Optician CooperVision Myopia Series
Part 1: Prevalence and progression – Professor Desmond Fonn
Part 2: What does a good myopia control study look like? Part 1
– Dr Kathy Dumbleton
Part 3: What does a good myopia control study look like? Part 2
– Dr Kathy Dumbleton
Part 4: Why fitting contact lenses in young children is safe?
– Professor Mark Bullimore
Part 5: Three year milestone results in contact lens myopia control
– Dr Paul Chamberlain
Myopia can be defined as a condition of the eye with a spherical equivalent refraction of at least -0.50D that produces poor distance vision. However, the definition of high myopia is rather vague although of more concern because of the associated pathological complications. High myopia in previous studies has been defined as ranging from -5.00 to -12.00D.1
There is agreement that high myopia increases the risk of pathologies such as cataract, glaucoma, retinal detachment and macular degeneration all of which can result in irreversible loss of vision.
Myopia has always been considered as a benign condition that can usually be adequately corrected with spectacle or contact lenses and even though the condition might have progressed regardless of the age of the patient, the usual treatment is simply to increase the negative power of the correcting lenses without much thought about attempting to halt or slow the progression of myopia. One traditional method used to slow myopia progression was to under-correct the myopic error which does not appear to have any retarding benefit but on the contrary, increases the progression.2,3 Bifocal and progressive multifocal spectacle lenses have also been prescribed for years to slow myopia progression and it has been shown in studies that although there is a slowing of myopic progression, the results are clinically insignificant.5-7
The economic burden of myopia is substantial. Holden et al have reported that uncorrected refractive error was the most common cause of distance visual impairment in 2010 affecting over 100 million people globally1 and a large proportion of that is due to myopia. Vitale et al reported the annual cost of correcting refractive error in the United States 10 years ago, was between $3.9 and $7.2 billion.8 The lifetime cost of refractive correction of myopia is considerable which is not limited to corrective appliances. Consideration must also be given to the cost of treating eye disease associated with myopia and managing the visual impairment. There are many lifestyle disadvantages to being myopic and many patients are inconvenienced by having to wear spectacles and contact lenses. Children in particular are self-conscious wearing glasses and are more likely to be bullied than those who do not wear glasses.9 There have been considerable advances in lens design to improve cosmesis but negative lenses particularly in higher powers still generate aberrations and image minification that can cause visual decrement.
Prevalence of Myopia
Myopia prevalence is considered to have reached epidemic levels in many countries. According to Resnikoff et al uncorrected myopia affects over 100 million people (children, adults and the elderly) and is the most common cause of distance visual impairment in the world.10 It is estimated that 1.5 billion people are myopic which means that the world-wide prevalence is approximately 22%.11 It is well established that the prevalence is greater in Asia in general and among East Asian populations but the prevalence in Asia can vary quite considerably12 with the lowest prevalence (0.3%) recorded for a study in Nepal and the highest (96.5%) recorded in South Korea. In addition to reporting on the prevalence of myopia in Asian children and adults from a meta-analysis of 50 population based surveys, Pan et al also reported on the prevalence by age and found that myopia was highest in the 20 to 29 year age group, decreased between 30 and 69 years and then increased again at age 70+.
Jung et al’s epidemiological study of myopia prevalence in 19-year-old male conscripts in South Korea found it to be astoundingly high at 96.5% and the prevalence of high myopia (at least -6.00D) of 21.6% is equally alarming.13 A similarly high result was found in a relatively small group of 47 microscopists in Hong Kong with an age range of 22 to 42 years; 87% were myopic14. They also reported that the average amount of myopia (-4.45D) in this study was higher than the Hong Kong general population.
An important paper to mention is by Holden and colleagues who conducted a meta-analysis of the global prevalence of myopia and projected the change in prevalence to the year 205015. They estimated that 2 billion people were myopic in 2010 and that number would increase to five billion by 2050 and one billion will suffer from high myopia if the current trends continue without any therapeutic intervention. This translates to a staggering 50% of the world’s population who will be myopic by 2050 compared to about 30% currently (figure 1).
