How we deal with missed appointments varies. They may be a chance to catch up, to grab a cup of tea during a busy clinic or write a referral letter but the bottom line is that missed appointments cost money and interfere with the smooth running of a clinic. Furthermore, it is important to understand reasons why patients do not show as this may help reduce future no-show impact and also possibly have implications for future ongoing and consistent care of patients.

Background
In the past missed appointments may have just been annoying and something that was left to the support staff to deal with. However, with the advent of shared care and referral refinement, the need for follow-up tests such as repeated field and pressure measurements has clinical relevance too. Indeed, attendance for appointments bears some reflection of patient compliance and might usefully influence future management options.
Missed appointments are not unique to optometry. The NHS recorded a no- show rate of 9% for outpatient appointments in English hospitals for December 2016.1 A figure that has been remarkably consistent across all branches of the NHS and in the year 2014/15 translated to 5.6 million missed appointments.2 Although exact figures are difficult to measure, the National Audit Office estimated that in 2012/13 this cost the NHS £225 million.3
Figures published by the General Optical Council show that 21.1 million eye examinations were conducted in 2011. If the failed-to-attend rate within the NHS is generalised to optometry, a 9% no-show rate would equate to nearly two million missed appointments at a cost in excess of £40 million in eye examination fees alone.
Dentistry has also looked at the problem.4 In 2010, the British Dental Association (BDA) invited dental practice owners in England to participate in a review. The responses that they received represented more than 150 dentists working in 59 different practices. Each practice that participated submitted a report covering a 12-month period detailing the number of appointments that were missed and the hours of work that this represented. Although the mode of practice in dentistry differs from that in optometry, with differing recall periods and treatment regimes it is still worth considering the results. The findings were startling, with each full time equivalent dentist having 360 missed appointments a year. There was also a correlation between the amount of NHS work that the practice undertook and the number of missed appointments, with a larger number of missed appointments in practices which had a greater NHS commitment.

Reasons for No Shows
A number of studies have been conducted within Primary Care in the NHS. Neal et al5 reported on the causes for missed appointments. They interviewed patients who had missed appointments. Most respondents reported a multifactorial cause, but the greatest single quoted reason was that they ‘simply forgot’, with difficulty cancelling the appointment or the inconvenience of the time or location of the appointment being mentioned in about a third of cases. They also reported that 91% of the patients who failed to attend did consult within the next three months, and over half of them within three weeks. The results are summarised in table 1.
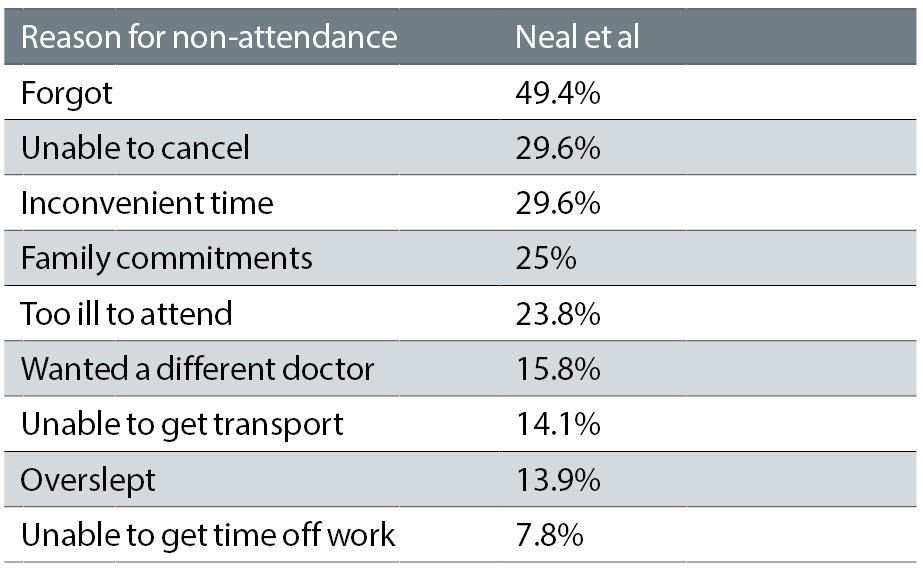
Table 1: Reasons for non-attendance 5
When considering missed appointments, George and Rubin6 make a valid point about the use of an appointment system. They reviewed a study detailing attendance profiles at booked appointments and open ‘drop in’ clinics and one theme that recurred was that people who miss appointments have a less predictable, more chaotic lifestyle. This was not a critical judgement but a reflection of their lived experience. It identified single mothers with children, whether the children accompanied them or not, and people with other social problems as more likely to have difficulty with an appointment system. They also identified the reliance on public transport and its unreliability as a factor in missing or keeping appointments.
