenses. Practices that employ remote edging devices have the advantage of being able to visualise the appearance of the lens on-screen.
Lens centration
As professionals, patients expect us to take the appropriate measurements in respect of the lens type being dispensed to ensure they obtain comfortable visual performance from their spectacles. It also helps to avoid unexpected delays when the laboratory has to refer back to the practice to obtain additional information, especially if a measurement was not initially taken.
The two most important measurements for consideration are those of horizontal and vertical centration. Correct centration ensures that the area of the lens where the prescription is most effective is placed at the optimum point for the individual patient. In addition, correct centration minimises the visual problems, which may arise from unwanted differential prismatic effects in the case of anisometropia, and goes some way to reduce the annoying effect of unwanted reflections from the surfaces of the lens and the creation of ghost images.
Horizontal centration for distance vision
If a spectacle lens is correctly centred, we presume that the optical axis will coincide with the visual axis (a line joining the object and the fovea) of the patient. This means that there will be no prismatic effect experienced by the patient when viewing through this point on the lens. There are various and well known methods of determining the horizontal centration requirements for a patient which depend upon us making several assumptions about the complexities of the eye’s optical system. We assume that the distances between the eye’s visual axis, the eyes’ centres of rotation, the pupil centres and centration points on the spectacle lens (in the spectacle plane) are the same. This assumption allows us to measure the inter-pupillary distance (PD) in the traditional way using a millimetre ruler (Figure 1).
[CaptionComponent="2703"]
It is worth pointing out that the distance PD is a facial measurement. However, when this measurement is transferred to the appliance (lens) it is known as the centration distance (CD). As an example, a
subject may have a binocular distance PD of 60mm (30mm in each eye). This would be ordered as a distance centration distance of 30mm in both eyes. When measuring a subject’s distance PD using a millimetre ruler, either the pupil or the pupil/iris margin can be used as the ‘zero point’ in the determination of this measurement. A word of warning if the iris/pupil margin is being used as opposed to the pupil centre, as anisocoria (unequal pupil diameters) will produce an incorrect measurement and most subjects will of course display a small degree of anisocoria. When using a simple millimetre ruler another error that can occur is when the practitioner’s PD is very different to the subject’s. The generally accepted methods of measuring the PD are:
- Using a millimetre ruler
- Using a pupilometer
- Marking the pupil centres using dummy lenses or tape
- Using digital measuring devices.
Figure 2 illustrates horizontal centration for distance vision.
[CaptionComponent="2704"]
The near horizontal centration distance
As already mentioned, when recording the PD for distance vision, we are assuming that the eyes are fixating on a distant object and that the visual axes are parallel. When the eyes converge to view a near object we are not particularly interested in the distance between the pupil centres of the converging eyes. Of more importance is where the converging visual axes of the right and left eyes meet the spectacle plane. The distance between these two points is known as the near centration distance (NCD). The NCD is usually less than the near PD (the distance between the pupil centres in near vision). The NCD for a particular patient depends on the PD for distance vision, the position of the spectacle plane measured from the eye’s centre of rotation and the near object distance. In practice, one either measures the NCD directly, or one can determine it from a table of interpupillary distances (PDs), and working distances (Table 1).
When measuring the NCD of a subject using a millimetre rule, the practitioner must ensure that the subject is wearing a spectacle frame so that the measurement is taken in the spectacle plane (Figure 3).
[CaptionComponent="2705"]
The practitioner’s left ‘object eye’ lies centrally in front of the patient’s nose at the agreed working (reading) distance (Figure 4).
[CaptionComponent="2706"]
From Figure 5, it is evident that the NCD is dependent on the distance PD, working distance l, and the fitting distance s, as shown in the formula:
NCD = PD x l/(l + s)
which is simply derived from similar triangles in the figure and can be used to calculate the NCD for a patient.
Decentration for near vision is designed to allow the eyes to look through the optical centres at the fixation point as shown in Figure 5, and assuming equal powered right and left lenses, to experience zero horizontal differential prism when looking at other object positions.
[CaptionComponent="2707"]
Vertical centration
The subject of vertical centration is often ignored when dispensing single vision spectacle lenses. It is, hopefully, well known that the vertical positions of the right and left centres have to be the same or vertical differential prismatic effects will be induced. What is sometimes forgotten is that the optical centre should be correctly placed to agree with the pantoscopic tilt, or vice versa.
