Blepharitis, or inflammation of the lid margin, is a common cause of ocular discomfort and dry eye symptoms.1 This common affliction is observed by eye care practitioners (ECPs) in 37-47 per cent of patients.2 Symptoms, such as burning, itching, grittiness, and blurry vision, are non-specific and overlap with numerous other ocular anomalies, challenging ECPs to find the cause. Blepharitis is divided into two categories, namely anterior, involving the lid margin around the lashes, and posterior involving the more distal positioned meibomian glands. Recently, much attention has been devoted to posterior blepharitis or meibomian gland dysfunction (MGD) and its role in evaporative dry eye as reported by the Tear Film Ocular Society (TFOS) in 2011.3 Little, however, has progressed in the realm of anterior blepharitis which can also contribute to ocular discomfort.
Anterior blepharitis: staph or Demodex?
Anterior blepharitis is caused by an infectious agent and can be chronic or acute in nature.4 The causative agents can be bacterial (staphylococcal), fungal (yeast) or parasitic. Typical symptoms include sore, dry, burning eyes, usually bilateral, with periods of exacerbation. Patients also complain of sticky eyes upon wakening and are concerned about how red and ‘tired’ their eyes look. They report being overly frustrated with the chronicity of the condition, despite their compliance with lid hygiene and the temporary symptom relief that ocular lubricants provide.
Ocular signs of anterior blepharitis are comprised of hyperaemia, lid oedema and debris along the lash line. This may or may not be accompanied by corneal staining, depending on the severity of the condition. ECPs are quite familiar with the yellow crusty collarettes on the lashes of staphylococcal anterior blepharitis (Figure 1), but when the condition doesn’t improve with traditional lid scrubs and antibiotic treatment, one should consider other causes.
[CaptionComponent="2730"]
A detailed examination of the debris on the lashes may lead to a different diagnosis, often missed by ECPs. Clear, gelatinous, waxy debris that remains at, and surrounds, the base of the lashes, points to a parasitic infestation caused by the Demodex mite. Symptoms of persistent ocular discomfort,5 especially upon awakening and itching along the lash line, should direct the ECP to look at the base of the lashes more attentively.
Demodex
Demodex is a parasitic mite. Although many species exists in animals, only two are hosted by humans, namely D folliculorum and D brevis. The eight-legged transparent arthropod measures between 0.2-0.4mm in length (brevis being short) with a head and an opisthosoma (body-tail) (Figure 2).
[CaptionComponent="2731"]
The mite has a life span of three weeks, during which it can lay between 12-15 eggs to foster the subsequent generation. It is the most common ectoparasite (living outside the body) in humans affecting both sexes equally in 20-29 per cent of asymptomatic patients.6-8 The prevalence of the Demodex mite increases with age and can reach 100 per cent of people over the age of 70.9-10 Healthcare professionals, including medical students, have a higher risk of acquiring Demodex through direct contact with infected patients.11 In addition, the mite is a vector for bacteria such as Streptococci, Staphylococci, and Bacilus oleronius, creating opportunity for further inflammatory response.11-13
D brevis lives deep in sebaceous glands of the skin, including the meibomian glands, looking for sebum as a source of nutrition. D folliculorum resides in hair follicles including those of the nose, cheeks, ear, scalp, eyebrows and eyelashes.14 In the eye, Demodex pierces through follicular and glandular epithelial cells using its mouth, damaging the lid margin.15 Due to its suspected sensitivity to light,16 the mite buries itself headfirst into the lash fo
llicle and is not typically seen fully on the lash. The female mite remains in the follicle and the male counterpart moves between follicles, likely at night, to copulate. In fact, there could be up to six or eight mites in a single follicle.
