It has been said that the patient experience is the sum of all interactions1 and in the context of the customer journey in optometric practice, many of these interactions are within the control of the eye care professional (ECP) in the consulting room. Where this is the case, it is important for all touchpoints to be managed well in order to deliver a great patient experience and in turn, a successful clinical outcome. This is especially important in relation to contact lens fitting, and toric contact lenses are no exception. This article will describe the various stages in fitting soft toric contact lenses and identify the key ECP touchpoints in a soft toric contact lens fitting appointment that will help ensure a positive outcome for both ECP and patient alike.
Who needs a toric contact lens?
Research suggests that almost half of all spectacle wearers have clinically significant astigmatism (≥0.75D) in at least one eye 2 so it would be reasonable to assume that toric contact lens prescribing rates would closely align with this. International prescribing trends suggest that toric contact lens prescribing rates vary widely in different countries but the biggest discrepancy is with daily disposable toric prescribing (figure 1) which is some distance from mirroring the prescribing rate of astigmatism in spectacle wearers.3
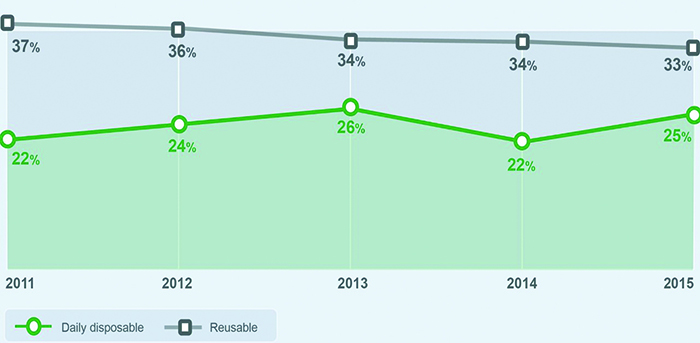
Figure 1: Fitting of disposable versus repeat use toric contact lenses (with kind permission of P Morgan, the University of Manchester, 2016)
There may be a number of reasons for this discrepancy in prescribing:
1 Prescription – sphere, cylinder and axis

Prevalence of astigmatism within a population of spectacle wearers will include a wide range of prescriptions that when adjusted for back vertex distance (BVD) renders the cylinder value lower than what is considered clinically significant in a contact lens prescription. For example, a spectacle prescription of
-9.00/-0.75x180 @12mm -8.12/-0.61x180 @0mm.
The value of the cylinder at the corneal plane (-0.61D) is less than the minimum available cylindrical correction in toric contact lenses and it would make sense to select a spherical contact lens in this instance. Naturally, the opposite is true for plus powers but the typical distribution of refractive error is skewed towards myopic prescriptions which may contribute towards the explanation of the contrast in prevalence of astigmatism between spectacle prescribing and toric contact lens prescribing.4
The location of the astigmatism may also influence prescribing decisions with toric contact lenses where with the rule astigmatism and oblique astigmatism appears to have greater detrimental impact on reading speed than against the rule astigmatism.5
2 Ocular dominance

There is a large proportion of the spectacle wearing population with clinically significant astigmatism in one eye only and this may influence the decision to prescribe a toric contact lens especially if the astigmatism is in the non-dominant eye.2
3 Pupil size
Similarly, pupil size may also influence prescribing decisions; if the pupils are miotic and the cylinder value is towards the lower range the predicted visual outcome could be considered to be adequate with a spherical contact lens design.
4 Choice
While the quality and availability of toric contact lenses has expanded over the recent years, choice within the daily disposable category has remained limited up until now compared to reusable soft toric lenses with both parameter range and material options. If a daily disposable modality is required either through patient request or ECP recommendation, wearers may be prescribed spherical daily disposable lenses where a toric lens is likely to give a better visual outcome.
Considering all of these discussion points, it has been estimated that approximately 36% of the contact lens wearing population should be fitted with a toric contact lens in at least one eye.2 However, a number of studies have shown significant improvements in visual acuity through fitting low astigmats (0.75D, 1.00D) with toric soft lenses compared with spherical soft lenses.6,7 Measurements of eye strain have also been found to be significantly better (28% less) with toric soft lenses compared to spheres.8
Holden9 indicated that the prevalence of astigmatism is 45.4% with a correction threshold of ≥0.75D. Whether the threshold is 36% or 45.4%, the fact remains that prescribing torics is significantly under-represented within the daily disposable modality although with broader product ranges entering the market, this is set to change.