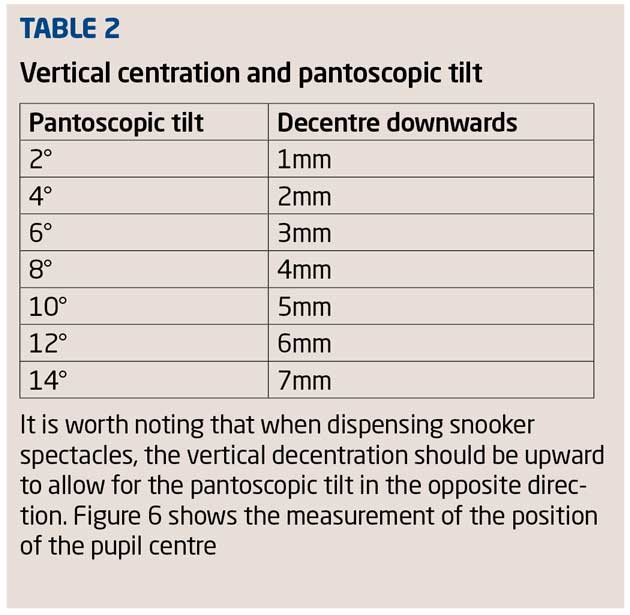
The pantoscopic tilt is only the same as the angle of side if the line of the side of the spectacle frame is horizontal. As previously mentioned, it is important to place the optical centre so that the optical axis of the lens passes through the eye’s centre of rotation. This single factor determines the optimum performance of the lens in all positions of gaze. Horizontal centration for distance vision is determined by the measurement of the PD for distance vision. The correct vertical centration depends on the amount of pantoscopic tilt. It can be easily shown that correct vertical centration requires the optical centre to be decentred by approximately 1mm for every 2° of pantoscopic tilt (Table 2).
If, as it usually is, the frame is tilted towards the face at the lower rim the optical centre must be placed below the pupil centre with the eyes in the primary position. Manufactures of aspheric lenses have always insisted that this type of lens be correctly centred vertically as well as horizontally, although vertical centration should be applied to all lenses. Incorrect vertical centration has the effect of making a spherical lens behave like an astigmatic lens. In other words, incorrect vertical centration will produce an unwanted sph/cyl effect.
In conclusion, for single vision lenses, the general guidelines are:
- Measure the distance PD to determine the horizontal centration requirements. Specify monocular centration distances if the monocular PDs are unequal
- Determine the vertical centration by using the pantoscopic tilt of the required frame. This applies to both lenses for distance and near vision
- For near vision, centration should match the near centration distances.
Useful terms relating to centration are defined in Table 3.
Centration of bifocals
When dispensing bifocals, as well as taking the factors that apply to single vision into account, we must also consider the following points:
- Segment type and size of any previous bifocal segment if worn as this can affect the field of view, centration, jump and cosmesis that the patient has become accustomed to
- Segment fitting height in previous bifocals if worn
- If only one bifocal lens is to be dispensed (the other lens remaining unchanged) the segment drop (distance from the optical centre of the distance portion to the segment top) should be specified to avoid unwanted vertical differential prismatic effects.
For new wearers the accepted fitting position for the segment dividing line is taken as being level with the lower limbus (Figure 7), before any adjustment for pantoscopic tilt is allowed for. As mentioned above, for existing wearers it is vital to establish the existing fitting height in their previous spectacles and to only consider changing this with good reason and the full support of the patient.
Positioning of the segment dividing line is generally made in relation to the horizontal centre line of the frame using a millimetre ruler. This is known as the segment top position. It is also acceptable to specify the position of the dividing line in relation to the lowest point in the lens edge. This is known as segment height. Horizontal centration of bifocals is somewhat more restricted due to the fact that the nature of lens manufacture results in most bifocal lenses having pre-determined insets in the region of 1.5 to 2.5mm in each eye. In practice, bifocal lenses tend to be ordered with reference to distance centration rather than near.
Progressive power lenses
Due to the vast range of progressive power lenses (PPLs) now available many practitioners tend to dispense a small range of lens designs and draw on previous experience within these ranges when recommending lenses to a patient. Although there is nothing wrong with this approach, providing there is a good representative cross-section of designs, it is essential that one also keeps abreast of new developments and the additional measurements required when ordering some lens designs.
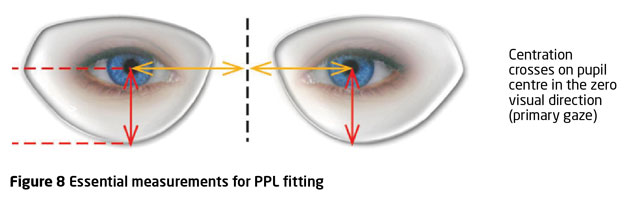
As with bifocals, the horizontal centration of PPLs follows the same basic principles as single-vision lenses in respect of measuring the inter-pupillary distances. When ordering a PPL, it is usual to specify the vertical and horizontal position of the fitting cross (Figure 8). Unlike bifocals, the vertical centration of PPLs usually requires the fitting cross be aligned with the pupil centre, the measurement being taken with reference to the HCL or the lowest point on the lens edge.
When dispensing traditional PPLs an average pantoscopic tilt of 8-10° is normally allowed for within the lens design and so no adjustment is needed in this respect. However, previous fitting heights should always be considered when refitting existing wearers and duplicated wherever possible in new spectacles to avoid the risk of non-tolerance.
When monocular measurements reveal a high degree of unequal convergence, or when shorter than normal working distances are required, one can consider specifying an individual, freeform design.
