If there is any doubt that contact lens dropout could be a major challenge for you, your patients and your practice, look no further than the latest data on the UK market. In 2016, an estimated 800,000 people were new to contact lenses but almost as many – 700,000– dropped out (figure 1).1
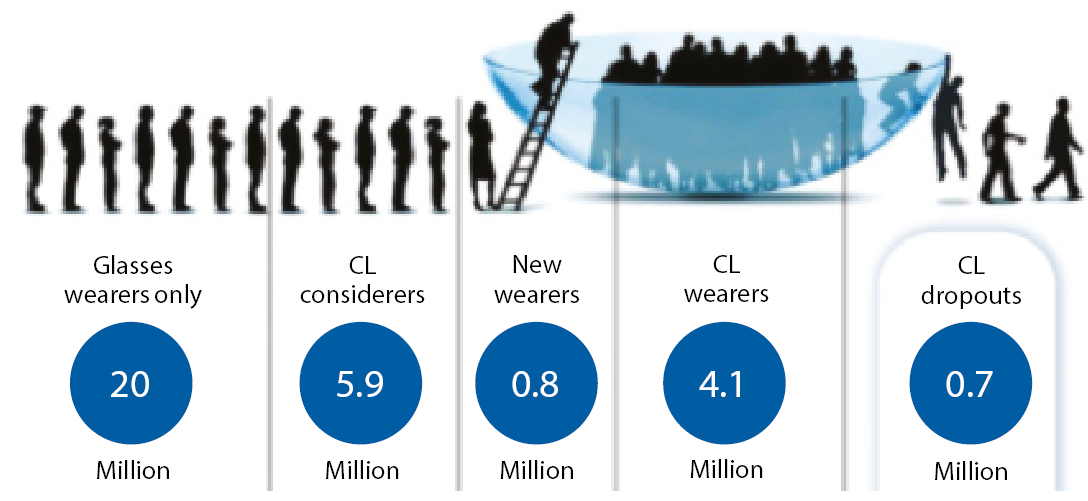
Figure 1: The UK contact lens market in 20161
When their lifetime value to your practice makes contact lens wearers an average of 60% more profitable than spectacles-only wearers,2 the business implications of this ‘leaking bucket’ are also clear. In fact, dropout has an impact throughout your business, from wasted chair time to loss of satisfaction, confidence and loyalty among your patients.
Turning the challenge of dropout into an opportunity may require a targeted approach. New research findings are changing our thinking on the reasons for dropout and show that different strategies are needed to help retain patients in contact lenses at key moments during a lifetime of wear:
- When first fitted with contact lenses
- When an established contact lens wearer
- When reaching presbyopia
This article will review what we now know about dropout at these key moments, how we can identify those at risk and how we can tailor our management strategies to support retention at each stage.

The new wearer
Discomfort and dryness have long been considered the primary reasons for dropout but typically studies involve broad patient populations.3-10 Two new studies focused on the reasons behind dropout among new wearers and whether the lens type worn and other factors influence retention.11,12
Both were multi-site, sponsor-masked and conducted in a representative range of UK practices. One was a retrospective chart review of 524 patient records11 and the other a prospective fitting study to which 531 patients were recruited.12 Each looked at new contact lens wearers over the course of the first year of wear and each identified potential opportunities to improve retention rates.
The practitioners’ view
When patient records were reviewed, the practitioner-reported overall retention rate at one year was 74%, or a dropout rate of 26%.11 But nearly half of those who gave up in the first year did so in the first two months, and a quarter within the first month (figure 2), showing that the early stages of lens wear are crucial to ongoing success.
