In the first article in this series, we considered Acanthamoeba keratitis (Optician 05.05.17). In this second discussion of keratitis, the focus will be upon bacteria.
Bacteria are often associated with infection and it is not uncommon to have an ailment and to think immediately of the need for antibiotics (compounds that ‘kill’ bacteria). This concept has become so engrained in society that often the deeper understanding of bacterial infection is overlooked. Bacterial keratitis is a potentially serious corneal infection that can cause visual impairment if not treated. It is a significant global health problem and is often associated with contaminated contact lens wear in developed countries and agricultural work with exposure to organic matter in developing nations.
This article offers a broad overview, discussing what bacterial keratitis is, what bacteria cause it, what are the symptoms, and what can be done to diagnose and treat bacterial keratitis and prevent it completely.
What are bacteria?
Bacteria are microscopic organisms, typically a few micrometres (10-6m) in length. They are described as ‘prokaryotes’, which means that they are unicellular, lacking a membrane-bound nucleus, mitochondria and other membrane-bound organelles. It is now widely accepted that bacteria were among the first living organisms on Earth, with ‘proteobacteria’ responsible for eukaryotic evolution (organisms with membrane-bound organelles), through a series of endosymbiotic events (engulfment and non-digestion of bacteria by microorganisms to their benefit).1
Bacteria inhabit all environments, and it is estimated that there are 5 x 1030 (5 quintillion) on Earth.2 Often bacteria are associated with disease and infection, but they are also vital to our environment (recycling nutrients in the soil, such as the fixation of nitrogen from the atmosphere), and to animal and human bodies. Of note, the human microbiota is composed of approximately 39 x 1012 (39 trillion) bacteria and they populate the epithelial layers, such as the skin, the upper respiratory tract (nose and larynx) and the gut.3 They help the body in the protection against disease-causing bacteria and also, in the case of gut flora, improve the digestion process.
Bacteria that are able to breach the protective layer of the human microbiota and the immune system cause infection through colonisation of human tissues and inflammation. These are defined as pathogenic. They possess molecules that help the invasion process which are called virulence factors. If the immune system is weakened or there is trauma to the epithelial layers, even some species of the microbiota can cause infection and disease.
How do bacteria cause bacterial keratitis?
Keratitis is a severe sight-threatening condition in which the cornea becomes inflamed.4 Vision is impaired and it is often accompanied by severe pain. Bacterial keratitis is caused by a variety of bacteria, and their main mode of transmission is through contaminated contact lenses and/or corneal injury.5 In some cases of corneal injury, infection is caused by bacteria that are normally found in the natural human skin microbiota. In both situations, the bacteria colonise the corneal surface and also gain entry to the lower epithelial layers through small injuries of the cornea.
The role of the contact lens
It is not surprising that contact lens contamination is a major route to infection.6 Due to the ubiquitous nature of bacteria (found everywhere in the environment), it is understandable that contact lens cases, solutions and lens are exposed to bacteria. Individuals usually put lenses on in front of bathroom mirrors, where they are kept on shelves or by sinks for ease of use. Surfaces can be covered in bacteria, invisible to the naked eye; they may be damp allowing excellent breeding conditions for bacterial colonies in biofilm (figure 1).
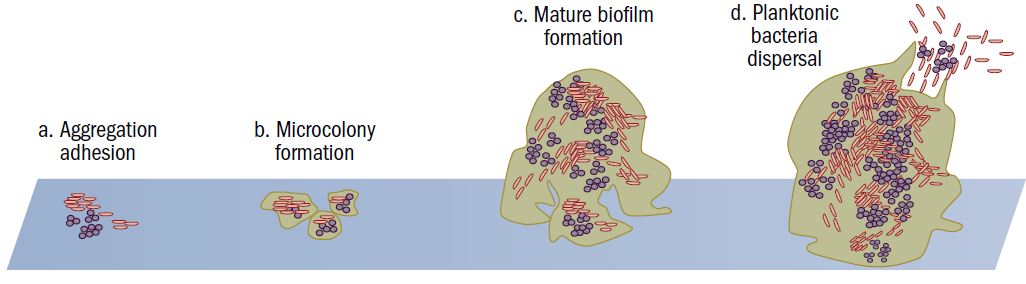
Figure 1A: Biofilm formation on surfaces composed of a. deposit, aggregation, adhesion, b. microcolony formation, c. mature biofilm formation and
d. dispersal
This type of environment is ideal for accidentally cross-contaminating the contact lenses with hands or a towel or napkin. Once on the contact lens, bacteria can stick to the surface through the biofilm or through direct interaction with molecules on the contact lens. All bacteria can contaminate contact lenses, but the most common are Streptococcus, Pseudomonas and Stapylococcus spp.