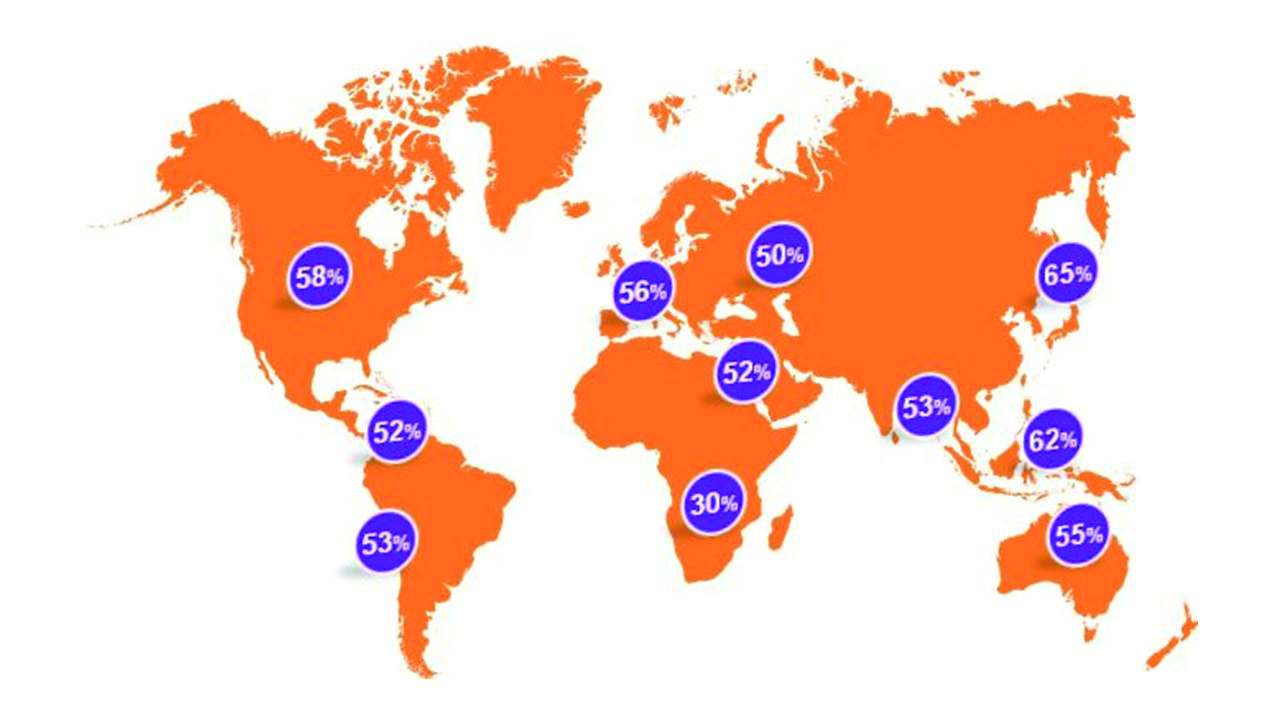
Figure 1: Predicted prevalence of myopia by 2050 (adapted from Holden et al)1
A survey administered among global eye-care practitioners to determine clinical practice attitudes and strategies in managing myopia found that in general, practitioners are reluctant to adopt modern myopia control strategies even though they are moderately concerned about the increased prevalence of myopia. However, ‘Asian practitioners, especially those practicing in China, were more concerned about the increasing prevalence of paediatric myopia in their practices than clinicians in any of the other continents,’ according to Wolffsohn and colleagues.16 This is not entirely surprising given the well-publicised fact that greater prevalence of myopia exists in Asia. Asian ethnicity also appears to be a strong risk factor of myopia development for Asians residing in other countries. In an Australian study of children aged 11 to 15 in Sydney, they found that there was a much higher prevalence of myopia among East Asian students than the European Caucasians. The proportion of East Asians with myopia was 39.5% versus only 4.6% European Caucasians.17
Relatively high prevalence has also been reported for some western countries. For example, Vitale and co-workers reported in 2009 that the prevalence for persons aged 12 to 54 years in the United States increased from 25% in 1971-72 to 41.6% in 1999-2004 for the same age group for black and white individuals and for all severity levels of myopia. Although Vitale found that the prevalence of high myopia (defined as greater than -6.00D) is much lower, the 30-year increase was eightfold.18
Several studies on myopia prevalence have been conducted in Europe. In the United Kingdom Logan and co-workers found half of the 373 students aged 19.6 years (range 17 to 30 years) were myopic but in this case, there was no difference between white and British Asian students.19 A subsequent study reported by Logan and colleagues in 2011 on two groups of children aged six to seven and 12-13 years in Birmingham, UK found prevalence rates of 9.4% and 29.4% for the two groups respectively. In this case, there were significant ethnicity differences in the older group; 36.8% prevalence for the Asians and 18.6% prevalence for the white Europeans.20 Kleinstein also found a higher prevalence among Asian children than whites.21 The Northern Ireland Childhood Errors of Refraction (NICER) study was conducted on school children aged six to seven and 12-13 years. There was an eight-fold difference in myopia prevalence between the younger and older children (2.8% and 17.7% respectively) [22], somewhat lower than the Logan et al report.