Another interesting fact was that the no-show rate was highest on Mondays and lowest on Fridays, though this was a hospital-based study and may differ in a primary care practice based.
Consequences of missing appointments
As optometry becomes more involved in shared care and referral refinement schemes, the consequence of missed appointments becomes more important. The medicalisation of our profession, and its assumption of an increasing secondary care role with the management of chronic conditions, makes it more likely that patients will have a series of appointments. It also makes attendance at these appointments more important for patient outcomes and on-going care.
Attitudes to missed appointments
Martin et al 7 were interested in the attitudes of both the practice team and patients towards missed appointments. They conducted a series of semi-structured interviews to explore these themes. There were differing attitudes from the primary care practitioners and the reception staff towards missed appointments. GPs seemed to have ambivalent attitudes towards non-attendance, they were willing to make allowances for people with chaotic lives recognising the difficulties they had and even welcoming the time that a missed appointment gave them to catch up on administration. However, they felt that those who were ‘reckless’ about keeping appointments were blame-worthy. Interestingly, the GPs had a more negative attitude towards patients who were late for appointments finding the consequent late running clinic more disruptive than non-attendance.
In contrast, reception staff had more negative attitudes than GPs towards missed appointments, expressing irritation after working hard to find an appointment slot and frustration that the appointment could have been given to someone else.
The patients’ attitude to missed appointments was more complex. They acknowledged how annoying it must be for GP. They also felt that a penalty for missed appointments would be appropriate but that this would not have prevented them from missing their appointment and it was more to compensate the NHS for wasted resources or as a punishment for missing their appointment rather than an incentive to keep their appointment.
Reducing Missed Appointments

The reasons for missed appointments and patient attitudes suggest that introducing a financial burden for missing appointments would not be effective in increasing attendance rates. However various other strategies have been trialled both in general medicine and dentistry. These include:
Telephone and text
Telephone use has changed dramatically in the last 10 years.8 Mobile phone ownership has increased with 93% of UK adults now owning a mobile phone.9 The ownership and use of smartphones has doubled since 2012, and 90% of 16 to 24-year-olds now own one and, overall, 66% of all adults own a smartphone.9
In the UK we now spend on average two hours a day using our phones and send the equivalent of 107 texts per phone per month. All of this suggests that phoning or texting to remind people about their appointments is the ideal way to reduce no shows. Machiria10 found that phone reminders proved effective in primary care medicine, while Su-Mei Liew11 found that texting also produced positive results. The efficacy of text reminders was also found in dental practice.
None of these studies reported on the actual wording of the text message and there is evidence to suggest that even subtle changes can have a profound effect on efficacy. For instance, Haynes et al12 monitored the effectiveness of reminder texts with differing wording and found that a personalised message that included the recipients name was the most effective.
Clinic management
Another strategy that has been suggested to lead to fewer missed appointments is to reduce the time between booking the appointment and the actual appointment itself. The time of the appointment is also important, as it needs to be convenient for the patient. Just offering the next available time slot can lead to an appointment that is inconvenient for bus times or collecting children from school and as we have seen people with busy lives are more likely to miss their appointments so scheduling a time that is most convenient for them is important.
This also raises the question of open access clinics. There are advantages of running an appointment system for both the patient and the practice. From the patient’s point of view it allows them to plan ahead and means less waiting in the practice.6 It is also better for ongoing management, such as in shared care schemes. For the practice, the benefits include less practitioner stress and an ability to control the workload both in terms of number of appointments and the length of the appointment needed.