Defining the key moments in soft toric contact lens fitting
Once a decision has been made to fit a toric lens there are several key moments that have the potential to significantly improve the experience for the wearer and favourably influence overall success rates.
1 Lens selection
Given that regional variations in thickness are essential characteristics of modern soft toric contact lenses, choice of contact lens materials with oxygen transmissibility levels that help to maintain corneal physiology should be a key consideration for both new and existing astigmatic contact lens wearers. The recent introduction of new silicone hydrogel daily disposable toric lenses to the market offers higher levels of oxygen transmissibility compared to daily disposable hydrogel toric lenses and are welcome additions for ECPs and wearers keen to benefit from the health and convenience of a one-day modality (figure 2).
 Figure 2: Dk/t mapping of a range of daily disposable toric contact lens materials and prescriptions. The Dk/t scale has been standardised to enable correct like-for-like comparison of Dk/t over the complete lens
Figure 2: Dk/t mapping of a range of daily disposable toric contact lens materials and prescriptions. The Dk/t scale has been standardised to enable correct like-for-like comparison of Dk/t over the complete lens
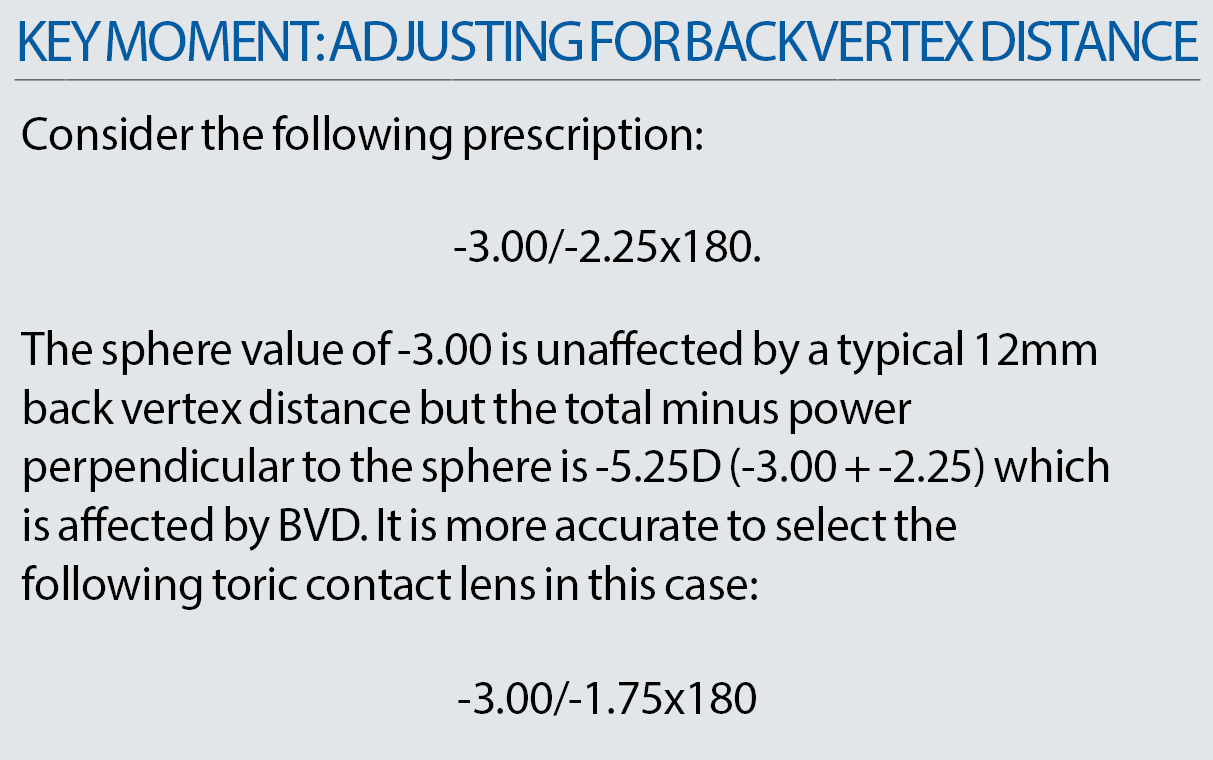
2 Adjusting for back vertex distance.
The general ‘rule-of-thumb’ is to make an adjustment for back vertex correction for powers of ≥4.00D. It is important to remember that this needs to be considered for both meridians of power in astigmatic prescriptions.
Of course this has a bearing on even higher astigmatic prescriptions, which at first glance may not initially be considered within range for a daily disposable toric lens.