Progression of Myopia
Progression has several connotations. Progression can relate to temporal changes of myopia for individuals or groups. It is well established that the increase in severity of myopia occurs in childhood. For example, McCullough and colleagues reported that the proportion of myopic children in the UK aged 10 to 16 years in 1960 was 7.2% and that increased by more than double to 16.4% for 12 to 13-year-olds in the study period 2006-2008.23 They also suggested that white children are becoming myopic at an earlier age. Lin and colleagues studied the prevalence of myopia of Taiwanese school children from 1983 to 2000. They found that the onset of myopia occurred at an earlier age in 2000 compared to 1983 and the severity increased for all age groups between those time frames as well. For example, in 2000, myopia of eight-year-olds was -0.15 ±1.40D and 18-year-olds was -3.64 ± 2.41D. Whereas in 1983 the mean value for eight-year-olds was +0.45 ±1.03D and 18-year-olds was -2.55 ±2.55D.24 They concluded that the progressively increasing severity of myopia occurred as a result of children becoming myopic at a younger age. Holden and colleagues also stated that earlier onset could result in a more rapid progression leading to higher myopia which increases the risk of associated eye disease25 (figure 2). Saw et al studied factors related to myopia progression of Singaporean children and concluded that myopia progression was faster for younger children and those who had higher myopia at younger ages.26 Williams and colleagues reported on a temporal increase of myopia but with different subjects. Those born between 1910 and 1939 had a prevalence of 17.8% compared to 23.5% for those born between 1940 and 1979.27