The frustrations caused by an appointment system compared to an open access clinic include non-attendance but also patients being unhappy that they cannot get an immediate appointment or on their preferred day. An appointment system also requires an efficient practice system to both make and cancel/change appointments and can lead to receptionist stress in negotiating with patients who see them as a barrier to their preferred outcome. It can also increase the stress levels of the patient in having to attend at a particular time such as finding suitable parking or arranging time off work.
Clinical Consistency
Recognising that people have a preference for who they see will also influence their attendance. Asking them if they have a preference at the time of booking is simple and will help compliance.
We also have a duty to educate our patients about the importance of the on-going nature of eye care and the need for future appointments. We can also ensure that support staff reinforce the message that it is never too late to cancel or re-book an appointment, especially as it is then available for someone else to use.13
Conclusion
Implementing and auditing a programme to reduce the incidence of missed appointments is an easy exercise for a practice to conduct. Setting up an audit of missed appointments, instigating a programme to reduce the no shows and then re-auditing the results will monitor how effective the intervention is. Given the clinical importance of appointments and the extent and cost of missed appointments, it should be something that is constantly monitored and improved by all practices.
A good reminder will contain certain critical information. If implementing a reminder system, a few key points to include in the reminder might be as follows:
- The practice name and contact details.
- What the reminder is for – a routine check or a more specific reason such as supplementary tests or monitoring.
- The time.
- The date.
- The location of the appointment and who it is with.
- A ‘call to action’ – a specific reminder to attend or to change the appointment if it is inconvenient.
I hope this overview provokes some thought about why no-shows happen and why we need to be aware of their nature, not just for commercial reasons but for sound clinical care reasons too.
Andy Millington is an optometrist with a private practice in Chepstow and teaches at Cardiff University where he has been instrumental in the development of the special clinic service aimed at children with learning and cognitive impairment.
References
- England N. [Available from www.england.nhs.uk/statistics/statistical-work-areas/hospital-activity/quarterly-hospital-activity/qar-data/.
- Health Do. A zero cost way to reduce missed hospital appointments 2016 [Available from www.gov.uk/government/publications/reducing-missed-hospital-appointments-using-text-messages/a-zero-cost-way-to-reduce-missed-hospital-appointments.
- Office NA. NHS waiting times for elective care in England. 2014.
- Association BD. Failure to attend. 2013.
- Neal RD, Hussain-Gambles M, Allgar VL, Lawlor DA, Dempsey O. Reasons for and consequences of missed appointments in general practice in the UK: questionnaire survey and prospective review of medical records. BMC Fam Pract. 2005;6:47.
- George A, Rubin G. Non-attendance in general practice: a systematic review and its implications for access to primary health care. Fam Pract. 2003;20(2):178-84.
- Martin SJ, Bassi S, Dunbar-Rees R (2012) Commitments, norms and custard creams – a social influence approach to reducing did not attends (DNAs). Journal of the Royal Society of Medicine 105: 101-4.
- Liew SM, Tong SF, Lee VK, Ng CJ, Leong KC, Teng CL. Text messaging reminders to reduce non-attendance in chronic disease follow-up: a clinical trial. Br J Gen Pract. 2009;59(569):916-20.
- OFCOM. Landline and Mobile Statistics. 2016.
- Macharia WM, Leon G, Rowe BH, Stephenson BJ, Haynes RB. An overview of interventions to improve compliance with appointment keeping for medical services. JAMA. 1992;267(13):1813-7.
- Foley J, O’Neill M. Use of mobile telephone short message service (SMS) as a reminder: the effect on patient attendance. Eur Arch Paediatr Dent. 2009;10(1):15-8.
- Haynes LC, Green DP, Gallagher R, John P, Torgerson DJ. Collection of Delinquent Fines: An Adaptive Randomised Trial to Assess the Effectiveness of Alternative Text Messages. Journal of Policy Analysis and Management. 2013;32(4):718-30.
- Contracting NPC. Shared learning: Managing and minimising failure to attends (FTAs).