For example:
-10.00/-3.00x180 @12mm -9.00/-2.25x180 @0mm
which is now available as a daily disposable toric lens in three options. Of course the opposite is true for plus prescriptions where the cyl value increases with back vertex adjustments.
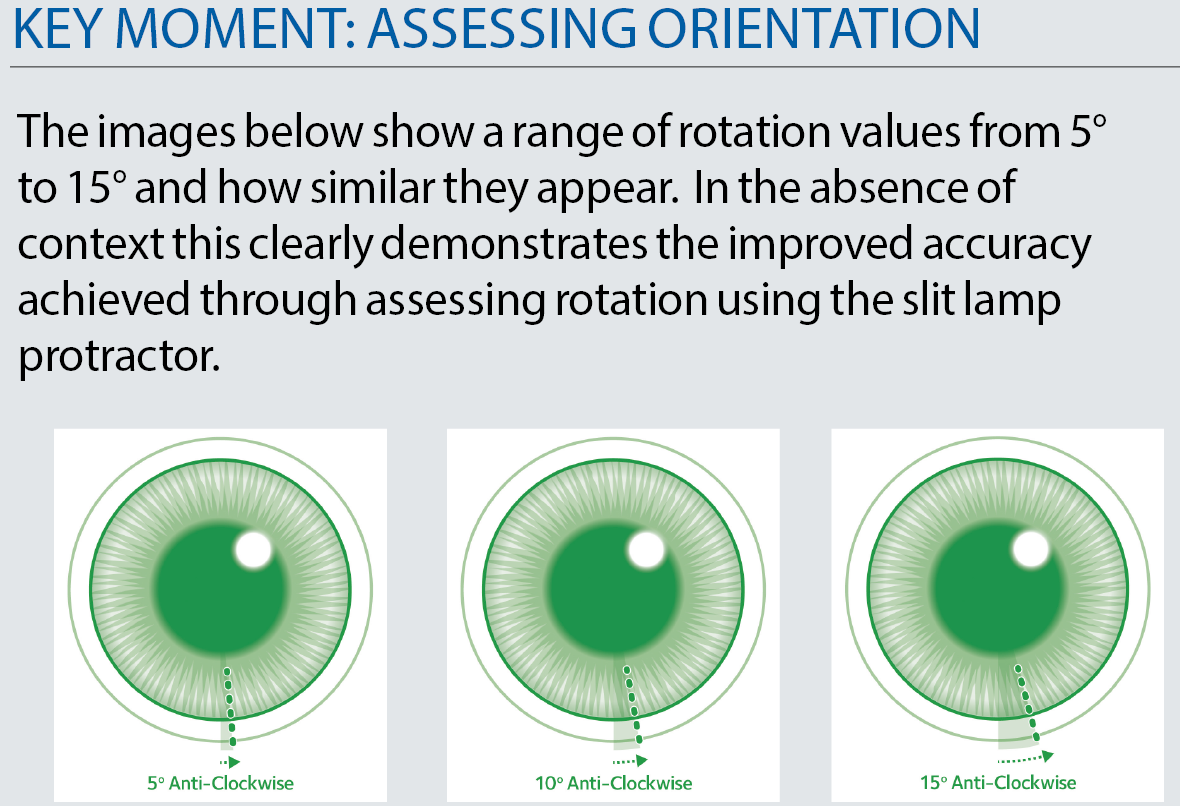
3 Assessing the fit – orientation
Aside from assessing centration and movement in the typical way, it is important to review the orientation of a toric lens to establish whether or not any axis adjustments need to be made.
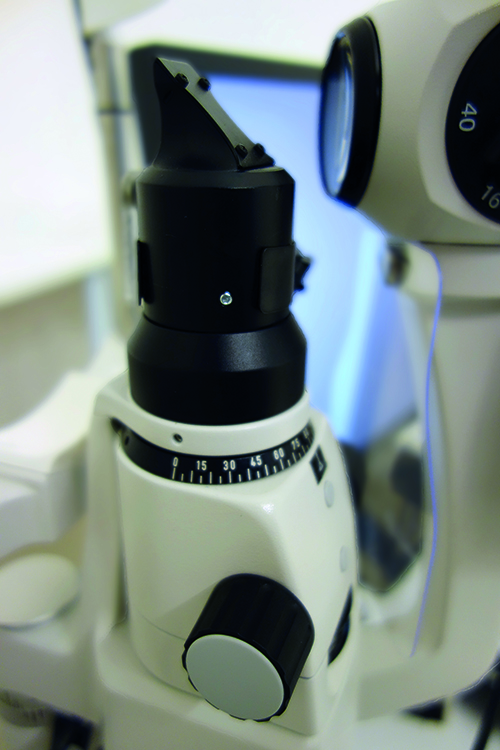 Figure 3a: Slit-lamp protractors
Figure 3a: Slit-lamp protractors
It is important to do this as accurately as possible using the slit-lamp protractor (figure 3a+b) to help as it is easy to under-estimate rotation and this can affect the visual outcome quite significantly – especially with higher astigmatic corrections.