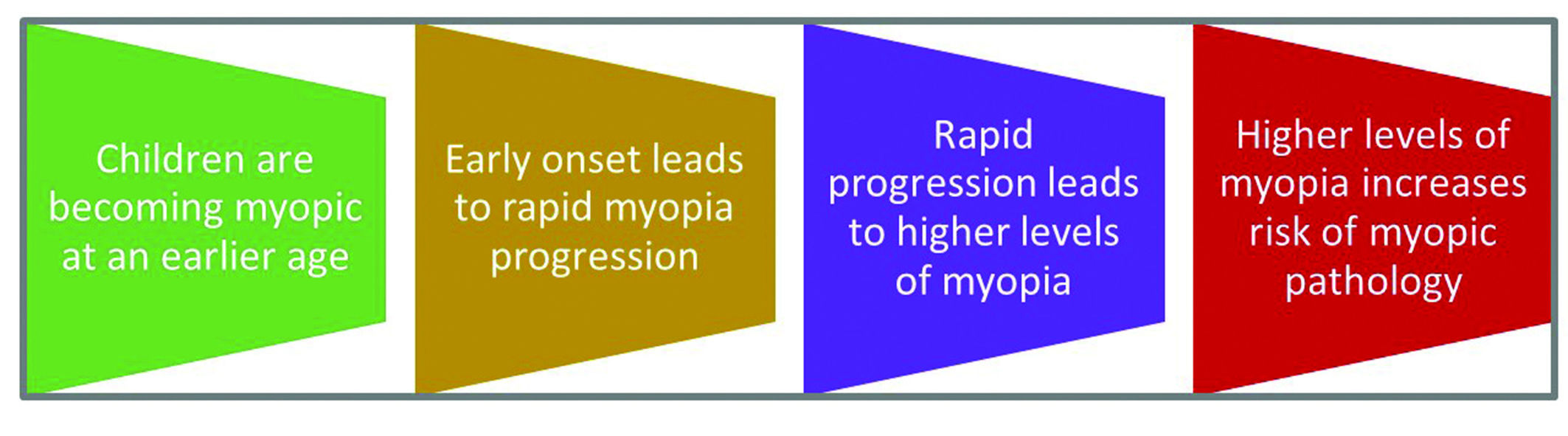 Figure 2: Progression of myopia
Figure 2: Progression of myopia
The most worrying aspect about progression is the increase in number of patients who fall into the category of high myopia8 and the alarming projected number by Holden et al.1 They projected that one billion people (10% of the world’s population) will have high myopia by the year 2050 if myopia control strategies are not instituted on a global scale. This seems unlikely as there are already well-established clinical methods to retard the progression of myopia by at least 50%28,29 (figure 3). But as Wolffsohn et al pointed out, the majority of practitioners prescribe single vision lenses to correct myopia for young people16 because they are either unconvinced that myopia controlling procedures are sufficiently established or are not confident or sufficiently schooled in these procedures.
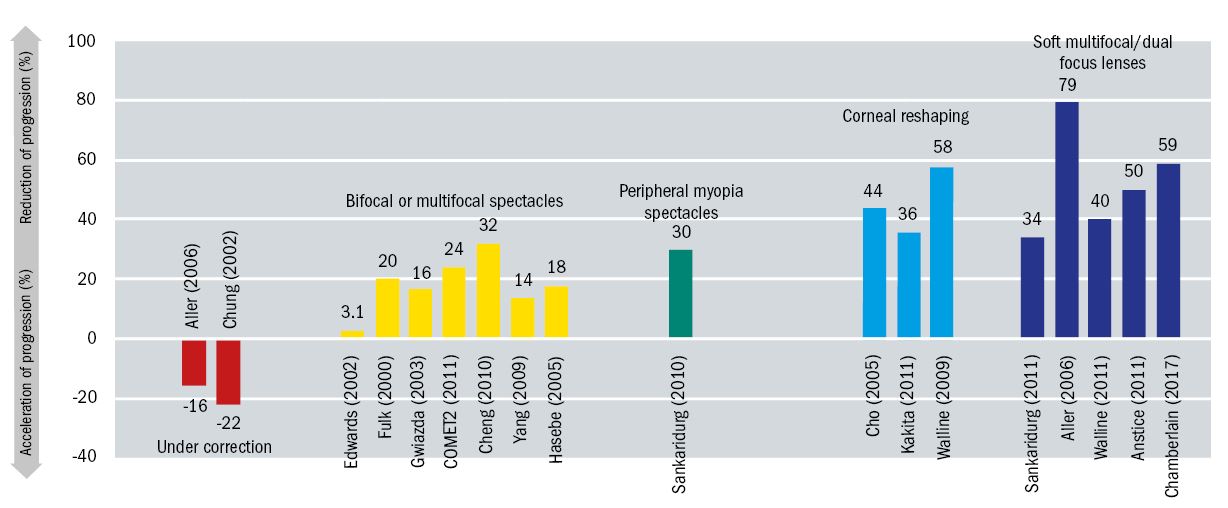 Figure 3: Effectivity of a range of myopia control strategies showing percent reduction in spherical equivalent refractive error (SERE) (Adapted from Walline J, Myopia Control: A Review 2016.)
Figure 3: Effectivity of a range of myopia control strategies showing percent reduction in spherical equivalent refractive error (SERE) (Adapted from Walline J, Myopia Control: A Review 2016.)
