In Part 6 of this CET series we looked at the method of choosing a reading addition appropriate to the patient’s age. There are several factors that have an influence on this choice, not least the current reading prescription of the patient and their residual level of accommodation. This article will describe how these are incorporated into the routine evaluation of the patient and then take a look at some further techniques it is useful to be aware of and which are adopted, in variable importance, throughout optometry.
Patient’s previous prescription
Patients presenting with an existing prescription for spectacles (distance or already incorporating a reading addition) from a previous eye test will often complain of a deterioration in their near sight with these, or of having to increase their working distance. More interestingly, patients may express a deterioration of their near sight without spectacles but report good near vision if the spectacles are worn. In both instances the near addition should be checked to ensure there hasn’t been a change in its required power. Also one should look for a change in the distance refraction that might be impacting on the near vision (for example an increase in hyperopia and myopia). The best technique for this is as follows:
? Ensure the distance refractive error has been checked and fully corrected
? Place the reading addition taken from the previous prescription or spectacles in the trial frame. If the patient only has single vision reading spectacles and no distance spectacles, use the results found from the distance refraction and patient’s age as a guide to selecting the reading addition. For example, if the previous near Rx is +1.00/-0.50x 90 and the age 53, and the distance refraction is found to be -0.50/-0.50x90, then the predicted addition based on age is +2.00DS (with the implied previous addition being +1.50DS)
? Ask the patient to hold the near vision chart at their preferred working distance
? Carry out the procedure as described in ‘prescribing by age and working distance’ in Part 6 (18.07.14).
In the absence of an old prescription or any distance refraction details, any change between the new and old reading spectacles will only be determined by comparing the difference between the sum totals of the reading prescription (the distance refraction plus the near addition).
Demonstrate to the patient any change found in the prescription, ensuring the working distance and range are within acceptable limits and the patient is happy with this.
Addition as a proportion of the amplitude of accommodation
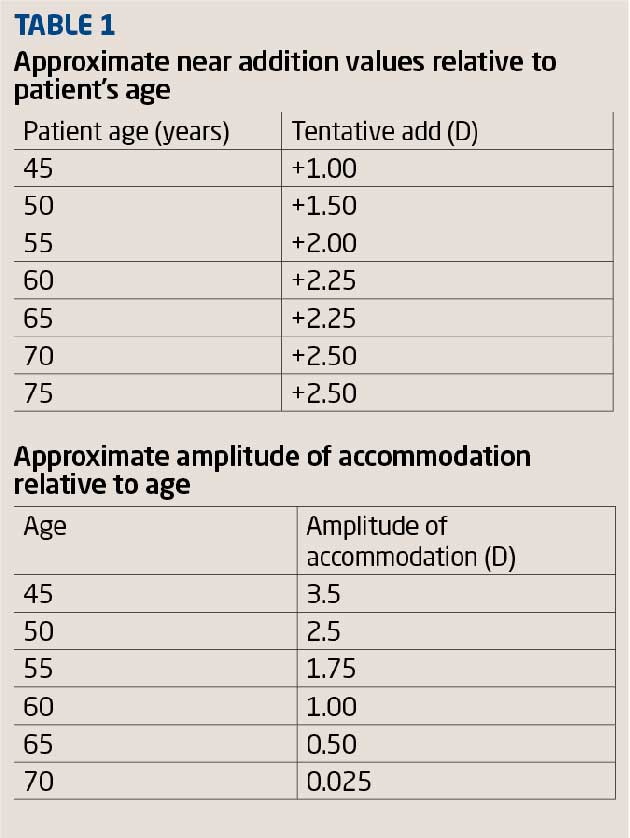
The amplitude of accommodation reduces with age. Measurements can range from approximately 10DS at age 20 reducing to 4.50DS at age 40 (Table 1). Values can vary depending on depth of focus, poor general health and medication. Measuring the amplitude of accommodation will give an indication of the patient’s accommodative ability and range of clear vision and serve as a starting point for determining a near addition.
? Measure the amplitude of accommodation monocularly then binocularly: ‘Push-up/push-down’ method using the RAF ruler (Figure 1). With the patient wearing their habitual distance correction, rest the RAF rule against the patient’s cheek. Push the near type target furthest away from the patient and ask them to view the clearest line of words/letters they can see comfortably. Move the target slowly towards the patient and ask them to inform you when the words/letters first become blurred. Ask the patient if they can make the words/letters clear again, if they can, continue to move the print closer to the patient until the print is permanently blurred. Note the amplitude in dioptres. Now push the target away from the patient and ask them when it first comes in to focus, repeat this to ensure the results are consistent. The amplitude of accommodation is determined by taking an average of the two values noted with the ‘push up and push down’ method. Take the reading from the side of the RAF rule, measured in dioptres. If the patient is unable to see the near target clearly, a supplementary addition lens can be added to the distance correction to improve the clarity of the near target and the test carried out as described. However, the final result will need to be adjusted to allow for the supplementary lens. For example if a +1.00DS supplementary lens is used, and amplitude measured as +5.00DS, then the actual amplitude is +4.00DS. Because this binocular test simultaneously changes the accommodation and convergence demands, the test is best done monocularly.