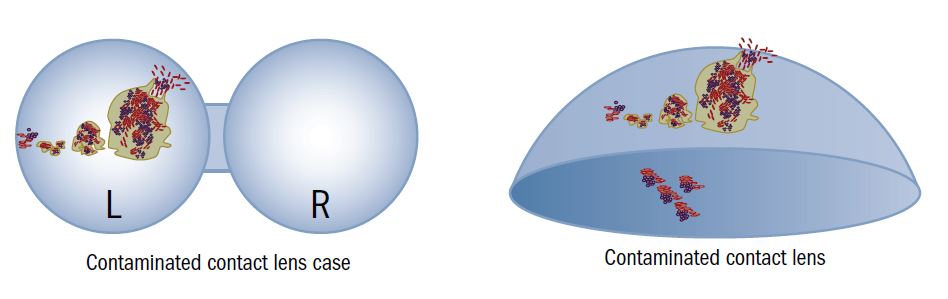
Figure 1B: Biofilm dispersal can contaminate contact lens cases leading to contamination of both sides of the contact lenses. The biofilm cycle
recommences. This is the major risk factor in bacterial keratitis
Corneal injury
Corneal injury is commonly a cause of bacterial keratitis.6 It is widely accepted that contact lens use can cause micro-lesions in the epithelial layer, allowing bacterial entry and colonisation of the Bowman’s membrane and stroma. However, bacterial keratitis is also found in many non-contact lens users, in particular those who work in the farming and agricultural industry. In these cases, it is likely that infection is initiated through incidental entry to the eye. For example, contaminated soil samples taken by the wind, rubbing eyes with unwashed hands and splashes of organic matter have all been identified as causative.7 Bacteria associated with this are typically, but not exclusively, Bacillus and Enterobacteria spp.
Common bacteria associated with bacterial keratitis
Streptococcus species
Streptococci are commonly found in the upper respiratory tract (nose, sinuses and throat) in asymptomatic individuals. The proximity to the eye may account for this pathogen’s role in causing bacterial keratitis, with the most common and aggressive species being S. pneumoniae.
Streptococci are Gram positive and round in shape and penicillin has historically been used to combat infection. However, there is increasing evidence of penicillin-resistance emergence and fluoroquinolones are the current medication of choice.
Infection in the cornea is associated with trauma and chronic dacryocystitis (inflammation of the tear ducts). Patients often present with a deep stromal abscess and plaque formation. Compared with S. pneumoniae, S. viridans is less aggressive and it is associated with crystallinean keratopathy (a condition in which crystals are deposited in the corneal epithelium and/or anterior stroma).8-9
Staphylococcus species
Staphylococcus are common in the normal microbiota of the skin and respiratory tract but in the eye they can typically cause conjunctivitis or ‘pink eye’. They are also the most common bacterium to cause recurrent bacterial keratitis10. Discussion surrounding decolonisation of Staphylococcus aureus from around the eye area has been put forward as a possible solution and as gram positive cocci they are sensitive to a wide range of antibiotics, but the emergence of resistance is rapidly becoming a big problem and the unnecessary use of antibiotics is not recommended11.
Bacillus species
Bacillus cereus are Gram positive anaerobic bacteria found in the soil, natural water sources and vegetation. The infection of the eye is usually associated with corneal injury and occurs within 24 hours resulting in the presence of chemosis (swelling of the conjunctiva) and severe eyelid oedema. There have also been cases of contact lens associated keratitis.12 Isolated colonies are susceptible to aminoglycosides and vancomycin.
Non-tuberculosis Mycobacterium
Non-tuberculosis mycobacteria (NTM) are becoming increasingly common water contaminants and for this reason they are important pathogens in bacterial keratitis. NTMs can invade the cornea after trauma or surgery and the resultant disease is often misdiagnosed for acanthamoebal, fungal or viral infection. This can lead to a severe delay in effective treatments. Amongst the NTM causing bacterial keratitis, M. abscessus is one the most prevalent.13
Pseudomonas species
Pseudomonas is by far the most commonly associated bacteria with eye infection. It is a Gram negative bacterium, which means that different types of antibiotics from those that are effective against the Gram positive bacteria (mentioned above) are needed. Pseudomonas spp. are often associated with contact lens use.