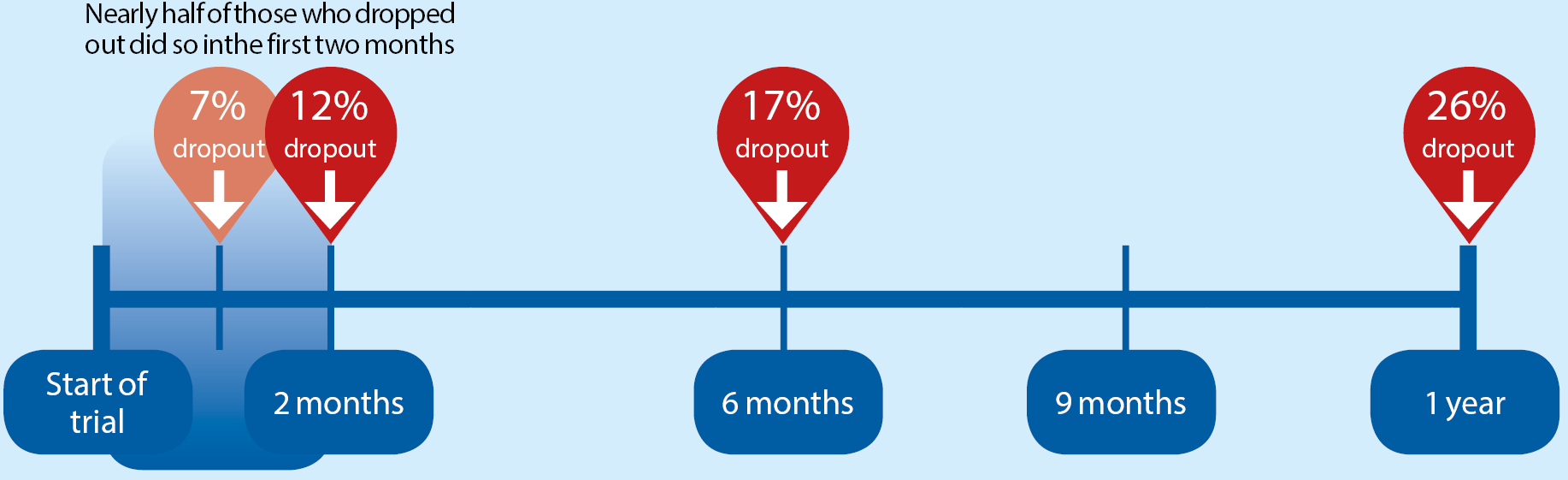
Figure 2: Proportion of new wearers who discontinued lens wear by number of days since dispensing (n=510, for 14 patients time discontinued unknown)11
The study found that new wearers aged under 45, those with higher sphere powers, single-vision lens wearers, and those who bought lenses on a regular quarterly basis, were significantly more likely to still be in contact lenses after a year.
Retention rates were not related to gender, lens replacement frequency, material type or toric cylinder power. Type or location of practice had no influence on dropout but retention rates varied widely between individual practices, from 40% to 100%.
Practices that were more successful at retaining patients (>80% overall rate) tended to carry out more fittings per week (10.5 vs 6.3) than those that were less successful (<70%) and have a higher proportion of turnover from contact lenses.13 They were also more likely to offer a full-time contact lens service.13
The reasons why new wearers discontinued show that dropout is more complex than we supposed. While handling and comfort were the most commonly cited performance-related reasons for discontinuing in new spherical lens wearers, visual problems were the most common reason among new wearers of toric and, especially, multifocal lenses.
As expected, dropout due to handling problems decreased as experience increased. If lens performance was poor, cost also became an issue after three months or more of wear, although contact lens wearers are known to be health not price driven.14
So while discomfort and dryness are the most common reasons for dropout overall, these new findings suggest that vision problems among new wearers are – at the very least – more of a factor than previously thought.
Crucially, practitioners taking part in this study were often unaware their patients had lapsed and for nearly one in three dropouts (32%) the reason for discontinuing was unknown.
And despite research showing 77% of lapsed wearers can be successfully refitted,6 in only a minority of cases (29%) had patients had a further trial fitting, modified power or different lens type been tried before the patient dropped out.
The patients’ view
So were the findings consistent when new wearers were fitted then surveyed over the course of the first year rather than past records reviewed?
The overall one-year retention rate was similar (78%) and those with spherical refractions more likely to still be wearing lenses at the end of the year.12 From this study, women were more likely to continue than men.
Poor vision was the primary patient-reported reason for discontinuation among toric and multifocal wearers, followed by poor comfort (figure 3). As with the retrospective chart review, for sphere wearers poor vision was much less likely to be a factor.