An alternative method is the ‘minus lens to blur’ method. Minus lenses are added over the distance correction monocularly until the distant target appears to be blurred, while the target distance is kept constant. This method changes the accommodation demand, but the convergence demand remains constant at distance.
[CaptionComponent="2724"]
? Various recommendations have been made to determine the initial addition from the measured results of the amplitude of accommodation. As a rule of thumb, the patient should be able to maintain up to half or two thirds of their amplitude of accommodation. Therefore the reading addition equals the working distance in dioptres minus two thirds or a half of the amplitude of accommodation in dioptres
? Using the initial addition calculated, carry out the procedure as described in Part 6 (18.07.14)
? This method can be less reliable in older patients, say over 55, due to age-related pupillary miosis which causes an increase in the depth of focus.
Balanced range of accommodation
Another method of prescribing the near addition is to place the dioptric midpoint of the range of clear vision at the patient’s normal near working distance. This midpoint is calculated by measuring the negative relative accommodation (NRA) and positive relative accommodation (PRA). NRA is a measure of the maximum ability to relax accommodation while still maintaining clear, single binocular vision of a test object at a specified distance. PRA is a measure of the maximum ability to accommodate while maintaining clear, single binocular vision of a target at a specified viewing distance.
? With the distance correction in the trial frame, direct the patient to look at a near test chart binocularly. Ask the patient the clearest line they can just manage and add plus power lenses in +0.25DS steps until the line of letters become clear. The plus power lens first to allow this is referred to as the ‘tentative add’
? Now continue to add plus power lenses in +0.25DS steps binocularly until the patient is no longer able to read the small print on the near chart. The total positive lens power added is the NRA
? Remove the NRA lens power and, starting from the tentative reading addition, add negative lens power lenses in -0.25DS steps until the patient is no longer able to read the small print on the near chart. The total negative lens power added is the PRA
? The initial tentative near addition is then adjusted to become the final tentative near addition. The final tentative near addition is a lens that provides equality for the NRA and PRA. For example, an initial tentative addition is found to be +1.00DS. For this case:
Blur lens power for NRA is +2.00DS therefore the NRA is +1.00DS
(+2.00-+1.00)
Blur lens power for PRA is +0.50DS therefore PRA is -0.50DS
(+0.50-+1.00)
The final tentative addition is +1.25 (this equalises the NRA and PRA, as they would both be 0.75).
The change suggested by the NRA/PRA is the algebraic sum divided by two, in this case 0.50/2 which is +0.25DS
? Using the final tentative add, carry out the procedure as described in Part 6 (18.07.14).
Binocular cross-cylinder
This method is believed to determine the power that creates an appropriate accommodative demand at the reading distance. Performing this test binocularly usually results in less plus power being required to reach the end point.
? With the distance correction in place, occlude the left eye and ask the patient to view a cross-grid target at the patient’s near working distance with the right eye (Figure 2)
[CaptionComponent="2725"]
? Ask the patient if the vertical and horizontal lines on the target appear equally clear
? Place a cross cylinder lens power -0.25DC at axis 90° in front of the right eye. For older presbyopic patients where the expected addition is high +1.00DS to the distance prescription, for the near chart to seen more clearly
? Ask the patient which of the lines on the grid, horizontal or vertical, appear clearer. A presbyopic patient should report the horizontal lines appear clearer
? Add plus lenses in +0.25DS steps until the patient reports the vertical lines are just clearer than the horizontal lines
? Now occlude the right eye and repeat the above procedure for the left eye
? Remove the occluder from the right eye and, binocularly, reduce the plus power gradually in both eyes, asking the patient to report when both the horizontal and vertical lines appear equally clear
? The plus lens power now found represents the tentative addition
? Using the tentative addition power, carry out the procedure as described in Part 6 (18.07.14).
Prescribing unequal adds
For presbyopes, when checking the plus lens power to bring near print in focus, the final reading addition should be equal for both eyes. Occasionally, unequal adds may be measured and prescribed, for example in cases of amblyopia, accommodative lag, anisometropia or simply a very ‘fussy and particular’ patient. Before confirming the need for unequal adds, check that the near addition end points and distance binocular balance have been correctly tested. The power required for the unequal add, working distance and range of clear near vision should be checked monocularly and finally presented to the patient binocularly to ensure the near vision is comfortable binocularly.