Clinical presentation and diagnosis
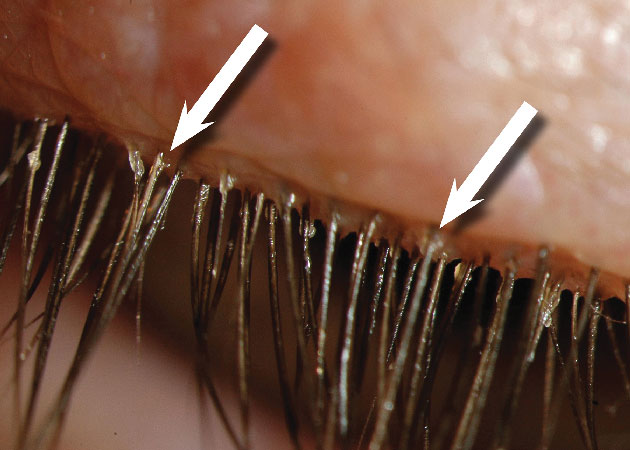
Itching, light sensitivity, tearing and overall ocular discomfort, are the most reported symptoms in patients with Demodex.5,7 Signs include inflammation of the lid margin, disorders of the eyelashes, MGD and corneal involvement, depending on the severity of the infestation. The most conspicuous indicator of the presence of D folliculorum is a clear waxy sleeve surrounding the base of the lash (Figure 3), commonly referred to as cylindrical dandruff (CD).17 CD is an accumulation of cellular debris, sebum and lipids, which create this waxy, greasy appearance.
[CaptionComponent="2732"]
This is in contrast with the dry, crusty collarettes typically found in staphylococcal blepharitis, in that they do not progress along the lash as it grows. Other noted differences of the clinical presentation of Demodex include, early morning ocular discomfort (as opposed to end-of-day dryness reported in dry eye) and itching along the lash line (to be differentiated from overall ocular itching commonly reported in allergies). The small size of the Demodex mite coupled with the fact that it buries itself in the follicle contribute to the reason why this diagnosis is often overlooked by ECPs during a routine slit-lamp examination. Furthermore, if the debris is not examined carefully, then it may be mistaken for a bacterial origin and inappropriate treatment may be dispensed.
Definitive diagnosis is confirmed upon microscopic observation of the mites using a low-grade light microscope (minimum 10X). Epilation of a lash, using flat head tweezers, is required and placing it on a microscope slide for observation. Adding a basic microscope to a clinical practice is inexpensive and can assist in positively identifying the presence of the mites. In addition, the direct observation of the mites by patients can be impactful in the education of the cause of their ocular discomfort and in the adherence to treatment. Since most ECPs do not possess a microscope in clinical practice, it has been suggested to pinch the desired lash and rotate it without epilating it.18 This movement seems to irritate the parasite and their tails will extrude further from the hair follicle, rendering them more visible under high magnification (at least 40X) on the slit lamp. Some practitioners19 have advocated simply initiating treatment when CD is observed in a patient with longstanding unresolving blepharitis.
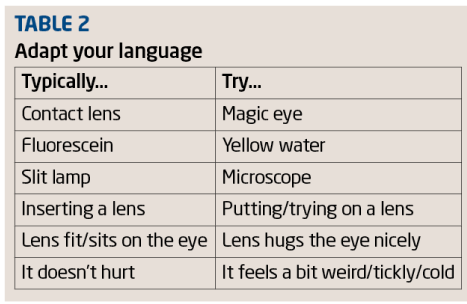
A severity scale has been proposed dependent on the density of the CD observed (Table 1).19
 Studies have reported a strong correlation between Demodex and acne rosacea,14,20 making them 7-8 times more at risk for Demodex. Substantial correlations with MGD and mixed blepharitis (both anterior and posterior) have also been noted.21 Immunocompromised patients,22-24 including those with eyelid basal cell carcinoma,25 have been found to present with increased mite densities. However, this has not been substantiated by others.7,26 Although the correlation between mite densities and clinical disease commands further investigation, it has been proposed that individuals with systemic diseases who are infested with Demodex may be more at risk for recurrent and amplified skin lesions.27
Studies have reported a strong correlation between Demodex and acne rosacea,14,20 making them 7-8 times more at risk for Demodex. Substantial correlations with MGD and mixed blepharitis (both anterior and posterior) have also been noted.21 Immunocompromised patients,22-24 including those with eyelid basal cell carcinoma,25 have been found to present with increased mite densities. However, this has not been substantiated by others.7,26 Although the correlation between mite densities and clinical disease commands further investigation, it has been proposed that individuals with systemic diseases who are infested with Demodex may be more at risk for recurrent and amplified skin lesions.27
Management
Left untreated, anterior blepharitis may lead to misdirection (trichiasis) or loss (madarosis) of lashes, thickened inflamed lid margins (tylosis), hyperaemia of the surrounding conjunctiva and corneal manifestations.9,28 Mite physiology warrants further investigation, but it is proposed that waste from digestion of cells and sebum is accumulated in intestinal sacs. At the end of its life cycle, the mite bursts, open spilling its contents on the ocular surface, increasing the bio-burden of the lid margin and the tear film.29 With nearly 100-150 lashes per eyelid,30 it may be impossible to eradicate all the mites, but one can attempt to limit infestation in an attempt to alleviate patient symptoms. Patient education as to the prevalence of Demodex, its associations with skin diseases and ocular discomfort is key in patient understanding of their condition and compliance with treatment.