On he cornea, it adheres to damaged epithelium and rapidly invades the stroma. This type of infection can cause a severe diffuse ulcer with a grey, yellow-green discharge, a hypopyon in the anterior chamber, and a severe ocular reaction which may extend to the sclera to cause necrotizing scleritis and/or perforation in two to five days.14
Moraxella species
Moraxella is a normal commensal microorganism of the respiratory tract that can cause disease in immunocompromised individuals. It notably can also cause otitis media and sinusitis. Rarely has it been associated with keratitis but recently UK ophthalmologists have described an increase in incidence.15
Enterobacteriaceae
Enterobacteriaceae are a large family of Gram negative bacteria and many are commensal microbiota of the human host. In the literature, there are several case reports of bacterial keratitis patients hosting these types of bacteria with Serratia marcescens being the primary pathogenic species,16 followed by Klebsiella pneunomiae and enterococcus.17-18 Abnormal corneal surface and contact lens use appear to be the primary risk factors. In older literature, there have also been cases reported of Enterobacter spp. and Proteus spp. causing bacterial keratitis, which supports the view that many enterobacteriaceae may be responsible for corneal infection.
Incidence
Incidence figures for bacterial keratitis alone are difficult to come by, as it is challenging to differentiate between other types of microbial keratitis (acanthamoebal, viral and fungal). This demonstrates the close similarities between different infectious keratitis cases in terms of the symptoms, transmission and ocular impact.
Overall, microbial keratitis is estimated to affect approximately two million individuals worldwide, with variation depending upon different geographical areas.19-20 These locations also correlate with different types of bacteria. For example, infections recorded in Thailand have a higher proportion of Pseudomonas spp., whereas in Paraguay Staphylococcus spp. and Streptococcus spp. have been most prevalent.21-23 In California, a decrease in Streptoccocal and Pseudomonal ulcers has been reported, but numbers linked with Serratia spp. keratitis have increased over the same period of time.23-24 This pattern is also noted in China, with an increase in Staphylococcus spp. and Streptococcus spp. infections and a decrease in Pseudomonas spp. keratitis.25 Therefore, it is evident to see that one solution cannot fit all cases globally, and each geographical location needs to understand the potential of environmental contamination of different pathogens into eye care solutions and contact lenses and direct transmission into the eye.
A comprehensive 12-year study in the UK highlighted that the commensal bacterium Moraxella is being increasingly isolated from microbial keratitis cases, but cases of antibiotic resistance in this group are still reassuringly rare.26
Ocular impact
If untreated, the ocular impact of bacterial keratitis can be severe, requiring surgical procedure to repair the cornea and minimise sight loss. This is life-changing for the patient. The severe reaction is due both to bacterial virulence factors and to the host’s immune response. All pathogens possess virulence (from the Latin word for ‘poisonous’) factors. They allow pathogenic bacteria to cause disease, such as colonisation (adhesion and invasion molecules) of the host and also to evade the immune system that defends the host from infection. Virulence factors are intrinsically linked to the host’s immune response as they constitute molecules (mostly of protein in nature) that the immune response can detect.
Even the immune response that is induced during keratitis can cause damage to the cornea, as it creates inflammation through the production of immunological molecules such as cytokines and chemokines. Cytokines attract more immune cells to the site of infection and the ‘fight’ between immune cell and bacteria/virulence factor can elicit swelling, pain, redness and photophobia). Therefore, on the one hand the immune response is necessary for elimination of the bacteria, but on the other hand severe inflammation in the cornea results from an active immune response.27
Symptoms
- During early infection symptoms include;
- Hyperaemia
- Sensation of sand in the eye
- Pain
- Sensitivity to light
- Excessive tearing
- Blurred vision
- Difficulty keeping eye lids open
A particular feature of bacterial keratitis is its very rapid progression to the complete destruction of the cornea. This can occur between 24 and 48 hours with certain types of bacteria, and it is often associated with corneal ulceration and stromal abscess formation.