Myopia risk factors: Genetics versus environment
Genetics is an established risk factor of myopia development. The risk of becoming myopic increases approximately five-fold if both parents are myopic compared to children who only have one or no myopic parents.30-32 However, there is as strong an influence on myopia development by the environment in which school aged children live and study.33 Rudnicka and colleagues conducted a meta-analysis of population-based surveys of the prevalence of childhood myopia. They concluded that the risk of myopia is greater in urban settings and that environmental factors play an important role in the development of myopia.34 Related to the environmental factor is the near work or amount of time that children spend on tasks at near distance. On this there is debate: on the one hand, prolonged near tasks appear to increase the risk of myopia development17 whereas Rose who studied Chinese children in Singapore and Sydney, Australia found that there was a significantly lower prevalence of myopia in the Australian children than the Singaporean children even though the children in Sydney spent much more time on near activity.35 In this study Rose also found that the Sydney children spent considerably more time outdoors than the children in Singapore and there is growing evidence that increased time spent outdoors is protective of myopia development.36,37 Xiong et al’s meta-analysis revealed a protective effect of light exposure on the development of myopia but not on the progression of myopia in those who were myopic.38 And Tideman et al’s study of 5,711 six-year-olds in the Netherlands found that environmental factors (eg less time outdoors and lower vitamin D) were strong risk factors for myopia development.39
Myopia: Moving from correction to treatment
The Holden et al projections1 are frightening, if myopia control strategies are not widely employed. Vitale and colleagues18 have shown that there has been an eight-fold increase in the number of high myopes in the United States over the past 35 years and by using Holden’s projections Vitale’s number is likely to almost double in the next four years. High myopia is enough of a clinical concern without the secondary ocular health complications, which will inevitably arise because of presumed structural changes to the eye resulting from increased axial length. The concomitant complications of retinal detachment, glaucoma, cataract and macula degeneration all contribute to high or pathological myopia as a leading cause of visual impairment and blindness. Liu and co-workers found that of the three major causes of visual impairment in an elderly Taiwanese population, the proportion of high myopic macular degeneration was 25%40 and in Japan, myopic maculopathy has been documented as the highest cause of monocular blindness.41 Similar findings of myopic morbidity have been found in other countries.42-44 Holden et al estimate there will be a seven-fold increase of people with vision loss by 2050 from 2000 assuming the proportion of high myopes with vision loss remains the same as current figures. This means that high myopia could be the leading cause of blindness by 2050.1
Low myopia is also not immune from vision loss. Flitcroft has suggested that physiological myopia is a misnomer45 as even low myopia (<5.00D) is associated with myopic retinopathy although the prevalence (0.42%) is exponentially lower than myopia greater than 9.00D (prevalence >50%) as shown by Vongphanit et al.46 Using these data Morgan has calculated that ‘for each 1.00D of reduction of myopia there is a 42% reduction in the prevalence of myopic retinopathy’.47 Brennan has applied similar logic to determine predicted prevalence of myopia by reducing the rate of myopia progression by 33%. This could reduce the number of myopic eyes (>-5.00D) by 73%.48 In an editorial authored by Holden and colleagues, they concluded that retarding the progression of myopia by 50%, if treatment is commenced at the age of seven, would result in about 90% fewer high myopes (5.00D or more) which would have a marked reduction on the risks of sight-threatening complications in later life.49 There is little doubt that myopia control is a viable therapeutic procedure to employ immediately as shown by Smith and Walline28 where all three strategies (atropine, orthokeratology and soft lens bifocals) retard myopia progression by about 50%. New technology presented by Chamberlain showed a 59% reduction of myopia progression with a dual focus one day soft contact lens.50 A review by Sankaridurg includes a graphic that compares the relative myopia control percentages for outdoor exposure, atropine, orthokeratology, soft contact lenses and spectacles. It appears that atropine has the largest effect followed by orthokeratology and soft lenses but one of the disadvantages of atropine is the rebound effect when treatment is discontinued. However, this phenomenon has not been studied in soft contact lens wearers.51
The economic burden of myopia has been described earlier and these costs do not account for the pathological complications associated with high myopia. With the projected increase in prevalence of high myopia and resultant increase in pathology, there will be considerable economic hardship to treat the eye disease, visual impairment and blindness over the next few decades. As people’s life spans will also be extended, the economic burden on individuals and society could become enormous. These are good reasons to begin therapeutic treatment of myopia in children to retard progression. Reducing the prevalence of myopia is much more challenging because etiology is still uncertain. However, exposing children to more time outdoors does seem to reduce the prevalence.38,39,52
Pressure from myopic parents and those who are not myopic but concerned enough about their children becoming myopic will likely influence eye care practitioners to start practicing myopia control. There is an abundance of lay information and there are many myopic eye care practitioners who must be sufficiently concerned about their own children to change their mode of practice from correction to prevention and therapeutic treatment of myopia.