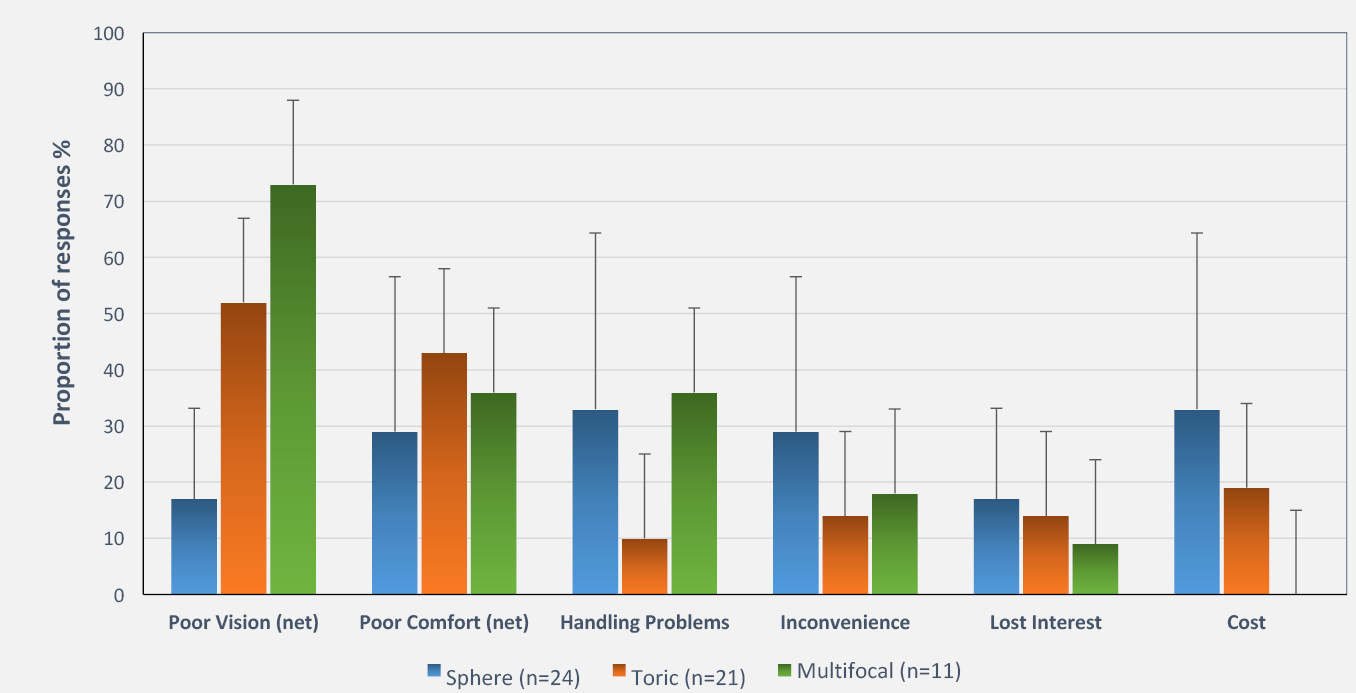
Figure 3: Patient-reported reasons for discontinuing lens wear among new wearers (n=56) in prospective study.12 Error bars show 95% confidence intervals
Patients who wore lenses full time (≥4 days/week) were significantly more likely than part-time wearers (≤3 days/week) to still to be wearing them after a year. And those who routinely received their lenses by post were more likely to continue than if lenses were posted on request or collected from the practice.
Thus there are many opportunities to improve retention among those new to contact lenses. While both vision and comfort are key factors, confidence in lens handling and habit formation also play significant roles in this group, especially in the first few weeks of wear.
The established wearer

Among established wearers, the most common reason for discontinuation is discomfort, reported by around half of those who lapse.3,4,7-10 Maintaining comfort is therefore a key goal if patients are to benefit from a lifetime of contact lens use.16
Research is now revealing more about comfort over the cycle of lens replacement and daily wear that suggests the way patients are questioned about comfort is critical to understanding contact lens performance.
The silent sufferer
End-of-day comfort with widely prescribed monthly replacement lenses declines over the course of a month’s wear.17 As many as a half of these patients report being ‘dissatisfied’ or ‘neutral’ in the final week before lenses are replaced. In fact over two-thirds of patients using monthly lenses experience comfort-related issues.18
Most of these ‘silent sufferers’ resort to compensating behaviours – such as using rewetting drops, removing their lenses and taking breaks from lens wear – to get through a month of wear (figure 4).18 Most report being frustrated, annoyed and inconvenienced.17 Yet crucially, many do not plan to tell their practitioner and, of these, most (85%) believe discomfort issues are a part of normal contact lens wear.

Figure 4 Experience among the two-thirds of patients reporting comfort issues with widely prescribed monthly lenses (n = 23717 and 75818)
Questioning about compensating behaviours, and asking whether lenses are as comfortable at the end of the replacement cycle as on day one, can help elicit much more from those patients who may seem ‘fine’ but clearly are not.
Our understanding of the mechanisms underlying contact lens-related discomfort is also improving, leading to more effective management strategies.