Clinical features
Bacteria can invade small lesions in the corneal epithelium, leading to swelling and necrosis of the epithelium and the stroma. At this point, the corneal ulcer starts to form and neutrophils (the first line of immunological defence) are recruited. These produce inflammatory molecules and cytokines that contribute to the necrosis of the stroma. As the infection progresses, other immune cells are recruited which can invade the anterior chamber causing hypopyon, a yellowish pus-like substance visible in the inferior anterior chamber through the cornea. Certain bacteria may also release toxins and proteases that contribute to the pathogenesis process and corneal destruction. If bacteria penetrate the cornea to infect the vitreous humour, the infection becomes full-blown endophthalmitis. 28
Diagnosis
Early diagnosis is essential in order to minimise severe damage and limit ocular impact. Not only is it important to identify what type of infectious agent is causing the microbial keratitis (bacterial, viral, fungal or acanthamoebal), as each infectious agent requires a different type of treatment (bacteria respond to antibiotics, viruses to antivirals and fungi to anti-fungals), but it is also important to identify the actual bacterial strain. This is because certain antibiotics are more potent against some bacteria than others.
Current diagnostic techniques focus on culture methods and molecular diagnostics. In both cases, the diagnostic procedure commences with a corneal scraping. The culture method is a comprehensive identification system of the causative bacterium or multiple types of bacteria and involves allowing the bacteria to grow in optimal media. After culture, bacteria can be stained and subjected to biochemical tests for identification. Furthermore, culturing the bacteria can provide better insight into their antibiotic sensitivities. Unfortunately, despite being the gold standard for diagnosis, the culture method does have its disadvantages. The main one is that its takes up to 14 days to report a culture as negative and this is too long for effective management of bacterial keratitis. For this reason, current protocols rely on first-line broad-spectrum antibiotics to prevent further deterioration.
Molecular diagnostics offers a quicker solution where corneal scrapings undergo polymerase chain reaction (amplification of specific genes or sections of DNA), followed by sequencing to identify the causative agent. This has been well received by diagnostic laboratories, but antibiotic sensitivities cannot be tested.28
Treatment
Broad-spectrum antibiotics are typically used as the first port of call in the treatment of any suspected infection of the eye in order to prevent any potential damage and clear infection as soon as possible.
Fluoroquinolones are the preferred antibiotic of choice, with topical therapy alternating between tobramycin, cetazolin or vancomycin every hour in acute cases. In current practice, fourth generation fluoroquinolines are now being considered. Moxifloxacin and gatifloxacin are preferred as they penetrate the ocular tissue more readily. In 2009, the FDA approved besifloxacin for use in bacterial keratitis for its effectiveness against both Gram positive and Gram negative, as well as anaerobic bacteria. In the UK, oflaxacin is still considered a good first-line antibiotic treatment.26
In some extreme cases of microbial keratitis, corneal perforation can occur, and there is a higher incidence in bacterial keratitis. This can be resolved by either penetrating keratoplasty (PK), sclera-corneal patches or the application of cyanoacrylate tissues. However, whatever the procedure, antibiotics are applied at all times.
The use of antibiotics in the treatment of bacterial keratitis has recently encountered severe obstacles as the emergence of antibiotic resistance correlates with the incidence of the disease. Globally, resistance to fluoroquinolones is becoming more significant and, in the near future, infections may become untreatable with current antibiotics. This is a major obstacle not only in the treatment and successful prognosis of disease, but also in the diagnosis and management of infection. For example, if a suspected bacterial keratitis is treated with broad-spectrum antibiotics and it does not resolve, it could be that another causative agent is responsible (virus, fungus or acanthamoebal) or that the bacteria responsible are already resistant to that particular antibiotic.29-36 Whatever the case, the delay in diagnosis and treatment could have devastating consequences for the patient’s well-being.
Prevention
The risk of bacterial keratitis can be significantly lowered by following simple guidelines for morning and evening routines. Handwashing is the first crucial step in limiting the transfer of bacteria into the eye area. Rinsing contact lens cases thoroughly with clean solution and placing both cases and caps on clean tissue away from water sources (bathroom and kitchen sinks) should always be undertaken.
Recently, a collaboration between the General Optical Council (GOC), the British Contact Lens Association (BCLA), patients and stakeholders was behind the launch of a very successful microbial keratitis prevention campaign called ‘Love Your Lenses Week’.37-39 This year it was from 25-31 March and it trended on social media as #loveyourlenses. As part of the campaign, the BCLA produced a top five of ‘dos and don’ts’ for contact lens care complementing the established and popular ‘No Water’ stickers.38 Although these stickers were designed with Acanthamoeba keratitis in mind, the same principles of transmission apply to bacterial keratitis. There is an obvious link between Acanthamoeba keratitis and bacterial keratitis, as Acanthamoeba that contaminate lenses and cases eat the bacteria that are also present.