Tea tree oil (TTO)-based treatments have proven to significantly reduce Demodex infestation in the eye.31-32 TTO is an essential oil that comes from the leaves of the Melaleuca alternifolia tree, which is native to Australia and possesses antibacterial, antifungal, anti-parasitic and anti-inflammatory properties.33 Consequently a regimen of TTO will not only target the mites, but any piggybacking bacteria.15 While pure TTO is irritating to the skin and ocular surface, several diluted products are commercially available in the form of lid scrubs, such as Sterilid eyelid cleaner (Theratears, Advanced Vision Research), Demodex Convenience Kit (Ocusoft), and Cliradex lid scrub (Cliradex).34-36 More recently,37 reports of the most active ingredient in TTO detrimental to Demodex is terpinen-4-ol, contained in Cliradex.
Treatment should persist for 4-6 weeks to eradicate both the mites and their eggs. Since transmission of the mites is by direct contact, an added strategy would be to avoid sharing face towels, change linens often (especially pillow cases) washing and drying them using a hot setting and to discard makeup in direct contact with the lid margin, such as mascara.38 It may be wise to check other family members as well and since Demodex resides in hair follicles all over the body, then a TTO-based shampoo and face wash may be recommended. Concomitant use of topical steroids should be avoided as this has shown to increase mite counts.39
ECPs should continually educate patients on preserving eyelid health to minimise ocular discomfort occurring from dry eye, allergies, anterior and posterior blepharitis and Demodex infestation.40 Given the propensity of eyelid disorders, reinforcing the notion of a healthy lid margin and tear film is crucial in maintaining good vision and supporting ocular tissue integrity.
Conclusion
Anterior blepharitis is a common problem of the lid margin, contributing to ocular discomfort, contact lens intolerance and eventual lid margin changes if left untreated. Careful examination of the type and placement of debris on the lashes coupled with symptoms of ocular discomfort may assist the ECP to better differentiate between staphylococcal and Demodex causes of anterior blepharitis and target treatment accordingly.
Case reports
Case 1: A 30-year old woman with a history of lupus and acne rosacea consulted for chronic dry eye (DE), severe ocular discomfort (ocular surface disease index-OSDI 67.5/100) and fluctuating vision affecting TV viewing and reading. Management included unpreserved tear lubricants, antibiotics and lid scrubs, which were ineffective at relieving her symptoms. A DE work-up revealed a tear film instability (TBUT 4-5secs), a hyperosmolar (>308mOsm/L) tear film (OD 322, OS 320 mOsm/L), a mild (grade 1) interpalpebral superficial punctate keratitis, mild MGD (grade 1), upper lid margin staining (ULMS grade 3) and significant anterior blepharitis (grade 3). A closer look at the blepharitis revealed that the deposits surrounding the base of the lash were CD (Figure 4).
[CaptionComponent="2733"]
Further probing revealed mild itching along the lid margin, especially in the morning. Epilation and microscopic observation of a lash containing CD revealed a mite attached to a lash.
The patient was educated as to the cause of her blepharitis and was shown the mite under the microscope. Initial therapy included TTO-based lid scrubs (Theralid, Theratears, Canada) with mild improvement to her symptoms (OSDI 65/100). Follow-up visits added lid scrubs containing 4-terpinol (Cliradex) for six weeks, which significantly improved her symptoms (55/100). Although still in the ‘severe’ symptom category the patient was pleased with the improvement. At the latest visit the patient reported periods of remission and exasperation whereby she adjusts the use of the lid scrubs with 4-terpinol accordingly. Unpreserved artificial tears continue to provide additional relief for her DE. The patient also reported an improvement in the redness of her cheeks, likely resulting from the use of prescribed lid scrubs on her closed eyelid and surrounding periocular area.
Case 2: A 24-year-old student consulted for a mild unilateral red eye with associated ocular discomfort. Visual acuity was unaffected and a brief history revealed recurrent episodes of blepharitis (2-3/year). Upon further questioning, she reported itching along the lash line, worse that morning. A comprehensive examination revealed no anterior or posterior segment anomaly other than a mild blepharitis with CD at the base of several lashes. Epilation and observation under a microscope confirmed the diagnosis. The patient was placed on lid scrubs containing TTO (Theralid, AVR) and her discomfort and redness improved considerably within two days.