Recording the results
The final prescription can be specified in two formats; either as the distance refraction plus the reading addition required for close work tasks, or as the final distance and reading prescription whereby the final near vision prescription is the sum total of the distance correction plus the near vision addition. The practitioner should select one format or the other and be consistent, so the prescription is not misinterpreted. Where an intermediate or occupational specific addition has been found, this should also be specified on the final prescription. Specifying the distance and near acuity and working distance and range will aid the dispensing practitioner. It will also help any optometrist testing the patient in future, and help establish what the expected levels of acuity should be with their new spectacles as well as any possible change in acuity subsequently found. Let us look at two different representations of the final correction
Example 1 – Distance prescription with near add
Distance Rx
R +2.00/-0.50 X 90 VA 6/6
L +2.50/-0.25 X 80 VA 6/6
Near add R and L +2.00 N5@ 40cm (range 35-55cm)
Intermediate add R and L +1.25 N6@ 70cm (range 50-75cm)
Example 2 – Distance prescription and intermediate/near prescription
Distance Rx
R +2.00/-0.50 X 90 VA 6/6
L +2.50/-0.25 X 80 VA 6/6
Near Rx
R +4.00/-0.50 X 90 N5@40cm
L +4.50/-0.25 X 80 N5@40cm
Intermediate Rx
R +3.25/-0.50 X 90 N5@70cm
L +3.75/-0.25 X 80 N5@70cm
Considerations for the management of presbyopia
Inappropriate assessment of the patient’s near vision prescription can be a common cause of patient dissatisfaction, leading to retests. Giving too much plus, incorrectly determining the patient’s working distance or not giving a reasonable range of near vision are among the commonest causes. Regardless of the method used to determine the near vision prescription, the goal is to provide the patient with clear, comfortable vision for their habitual visual tasks. An overview of prescribing considerations is provided below.
? Management decisions should be based on the results of the sight test as well as details of vocation and occupation, social requirements and any hobbies or specific visual tasks or demands
? Patients with early (incipient) presbyopia who do very little near work and are not experiencing any difficulties or discomfort will probably not require correction. Patients may be advised about the expected vision changes to come and how to compensate for the reduced accommodative ability, such as employing increased lighting or moving reading material further away. Always recommended an eye check as appropriate
? Beware of over-delaying prescribing the initial near correction. Unmanaged presbyopia can result in visual discomfort. Adaptation and adjustment after higher addition prescribing may be more difficult
? Check and double check the patient’s required habitual working distance and range. Common causes for retests are due to the patient’s and practitioner’s misinterpretation of their working distance and thus intolerance to reading spectacles (Figure 3). If possible ask the patient to measure their working distance and range requirements
[CaptionComponent="2726"]
? Beware of over-plussing the near correction
? Always demonstrate the change in any near vision prescription found. The patient should be clear about the effect that increasing the plus power will have on their working distance and range
? Beware of prescribing a change in near vision prescription that provides no visual change when compared to the previous prescription
? Beware of reducing the total plus power of the near correction. Age-related changes in distance refraction could influence the final prescription
? Beware of the loss of intermediate field when prescribing an initial near addition for the low-myopic presbyopia patient or when prescribing minus power at distance for the presbyopic patient undergoing a myopic shift in both eyes.
Summary
Although managing a patient with presbyopia by prescribing a reading addition for close work may seem easy, a host of factors need to be considered. Under-corrected or uncorrected presbyopia can cause significant visual disability and have a negative impact on the patient’s quality of life.
Gaining an understanding of the patient’s specific vocational and social visual requirements helps the optometrist recommend the treatment most appropriate for enhancing visual performance.
Advise the patient about presbyopia and how this ‘change’ is normal and expected at a certain time. Patients should be informed about the signs, symptoms, clinical course, and treatment options for presbyopia. Education at the time of the sight test and dispensing will help minimise adjustment problems. Information should be provided about the potential visual implications of alternative types of optical correction and their use.
First-time spectacle users can often be challenging cases, due to the psychological factors that remind the patient that he or she is getting older and that some functional abilities are decreasing as a result of ageing. Some patients find it extremely difficult to accept reading spectacles or multifocals and their implications.
? Tina Patel is an optometrist working in hospital and private clinics and is an examiner and assessor
Model answers
The correct answer is in bold text
1 What is the expected amplitude of accommodation for a 40 year old?
A 1.00DS
B 3.00DS
C 6.00DS
D 10.00DS
2 A patient uses the RAF rule with a +2.00DS supplementary lens. Print goes out and then back into focus at 18cm and 22cm respectively. What is their recorded amplitude of accommodation?
A 1.00DS
B 2.00DS
C 3,00DS
D 4.00DS
3 A visually impaired child has amplitude of accommodation of +18.00DS. What upper level of accommodation might be sustained to allow magnification through close working distance?
A 6.00DS
B 10.00DS
C 12.00DS
D 16.00DS
4 A patient with initial tentative addition of +2.00S has NRA of +0.75 and PRA of -1.25DS. What is the final tentative addition?
A 1.50DS
B 1.75DS
C 2.00DS
D 2,25DS
5 Which of the following statements about near cross-cylinder is true?
A It requires accommodation
B It is a monocular test
C It can only be done using a phoropter head
D It tends to give a lower addition if done binocularly
6 Which of the following might justify odd adds?
A Uneven accommodation with final distance correction
B Uneven pupils
C Unilateral proptosis
D Microstrabismus