Research by the BCLA during ‘Love Your Lenses Week’ revealed some interesting data on levels of awareness among contact lens wearers about potential infection routes. Monthly contact lens case replacement was found to be the least well-known preventative measure amongst contact lens wearers. With 77% of respondents also reporting at least one adverse experience with contact lenses, it is clear that wearer education, awareness and compliance are very important in limiting the risk of bacterial keratitis. In addition, the GOC found that 37% of contact lens wearers swim with their lenses and no goggles, and up to 44% did not know that showering with lenses is not recommended. Bacteria can live in water supplies as can Acanthamoeba, so avoiding water coming into contact with lenses is always the best practice.38-39
All this research taken together signifies that continuous education is very important in ensuring that all contact lens wearers consistently comply with recommended guidelines. Even experienced wearers may become complacent with their contact lens care so reinforcement of messages is essential.
Advice to practitioners
Practitioners are likely to encounter contact lens-related bacterial keratitis, and they play a major role in the education of patients to help prevent microbial keratitis. But in the event of suspected bacterial keratitis, immediate referral to an ophthalmology unit is essential so that swabs and/or scrapings can be taken for bacterial identification and antibiotics be prescribed. In addition, all contact lens types are an associated risk factor, and even daily lenses wearers can also suffer from this infection.
Immediate referral should come before first-line management, although this may often be difficult, as any treatment could mask the cause of infection and make diagnosis difficult. Gaining the trust of contact lens wearers and talking about lens contamination is highly recommended, as in many cases patients are adamant that their contact lens care is impeccable. Maybe it is, but they should still be reminded of how easily bacteria can contaminate even the most cared for lenses and cases.
Fiona L Henriquez is Professor of Parasitology, Infection and Microbiology Group Leader, Institute of Biomedical and Environmental Health Research, University of the West of Scotland
References
- Woese CR, Kandler O, Wheelis ML. Towards a natural system of organisms: proposal for the domains Archaea, Bacteria, and Eucarya. Proceedings of the National Academy of Sciences of the United States of America. 1990;87(12):4576-4579.
- Whitman WB, Coleman DC, Wiebe WJ. Prokaryotes: The unseen majority. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(12):6578-6583
- Sender R, Fuchs S, Milo R (2016) Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol 14(8): e1002533.
- www.mayoclinic.org/diseases-conditions/keratitis/basics/definition/con-20035288
- McLeod SD, LaBree LD, Tayyanipour R, et al. The importance of initial management in the treatment of severe infectious corneal ulcers. Ophthalmology 1995;102:1943–8.
- Eltis M. Contact-lens-related microbial keratitis: case report and review. Journal of Optometry. 2011;4(4):122-127. doi:10.1016/S1888-4296(11)70053-X.
- www.college-optometrists.org/guidance/clinical-management-guidelines/microbial-keratitis-bacterial-fungal-.html
- Galperín GJ, Boscaro G, Tau J, et al. Crystalline keratopathy: an infrequent corneal infection produced by the Streptococcus mitis group. Rev Argent Microbiol. 2011; 43(3):195-7.
- Norcross EW, Sanders ME, Moore QC 3rd, et al. Pathogenesis of A Clinical Ocular Strain of Streptococcus pneumoniae and the Interaction of Pneumolysin with Corneal Cells. J Bacteriol Parasitol. 2011; 2(2):108.
- Kaye R, Kaye A, Sueke H, Neal T, Winstanley C, Horsburgh M, Kaye S. Recurrent bacterial keratitis. Invest Ophthalmol Vis Sci. 2013 Jun 14;54(6):4136-9.
- Feiz V , Redline DE . Infectious scleritis after pars plana vitrectomy because of methicillin-resistant Staphylococcus aureus resistant to fourth-generation fluoroquinolones. Cornea 2007;26:238–40.
- Pinna A, Sechi LA, Zanetti S, et al. Bacillus cereus keratitis associated with contact lens wear. Ophthalmology. 2001; 108(10):1830-4
- Chu HS, Hu FR. Non-tuberculous mycobacterial keratitis. Clin Microbiol Infect. 2013 Mar;19(3):221-6.
- Sy A, Srinivasan M, Mascarenhas J, et al. Pseudomonas aeruginosa keratitis: out comes and response to corticosteroid treatment. Invest Ophthalmol Vis Sci. 2012; 53(1):267-72.
- Mian SI, Malta JB. Moraxella keratitis: risk factors, presentation, and management. Acta Ophthalmol 2011 Mar;89(2):e208-9.