Figure 3b: Slit-lamp protractors
4 Assessing the fit – axis adjustment

Once the rotation has been measured, it is then important to reference the original spectacle axis if this is different to the axis of the trial lens you have selected. (This may be the case where the spectacle axis is 175 and you have chosen a contact lens with an axis of 180.)
Consider the following spectacle prescription:
-1.25/-1.75x175
With standard contact lenses being supplied in axes with 10° intervals, you could choose a contact lens axis of 170° or 180° for this prescription. Most often, it is sensible to choose the axis closest to the major meridian – in this case it would be 180°.
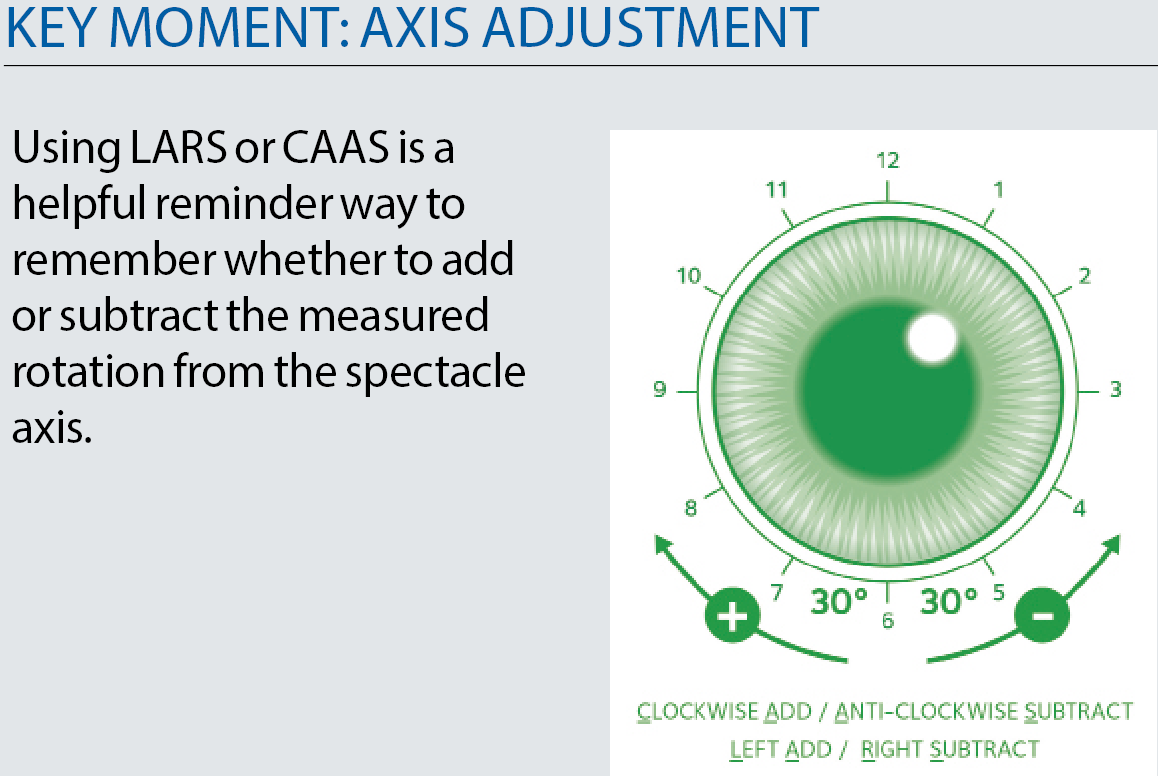
What if the lens settles at an orientation of 5° anti-clockwise? You would subtract 5° from the original spectacle axis which gives 170°. The new toric lens to order would be -1.25/-1.75x170.
It is important to remember that the orientation marker of the new toric lens will still locate at 5° anti-clock-wise.