Professor Des Fonn is Distinguished Professor Emeritus and the founding director of the Centre for Contact Lens Research at the School of Optometry and Vision Science, University of Waterloo.
This article is adapted from one published in Life Through a Lens (CCLS Australia), December 2016. This series was commissioned by CooperVision.
References
- Holden BA, Fricke TR, Wilson DA et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016; 123:1036-42.
- Chung K, Mohidin N, O’Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res. 2002; 42:2555-9.
- Adler D, Millodot M. The possible effect of undercorrection on myopic progression in children. Clin Exp Optom. 2006; 89:315-21.
- Smith T, Frick K, Holden B, et al. Potential lost productivity resulting from the global burden of uncorrected refractive error. Bull World Health Org 2009; 87:431-7.
- Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci 2003; 44: 1492-1500.
- Fulk GW, Cyert LA, Parker DE. A randomized trial of the effect of single vision vs bifocal lenses on myopia progression in children with esophoria. Optom Vis Sci 2000; 77:395-401
- Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci. 2012; 53:640-9.
- Vitale S, Cotch MF, Sperduto R, Ellwein L. Costs of Refractive Correction of Distance Vision Impairment in the United States, 1999-2002. Ophthalmology 2006;113(12):2163-70.
- Horwood J, Waylen A, Herrick D, et al. Common visual defects and peer victimization in children. Investigative Ophthalmology and Visual Science. 2005;46:1177-81.
- Resnikoff S, Pascolini D, Mariottia SP, et al. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ 2008; 86:63-70
- Holden BA, Sankaridurg P, Smith E et al Myopia, an underrated global challenge to vision: where the current data takes us on myopia control. Eye (2014) 28, 142-146
- Pan C-W, Dirani M, Cheng C-Y, et al. The age-specific prevalence of myopia in Asia: a meta-analysis. Optom Vis Sci. 2015; 92:258-66
- Jung SK, Lee JH, Kakizaki H, et al. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Invest Ophthalmol Vis Sci. 2012; 53:5579-83
- Ting PWK, Lam CSY, Edwards MH, et al. Prevalence of myopia in a group of Hong Kong microscopists. Optom Vis Sci. 2004;81(2):88-93
- Holden BA, Fricke TR, Wilson DA et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016; 123:1036-42
- Wolffsohn JS, Calossi A, Cho P, et al. Global trends in myopia management attitudes and strategies in clinical practice. Cont Lens Anterior Eye. 2016; 39:106-16
- Ip JM, Huynh SC, Robaei D, et al. Ethnic differences in refraction and ocular biometry in a population-based sample of 11-15-year-old Australian children. Eye (Lond) 2008; 22:649-56.
- Vitale S, Sperduto RD, Ferris FL 3rd. Increased Prevalence of Myopia in the United States Between 1971-1972 and 1999-2004. Archives of Ophthalmology. 2009;127(12): 1632-9.
- Logan NS, Davies LN, Mallen EAH, Gilmartin B. Ametropia and ocular biometry in a U.K. university student population. Optom Vision Sci. 2005;82(4):261-6
- Logan NS, Shah P, Rudnicka AR. Childhood ethnic differences in ametropia and ocular biometry: the Aston Eye Study. Ophthalmic Physiol. Opt. 2011; 31(5):550-8.
- Kleinstein RN, Jones LA, Hullett S et al. Refractive error and ethnicity in children. Arch Ophthalmol. 2003; 121:1141-7.
- O’Donoghue L, McClelland JF, Logan NS, et al. Refractive error and visual impairment in school children in Northern Ireland. Br J Ophthalmol. 2010; 94:1155-9.