References
1 Kanski JJ, Bowling B ed. Eyelids. Kanski and Bowling’s ed. Clinical Ophthalmology: A systematic approach. 7th edition. Elsevier Saunders, Edinburg p 34-8.
2 Lemp MA, Nichols KK. Blepharitis in the United States 2009: a survey based perspective on prevalence and treatment. Ocul Surf, 2009;7(Suppl 2):S1-S14.
3 Nichols KK, Foulks GN, Bron AJ, Glasgow BJ, Dogru M, Tsubota K, et al. The international workshop on meibomian gland dysfunction: executive summary. Investigative Ophthalmology & Visual Science, 2011;52(4):1922-9.
4 Carter K, Jones YJ. Eyelids. Gold DH Lewis RA ed. Clinical Eye Atlas, 2nd ed. New York: Oxford University Press. 2011:p20.
5 Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between Demodex and ocular Discomfort. IOVS, 2010;51:2906–2911.
6 Arici MK, Sumer Z. The prevalence of Demodex folliculorum in blepharitis patients and the normal population. Ophthalmic Epidemiology, 2005;12:287-90.
7 Kosik-Bogacka DI, Lanocha N, Lanocha A, et al. Demodex folliculorum and Demodex brevis in healthy and immunocompromised patients. Ophthalmic Epidemiology, 2013;20(3):159-163.
8 Galvis-Ramirez V, Tello-Hernandez A, Alvarez-Osorio L, Rey-Serranno JJ. The prevalence of Demodex folliculorum infection in patients attending a general ophthalmological consultation. Rev Salud Publica (Bogota), 2011;13(6):990-7.
9 Hom MM, Mastrota KM, Schachter SE. Demodex: Clinical cases and diagnostic protocol. Optom Vis Sci, 2013;90(7):198-205.
10 Kamoun B, Fourati M, Feki J et al. Blépharite à Demodex: Mythe ou réalité? J Fr Ophtalmol, 1999;22:525-7.
11 Wesolowska M, Knysz B, Reich A, et al. Prevalence of Demodex spp in eyelash follicles in different populations. Arch Med Sci, 2014; 10, 2: 319-324.
12 Lacey N, Delaney S, Kavanagh K, Powell FC. Mire-related bacterial antigens stimulate inflammatory cells in rosacea. Br J Dermatology, 2007;157:474-81.
13 Li J, O’Reilly N, Sheha H et al. Correlation between ocular demodex infestation and serum immunoreactivity to bacillus proteins in patients with facial rosacea. Ophthalmology, 2010;117(5):870-877.
14 Zhao YE, Wu LP, Hu L, Xu JR. Association of blepharitis with Demodex: A meta-analysis. Ophthalmic Epidemiology, 2012;19(2):95-102.
15 Liu J, Sheba H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol, 2010;10(5):505-510.
16 Coston TO. Demodex folliculorum blepharitis. Trans Am Ophthalmol Soc, 1967;65:361–392.
17 Gao YY, Di Pascuale MA, Li W et al. High Prevalence of Demodex in Eyelashes with Cylindrical Dandruff. IOVS, 2005;46(9):3089-3094.
18 Mastrota KM. Method to identify Demodex in eyelash follicle without epilation. Optom Vis Sci, 2013;90(6):172-4.
19 Schachter S. A different approach to treating demodex blepharitis. Optometry Times, 2014;January issue (URL:http://optometrytimes.modernmedicine.com)
20 Zhao YE, Wu LP, Peng Y, Cheng H. Retrospective analysis of the association between Demodex infestation and rosacea. Arch Dermatol, 2010;146:896-902.
21 De Venecia III AB, Siong RLB. Demodex sp infestation in anterior blepharitis, meibomian gland dysfunction, and mixed blepharitis. Phillipp J Ophthalmol, 2011;36(1):15-22.
22 Edmondson II, W, Christenson MT (1992). Lid Parasites. Clinical Optometric Pharmacology and Therapeutics, B. Onefrey. Philadelphia, Lippincott-Raven.
23 Pecorella I, Ciardi A, Maedsco A, Di Tondo U. Histological findings in the eyelids of AIDS patients. Acta Ophthalmol Scand, 1999; Oct;77(5):564-7.