The Tear Film and Ocular Surface (TFOS) International Workshop on Contact Lens Discomfort19 proposed a progression of discomfort, from ‘strugglers’ who experience lens awareness and visual disturbance that, if not addressed, result in reduced wearing time, to temporary discontinuation and, ultimately, permanent dropout (figure 5).
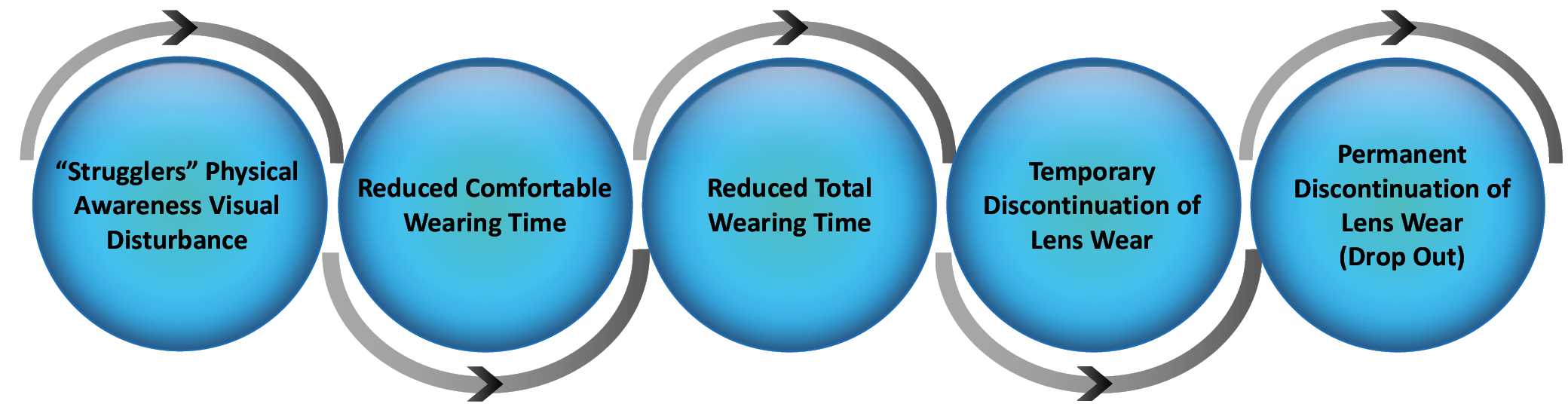
Figure 5 Progression of contact lens discomfort, adapted from TFOS19
Many contact lens types are associated with reduced user comfort from mid-afternoon onwards.20 Although declining comfort over the course of the day is also influenced by changes to the ocular environment,21 there may be little the wearer can do to alleviate ambient conditions or avoid challenging visual tasks such as prolonged digital screen use.
Clearly it is important to elicit symptoms at the end of the day as well as monitoring overall comfort. Supplementing questions about number of hours a day and days a week the lenses are worn comfortably can identify ‘strugglers’.
Asking patients to grade lens performance on a 0-10 scale will reveal a truer picture than simply asking: ‘How are your contact lenses?’ Use clinical signs and tests identified as correlating with contact lens discomfort,22 and in-practice tools such as grading scales. Probing the type of discomfort experienced is also useful; dryness is a key aspect of lens-related discomfort that drives discontinuation.23
Research has also shown, for the first time, an association between ocular surface sensation and quality of vision.24 Careful questioning about differences in visual quality through the day, in comparison with spectacles and for specific tasks, may therefore help identify ‘strugglers’ at risk of lapsing.
After discomfort, poor vision is consistently the next most common reason for dropping out among established wearers.6,9,10 Changing visual needs – such as uncorrected astigmatism and changes to lifestyle or work – should always be addressed.
Although toric lens designs have advanced, astigmats remain over-indexed in the dropout population.6,25,26 Toric contact lenses are still under-prescribed27 and a very high proportion of astigmats not using torics – including previous dropouts – can be successfully re-fitted (92%).28 Toric lenses have also been shown to deliver additional visual quality of life benefits to astigmatic wearers.29
The patient-centred approach
For new and established wearers alike, personalised prescribing – where contact lens recommendation is centred on the patient’s needs – is crucial to ongoing success.30 This approach – matching the lens to the patient, not the patient to the lens – leads to a better understanding of why you are recommending a particular product that can improve long-term outcomes and help reduce dropout.
Resources are now available to identify the predominant patient need, such as a simple pre-fitting questionnaire. Each aftercare appointment then provides an opportunity to ensure that patient needs continue to be met. Remember also to record and remind your patients why they first started wearing contact lenses to help maintain their motivation.