Now imagine the same lens stabilised at 5° clockwise rotation. This suggests the need to add 5° to the spectacle axis which gives 180°. By serendipity, the lens the patient is fitted with is in perfect alignment with the spectacle prescription and there is no need to adjust for the observed rotation. Without referencing the original spectacle axis and referring to the contact lens axis, it might be tempting to trial additional diagnostic lenses unnecessarily. Where higher astigmats are fitted with extended range products supplied in 5° axis intervals, this approach can really improve the patient experience by accurately measuring rotation and referencing the spectacle axis when applying LARS or CAAS.
5 Assessing the fit – stability
Another key moment in a successful toric lens fit relates to the stability of a toric lens on the eye. It is not enough to check stability in primary gaze, but to also check stability simulating realistic eye movements to be confident that the wearer experience remains good outside of the consulting room.10 There are two approaches that can be used here:
Option 1:
With the patient at the slit-lamp, focus on the orientation mark in primary gaze. Keeping the illumination and observation systems fixed, ask your patient to look up and left (eg car-rear view mirror), and blink before returning to the starting position. Check that the orientation mark remains close to your original observation to confirm lens stability. Repeat this for other gaze positions and record the results. Any significant time delay for the orientation marker to return to its original starting position would suggest that stability might be a concern and an alternative toric lens design could help. This is shown in figure 4.


Figure 4: Assessing toric lens stability on the slit lamp
Option 2:
Using the test chart as a distance target, ask your patient to look up and left and then return to the test chart. Any significant time delay in being able to read the best corrected acuity with toric contact lenses might infer that stability of the toric lens design is not ideal. Again, this can be repeated in other positions of gaze and also with near acuity targets.
Patient retention
With the undisputed safety profile of the daily disposable modality,11 it is encouraging to see additional daily disposable toric products entering the market. The challenging logistics of manufacturing and stocking large parameter ranges appear to have been addressed with parameter ranges in daily disposable toric lenses closely matching that of their reusable counterparts. Additionally, ‘borrowing’ technology from successful reusable toric lens designs in daily disposable options, along with more silicone hydrogel options serves to reinforce ECP confidence with daily disposable toric lenses. With retaining contact lens patients a key consideration for practice growth, fitting a product that matches the lifestyle requirements and prescription needs of each patient would seem to be the most logical approach to help achieve this.
Conclusion
ECPs are now strongly positioned to add value during reviews of existing astigmatic contact lens wearers fitted with older toric designs, material or modality and discuss daily disposable alternatives that may offer better health and convenience to the patient without sacrificing on comfort or vision. Equally, the opportunity to easily introduce soft toric lenses to new wearers has never been greater.
Consulting room tools like OptiExpert, for example, have been specifically designed with busy ECPs in mind to help efficiently and accurately address back vertex distance adjustments for initial toric trial lens selection and orientation adjustments to address any rotation observations which can help deliver a great patient experience.
Elizabeth Lumb is an optometrist and European professional services manager, CooperVision. This article was supported by CooperVision.
References
- The State of Patient Experience in American Hospitals. The Beryl Institute, Spring 2011.
- Young G, Sulley A and Hunt C. Prevalence of astigmatism in relation to soft contact lens usage. Eye & Contact Lens 2011;37:20-25.
- Data from Philip Morgan, the University of Manchester, 2016.
- Prevalence of refractive error in Europe: the European Eye Epidemiology (E3) Consortium Eur J Epidemiol. 2015; 30(4): 305-315.
- Nanavaty MA, Vasavada AR, Patel AS, et al. Analysis of patients with good uncorrected distance and near vision after monofocal intraocular lens implantation. J Cataract Refract Surg 2006;32:1091-7.
- Dabkowski JA, Roach MP, Begley CG. Soft toric versus spherical contact lenses in myopes with low astigmatism. Int Cont Lens Clinic 1992;19:252–256.
- Richdale K, Berntsen DA, Mack CJ, et al. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci 2007;84:969–975.
- Berntsen D et al. The effect of toric versus spherical contact lenses on vision and eyestrain in astigmatic patients. American Academy of Optometry, 2015 Scientific Abstract.
- Holden BA. The principles and practice of correcting astigmatism with soft contact lenses. Aust J Optom 1975;58:279-299.
- Chamberlain P1, Morgan PB, Moody KJ, Maldonado-Codina C. Fluctuation in visual acuity during soft toric contact lens wear. Optom Vis Sci. 2011 Apr;88(4).
- Chalmers RL, Hickson-Curran S, Keay L, et al. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci 2015;56:654-663.