Individual lens designs
With the development of freeform surfacing, the realisation of unique, individual lens designs has become a reality. Using wavefront computer modelling systems, freeform designs take into account optics-influencing variables and the wearer’s physiological viewing habits way beyond the usual elements of just the optical prescription. To achieve the desired results additional measurements and information are often required by the manufacturer. These are now well known to most practitioners and can be summarised as follows:
- Monocular distance CDs
- Monocular near NCDs
- Vertex distance
- Pantoscopic tilt
- Face-form angle
- Near working distance
- Was a trial frame or a phoropter used?
- Trial frame orientation (where is the addition placed in the trial frame?)
- Specific lifestyle information, vocation, hobbies etc
- Previous type/brand of lens worn.
As the availability of these new lens types becomes more prevalent, practitioners need to familiarise themselves with the extended specification required when ordering these products.
Occupational lenses
Lenses intended for use in the workplace can be broadly divided into three groups:
- Vocational bifocals/trifocals. Normal lens designs fitted differently or with modified additions to allow for specific vocational activities
- Occupational progressives which are designed to maximise the field of view at various working distances
Degressive near vision lenses which are designed to provide only intermediate and near vision.
When faced with dispensing any type of occupational lens it is vital that a visual task analysis is carried to determine the range of clear vision, field of view and specific working distances required by the wearer. For bifocals or trifocals it may be necessary to lift the segment so that the wearer can easily glance at closer objects. Measurement is taken again from the HCL or the lowest tangent and it is always worth writing on the order that you have specified a special height for vocational use. Generally occupational progressives are fitted in a similar way to standard PPLs, positioning the fitting cross at the pupil centre. Degressive lenses, however, differ greatly in the range and type of measurements required so it is important to consult the manufacturer’s literature (or ABDO’s Ophthalmic Lens Availability) when ordering these products.
Ordering
Once the frame and lenses have been selected, any initial setting up carried out and all relevant measurements taken, all that remains is to prepare the order ensuring that it conforms to current standards. The format for such orders is well known but there are several points worth noting with respect to ordering and record keeping:
- Describe carefully any changes that you want a laboratory to make to the specification of a spectacle frame
- If an intermediate addition has been calculated, the working distance for which the addition is intended should be recorded on the patient’s records
- Ensure that the manufacturer, lens brand name, refractive index or relevant brand name and coating all relate to the intended lens supplier. For example, don’t order a Hoya coating on an Essilor lens!
- Ensure that if you are requesting an unusual centration or fitting height that you enter a note to this effect on the order.
Although the information required in an order may remain the same, the format in which orders are sent can vary greatly from hand written or telephone ordering to network programs and online ordering facilities. Practitioners should wherever possible familiarise themselves with all methods, especially those used for individual lens designs.
Further reading
Fowler C and Latham Petre K (2001). Spectacle Lenses: Theory and Practice Butterworth Heinemann Oxford UK.
Jalie M (1984). Principles of Ophthalmic Lenses 4th edition The Association of British Dispensing Opticians London UK.
Jalie M (2008). Ophthalmic Lenses & Dispensing 3rd Edition Butterworth Heinemann Oxford UK pp 75-87.
Norville Optical (2012) Prescription Companion.
Ophthalmic Lens Availability (2014). ABDO London UK.
Tunnacliffe A H (2003). Essentials of Dispensing, 2nd Edition ABDO.
Andrew Keirl is an optometrist and dispensing optician in private practice, associate lecturer in optometry at Plymouth University, ABDO principal examiner for professional conduct in ophthalmic dispensing, ABDO practical examiner and external examiner for ABDO College
Model answers
(The correct answer is shown in bold text)
1 When dispensing high plus powers which of the following is not a reason for keeping the vertex distance as small as possible?
A To maximise the field of view
B To reduce the retinal image size
C To reduce convergence demand
D To reduce the centre thickness of the lens
2 Which of the following is not a reason for correctly centring a spectacle lens?
A To position the lens where the paraxial prescription is most effective.
B To reduce unwanted differential prismatic effects.
C To control the centre thickness of the lens.
D To reducing the possibility of the formation of ghost images.
3 Which of the following lenses is bi-aspheric in form?
A Zeiss Lantal
B Hoya Nulux EP
C Essilor Lineis
D Hoya Nulux
4 When dispensing for high myopia and assuming that all other parameters are equal, which of the following products is likely to produce a lens with the thinnest edge substance?
A Essilor Lineis
B Hoya Eyry
C Zeiss Tital
D Zeiss Lantal
5 Which of the following statements is most correct?
A The Super Lenti lens is available in both resin and glass materials.
B The use of high refractive index materials will always result in a heavier finished lens.
C The Rodenstock Lentilux lens is manufactured using a resin material.
D When dispensing medium to high plus lens, the uncut size used is of no consequence.
6 Which of the following statements is most correct?
A If a high powered plus lens with a spherical back vertex power is manufactured with a convex prolate ellipsoidal surface, aberrational oblique astigmatism will be reduced.
B If a high powered plus lens with a spherical back vertex power is manufactured with a convex prolate ellipsoidal surface, both aberrational oblique astigmatism and distortion will be reduced.
C Ring scotoma and the Jack-in-the-box effect are not eliminated with polynomial aspheric designs.
D The lens of choice for a high powered plus lens of spherical back vertex power is one that incorporates an atoroidal surface.