Selecting the optimal contact lens for each patient is therefore crucial. The TFOS workshop identified lens properties associated with improved comfort, such as friction, modulus and lens edge design.31 Advances in lens materials and design mean that a very high proportion of lapsed wearers can be successfully and easily refitted with new lenses, whether spherical or toric.26
Finally, remember that dropout among established wearers can occur at any age. More than half of all dropouts are under the age of 40,32 although the youngest wearers – aged eight to 17 years – show very high retention rates, at 87% on average for experienced wearers.33
Since fewer males aged between 18 and 33 years wear contact lenses than those younger than 18 years, a different approach may be needed to retain them.34 Factors such as contact lens care and convenience may be deterring males from continuing with lens wear as they mature.
The emerging presbyope

Our understanding of dropout with advancing age is also improving and suggests a major opportunity to encourage retention among emerging presbyopes.11,12,35
Among new wearers of multifocal contact lenses, the predominant patient-reported reason for dropping out is vision problems.12
However, new designs offering excellent visual outcomes have become available. Harnessing either improved designs or better fitting procedures can optimise vision and encourage retention.
A recent survey of 496 presbyopic patients aged 40 years and older again found poor vision (38%) and discomfort (34%) were the primary reasons for discontinuation.35 But convenience was also a factor, cited by 20% of lapsed wearers. Notably, those who began contact lens wear after the onset of presbyopia were no more or less likely to discontinue than long-term wearers.
While visual challenges will always be greater with presbyopes, the launch of new products has brought increased confidence and success in multifocal fitting which bodes well for increased retention for this group. Materials that help overcome dryness issues, and more daily disposable options to address convenience and flexibility, may also help retain patients in contact lens wear.
Presenting all the contact lens options, demonstrating the difference to the patient in real world situations and, again, tailoring your recommendation to individual needs are also key. Examples are combining progressive spectacles and multifocal contact lenses, using over-spectacles for specific tasks, or adding single-vision daily disposables for some activities where more suitable.
Early assessment is relatively unrepresentative of performance later on during multifocal contact lens wear and acuity-based measures are insensitive indicators of performance compared with subjective alternatives.37 Allow a period of adaptation before recalling multifocal wearers, and ask them to score their subjective vision at distance, intermediate and near.
Motivate and captivate
A deeper understanding of contact lens dropout and the underlying reasons why patients discontinue is informing our management strategies for keeping patients, whether new or established, young or presbyopic, in contact lenses.
Many strategies and in-practice tools are available that can easily be implemented to encourage retention. Ensure vision is optimally corrected, wearers are confident in handling lenses, and their comfort experience is fully explored and addressed with new technologies. Meet the patient’s predominant need from the outset and offer alternatives when needs change.
What motivates a person to start wearing contact lenses is unlikely to be what will make them stay in contact lenses across all life stages. Pay attention to retention and your patients can enjoy a lifetime of contact lens wear. And by improving practice efficiency, your business will benefit too.
Jane Veys is director, Global Professional Education and Anna Sulley is associate director, Global Strategic Medical Affairs, at Johnson & Johnson Vision Care.
Acknowledgements
Thanks to Stuart Todd and Anne Madec-Hily, Global Strategic Insights, at Johnson & Johnson Vision Care, for their input, and Alison Ewbank for help in preparing this article.
References
- Data on file. UK Incidence Study. Johnson & Johnson Vision Care 2016.
- Ritson M. Which patients are more profitable? CL Spectrum 2006;21:3 38-42.
- Weed KH, Fonn D and Potvin R. Discontinuation of contact lens wear. Optom Vis Sci 1993;70:12s 140.
- Pritchard N, Fonn D and Brazeau D. Discontinuation of contact lens wear: a survey. Int Contact Lens Clin 1999;26:157-162.
- Harknett T, Bowden T, Shadbolt H et al. Five years after dispensing – are contact lenses a success? Cont Lens Anterior Eye 2001;24:127-8.
- Young G, Veys J, Pritchard N et al. A multicentre study of lapsed contact lens wearers. Ophthal Physiol Opt 2002;22:6 516-527.
- Jutai J, Woolrich W and Strong G. The predictability of retention and discontinuation of contact lenses. J Am Optom Assoc 2003;74: 5 299.
- Richdale K, Sinnott LT, Skadahl E et al. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea 2007;26:2 168-74.
- Rumpakis J. New data on contact lens dropouts: An international perspective. Rev Optom 2010;147:1 37-40.