- Parment PA. The role of Serratia marcescens in soft contact lens associated ocular infections. A review. Acta Ophthalmol Scand 1997 Feb;75(1):67-71.
- Bouhenni R, Dunmire J, Rowe T, Bates J. Proteomics in the Study of Bacterial Keratitis. Hecker M, Riedel K, eds. Proteomes. 2015;3(4):496-511.
- Rau G , Seedor JA , Shah MK, et al. Incidence and clinical characteristics of enterococcus keratitis. Cornea 2008;27:895–9.
- Erie JC, Nevitt MP, Hodge DO & Ballard DJ et al. Incidence of ulcerative keratitis in a defined population from 1950 through 1988. Arch Ophthalmol 1993; 111:1665–71.
- Upadhyay MP, Karmacharya PC, Koirala S, Shah DN, Shakya S, et al. The Bhaktapur eye study: ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br J Ophthalmol 2001;85:388–92.1997; 104:1902–9.
- Shah A, Sachdev A, Coggon D, et al. Geographic variations in microbial keratitis:an analysis of the peer-reviewed literature. Br J Ophthalmol 2011; 95:762-7.
- Sirikul T, Prabriputaloong T, Smathivat A, et al. Predisposing factors and aetiologic diagnosis of ulcerative keratitis. Cornea 2008; 27:283–7.
- Bourcier T, Thomas F, Borderie V, et al. Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol 2003;87:834.
- Varaprasathan G, Miller K, Lietman T, et al.. Trends in the aetiology of infectious corneal ulcers at the FI Proctor Foundation. Cornea 2004;23:360–4
- Sun X, Deng S, Li R, et al. Distribution and shifting trends of bacterial keratitis in north China. Br J Ophthalmol 2004;88:165.
- Tan SZ, Walkden A, Au L, Fullwood C, Hamilton A, Qamruddin A, Armstrong M, Brahma AK, Carley F. Twelve-year analysis of microbial keratitis trends at a UK tertiary hospital. Eye (Lond). 2017 Apr 28.
- Robles-Contreras A, Perez-Cano HJ, Babayan-Sosa A, Baca-Lozada O. Bacterial Keratitis Infection: A Battle Between Virulence Factors and the Immune Response, Common Eye Infections, Dr. Imtiaz Chaudhry (Ed.), InTech, 2013 DOI: 10.5772/52264.
- Al-Mujaini A, Al-Kharusi N, Thakral A, Wali UK. Bacterial Keratitis: Perspective on Epidemiology, Clinico-Pathogenesis, Diagnosis and Treatment. Sultan Qaboos University Medical Journal. 2009;9(2):184-195.
- Park SH , Lim JA , Choi JS, et al. The resistance patterns of normal ocular bacterial flora to 4 fluoroquinolone antibiotics. Cornea 2009;28:68–72
- Miller D , Flynn PM , Scott IU , Alfonso EC, et al. In vitro fluoroquinolone resistance in staphylococcal endophthalmitis isolates. Arch Ophthalmol 2006;124:479–83.
- Sueke H , Kaye SB , Neal T, et al. An in vitro investigation of synergy or antagonism between antimicrobial combinations against isolates from bacterial keratitis. Invest Ophthalmol Vis Sci 2010;51:4151–5
- Kaye S , Tuft S , Neal T, et al. Bacterial susceptibility to topical antimicrobials and clinical outcome in bacterial keratitis. Invest Ophthalmol Vis Sci 2010;51:362–8.
- Moshirfar M, Mirzaian G, Feiz V, et al. Fourth-generation fluoroquinolone-resistant bacterial keratitis after refractive surgery. J Cataract Refract Surg 2006;32:515–8.
- Miller D, Flynn PM, Scott IU , Alfonso EC, et al. In vitro fluoroquinolone resistance in staphylococcal endophthalmitis isolates. Arch Ophthalmol 2006;124:479–83.
- Smith A , Pennefather PM , Kaye SB, et al. Fluoroquinolones: place in ocular therapy. Drugs 2001;61:747–61.
- Tello A, Austin B & Telfer TC. Selective pressure of antibiotic pollution on bacteria of importance to public health. Environ Health Perspect. 2011
- www.loveyourlenses.com
- www.optical.org/en/news_publications/news_item.cfm/goc-thanks-optical-industry-and-patients-for-love-your-lenses-support
- www.bcla.org.uk/Public/News/Blog_Posts/Love_your_lenses_Week_25-31_March_2017.aspx