24 Castanet J, Monpoux F, Mariani R, Ortonne JP, Lacour JP. Demodicidosis in an immunodeficient child. Pediatr Dermatol, 1997; May-Jun;14(3):219-20.
25 Erbagci Z, Erbagci I, Erkiliç S. High incidence of demodicidosis in eyelid basal cell carcinomas. Int J Dermatol, 2003 Jul;42(7):567-71.
26 Aydingöz IE, Mansur T, Dervent B. Demodex folliculorum in renal transplant patients. Dermatology, 1997;195(3):232-4.
27 Chen W, Plewig G. Human demodicosis: revisit and a proposed classification. Br J Dermatology, 2014;170:1219-25.
28 Kheirkhah A, Casas V, Li W, Raju VK, Tseng SC. Corneal manifestations of ocular Demodex infestation. Am J Ophthalmol, 2007;143(5):743–749.
29 Mackenzie D. Rosacea may be caused by mite faeces in your pores. New Scientist, 2012 (URL : http://www.newscientist.com/article/dn22227-rosacea-may-be-caused-by-mite-faeces-in-your-pores.html?full=true&print=true) accessed Aug 4, 2014.
30 Hart WM. The Eyelids. In Hart’s ed. Adler’s Physiology of the Eye, 9th ed. Mosby Year Book, St. Louis. 1992:p1-3.
31 Koo H, Kim TH, Kim KW et al. Ocular surface discomfort and Demodex: Effect of tea tree oil eyelid scrub in Demodex blepharitis. J Korean Med Sci, 2012;27:1574-9.
32 Gao YY, Xu D, Huang L, Wang R, Tseng SCG. Treatment of ocular itching associated with ocular Demodicosis by 5 per cent tea tree oil ointment. Cornea, 2012;31(1):14-7.
33 Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (Tee Tree) Oil: A review of antimicrobial and other medicinal properties. Clin Microbiology Reviews, 2006;Jan:50-62.
34 Sterilid eyelid cleaner, Theratears, Advanced Vision Research at http://www.theratears.com/sterilid.php (accessed on July 31, 2014).
35 Demodex Convenience Kit, Ocusoft at www.ocusoft.com/Dry-Eye-Therapy-DEMODEX-CONVENIENCE-KIT-P5321.aspx (accessed on July 31, 2014).
36 Cliradex at http://www.cliradex.com (accessed on July 31, 2014).
37 Tighe S, Gao YY, Tseng SCG. Terpinen-4-ol is the most active ingredient of tea tree oil to kill Demodex mites. Translational Vis Sci & Tech, 2013;2(7):1-8.
38 Roque MR et al. Demodicosis treatment and management. MedScape References, May 1, 2013 (URL: http://emedicine.medscape.com/article/1203895-treatment)
39 Dolenc-Voljc M, Pohar M, Lunder T. Density of Demodex folliculorum in perioral dermatitis. Acta Derm Venereol, 2005;85(3):211-5.
40 Benitez-del-Castillo JM. How to promote and preserve eyelid health. Clinical Ophthalmology, 2012 ;6 :1689-98.
Etty Bitton is an associate professor and the director of the Dry Eye Clinic at the École d’Optométrie, Université de Montréal. Samantha Kronish is a college student majoring in health sciences
Model answers
(Correct answers are in bold text)
1 Which of the following is the most conspicuous indicator of the involvement of Demodex foliculorum
A Hyperaemia of the lid margin
B Lash loss
C Clear, waxy sleeve around the base of a lash
D Corneal staining
2 Which of the following terms best describes Demodex folliculorum?
A Bacterium
B Amoeba
C Arachnid
D Virus
3 Which of the following statements about Demodex is true?
A It is the most commonly found parasite in the human body
B It has a three week life span
C It is more commonly found on males
D It is found on 100 per cent of people
4 Which of the following features of associated discomfort is characteristic of Demodex infestation?
A It tends to be significant upon waking in the morning
B It is much greater than the clinical signs might lead one to expect
C It increases toward the end of the day
D It is sufficient to disrupt sleep patterns
5 Which of the following has the strongest association with Demodex?
A Acne vulgaris
B Acne rosacea
C Contact dermatitis
D Psoriasis
6 Which of the following statements about Demodex management is false?
A Treatment should continue for 4 to 6 weeks
B Treatments ideally should include terpinen-4-ol
C Topical steroids may complement treatment with tea tree oil
D Hair and body washes should be considered