- Dumbleton K, Woods CA, Jones LW et al. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens 2013;39:93-9.
- Sulley A , Young G and Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye 2016;40:1 15-24.
- Sulley A, Young G, Hunt C et al. Prospective evaluation of new contact lens wearer retention rates. Eye & CL 2017 (in press).
- JJVC Data on file 2014. Vision Care Research. UK Contact Lens New Wearers Retrospective Study Report.
- Aslam A. What drives vision correction purchases? Optician 2014;247:6458 16-20.
- Ewens E. How to support contact lens wearers for success. Optician 2013;246;6431 32-35.
- Morgan PB. Optimising contact lens wear for a lifetime of use. Optician 2013;245;6400:32-37.
- JJVCC data on file 2016, MR survey with habitual SiH monthly CL wearers in US (2 widely prescribed SyHy CLs). N=237.
- JJVCC data on file 2016. GSI wearer experience online survey. US, UK & Germany. N=758 spherical SyHy monthly replacement CL wearers. % wearers who selected one or more of the responses.
- Nichols KK, Redfern RL, Jacob JT et al. The TFOS International Workshop on CL Discomfort: Report of the Definition and Classification Subcommittee. Invest Ophthalmol Vis Sci 2013;54: TFOS14-19.
- Plowright AJ, Morgan PB, Maldonado-Codina C et al. An investigation of ocular comfort in contact lens wearers, spectacle wearers and non-wearers. Optom Vis Sci 2008. E-abstract 85050.
- Navascues-Cornago M, Morgan PB and Maldonado-Codina C. Effect of three interventions on contact lens comfort in symptomatic wearers: a randomized clinical trial. PLoS One 2015; Aug 12:10:8.
- Papas EB, Ciolino JB, Jacobs D et al. The TFOS International Workshop on CL Discomfort: Report of the Management and Therapy Subcommittee. Invest Ophthalmol Vis Sci 2013;54:11 TFOS183-203.
- Chalmers RL. Overview of factors that affect comfort with modern soft contact lenses. Cont Lens Anterior Eye 2014;37:2 65-76.
- Rao SB and Simpson TL. Impact of blur on suprathreshold scaling of ocular discomfort. Invest Ophthalmol Vis Sci 2015;56:2304-2311.
- Young G. Why one million contact lens wearers dropped out. Cont Lens Anterior Eye 2004;27:83-85.
- Canavan K, Coles-Brennan C, Butterfield R et al. Multi-center clinical evaluation of lapsed wearers refitted with senofilcon A contact lenses. Optom Vis Sci 2014. E-abstract 145180.
- Young G, Sulley A and Hunt C. Prevalence of astigmatism in relation to soft contact lens usage. Eye & Contact Lens 2011;37: 20-25.
- Sulley A, Young G, Lorenz KO et al. Clinical evaluation of fitting toric soft lenses to current non-users. Ophthal Physiol Opt 2013;33:2 94-103.
- Nichols J, Berntsen D, Bickle K et al. A comparison of toric and spherical soft contact lenses on visual quality of life and ease of fitting in astigmatic patients. Paper presentation at Nederlands Contactlens Congres, March 2016.
- Meyler J, Pall B and Todd S. Changing the conversation. Optician 2017; 253:6584 26-29.
- Jones L, Brennan NA, González-Méijome J et al. The TFOS International Workshop on CL Discomfort: Report of the Contact Lens Materials, Design, and Care Subcommittee. Invest Ophthalmol Vis Sci 2013;54:11 TFOS37-70.
- JJVC Data on file 2016. European Incidence Study. n=42,058 Independent online survey consumers age 15+ in nine European countries and Russia.
- Chalmers RL, Hickson-Curran S, Keay L et al. Adverse events and retention of children and teens in a large daily disposable contact lens registry. Paper presentation at Nederlands Contactlens Congress, March 2016.
- Lam DY, Kinoshita BT, Jansen ME et al. Contact Lens Assessment in Youth: methods and baseline findings. Optom Vis Sci 2011;88:6 708-715.
- Rueff EM, Varghese RJ, Brack TM et al. A survey of presbyopic contact lens wearers in a university setting. Optom Vis Sci 2016;93:8 848-854.
- Ruston R, Sulley A and Madec-Hily A. From science to practice: a new multifocal. Optician 2016;251:6534 20-25.
- Papas EB, Decenzo-Verbeten T, Fonn D et al. Utility of short-term evaluation of presbyopic contact lens performance. Eye Contact Lens 2009;35:144-148.