- McCullough SJ, O’Donoghue L, Saunders KJ. Six Year Refractive Change among White Children and Young Adults: Evidence for Significant Increase in Myopia among White UK Children. PloS one. 2016; 11:1-19
- Lin LL, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore 2004; 33:27-33.
- Holden BA, Sankaridurg P, Smith E Et al. Myopia, an underrated global challenge to vision: where the current data takes us on myopia control Eye (2014) 28, 142-146
- Saw SM, Nieto FJ, Katz J Et al. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. 2000; 77:549-54.
- Williams KM, Bertelsen G, Cumberland P, et al. Increasing prevalence of myopia in Europe and the impact of education. Ophthalmology. 2015; 122:1489–97.
- Smith MJ, Walline JJ. Controlling myopia progression in children and adolescents. Adolesc Health Med Ther. 2015; 6:133-40.
- Smith EL. Prentice Award Lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011; 88:1029-44.
- Morgan I, Rose K. How genetic is school myopia? Prog Retin Eye Res 2005; 24:1-38
- Jones-Jordan LA, Sinnott LT, Manny RE,et al; Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group. Early childhood refractive error and parental history of myopia as predictors of myopia. Invest Ophthalmol Vis Sci 2010; 51:115-21.
- Zadnik K. The Glenn A. Fry Award Lecture (1995). Myopia development in childhood. Optom Vis Sci 1997; 74:603-8.
- Mutti DO, Zadnik K, Adams AJ. Myopia. The nature vs. nurture debate goes on. Invest Ophthalmol Vis Sci 1996; 37:952–7.
- Rudnicka AR, Kapetanakis VV, Wathern AK et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016; 100:882-890
- Rose KA. Myopia, Lifestyle, and Schooling in Students of Chinese Ethnicity in Singapore and Sydney. Archives of Ophthalmology. 2008; 126:527–30.
- Rose KA, Morgan IG, Ip J et al. Outdoor activity reduces the prevalence of myopia in children.Ophthalmology 2008;115:1279-85
- Read SA, Collins MJ, Vincent SJ. Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci 2014; 91:330-41.
- Xiong S, Sankaridurg P, Naduvilath T et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017; 95:551-566
- Tideman JWL, Polling JR, Hofman A et al. Environmental factors explain socioeconomic prevalence differences in myopia in 6-year-old children. Br J Ophthalmol. 2017 [Epub ahead of print]
- Liu JH, Cheng CY, Chen SJ, Lee FL. Visual impairment in a Taiwanese population: prevalence, causes, and socioeconomic factors. Ophthalmic Epidemiol. 2001; 8:339–50
- Iwase A, Araie M, Tomidokoro A, et al. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology 2006; 113:1354-62.
- Hsu W-M, Cheng C-Y, Liu J-H, et al. Prevalence and causes of visual impairment in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmolgy. 2004; 111:62–9.
- Cedrone C, Culasso F, Cesareo M, et al. Incidence of blindness and low vision in a sample population: the Priverno Eye Study, Italy. Ophthalmology. 2003; 110:584–8.
- 44 Evans JR, Fletcher AE, Wormald RPL, MRC Trial of Assessment and Management of Older People in the Community. Causes of visual impairment in people aged 75 years and older in Britain: an add-on study to the MRC Trial of Assessment and Management of Older People in the Community. Br J of Ophthalmol. 2004; 88:365–70.
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res 2012; 31:622-60
- Vongphanit, J., Mitchell, P., Wang, J.J. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology 2002;109: 704-711
- Morgan P Is myopia control the next contact lens revolution? Optician 2016
- Brennan NA. Predicted reduction in high myopia for various degrees of myopia control. Cont Lens Anterior Eye. 2012;35 S1: e14.
- Holden BA. Guest Editorial: Nearly 1 billion myopes at risk ofmyopia-related sight-threatening conditions by 2050 – time to act now. Clin Exp Optom 2015; 98: 491–493
- Chamberlain P Et al. Clinical evaluation of a dual focus myopia control 1 day soft contact lens – 3 year results BCLA June 2017
- Sankaridurg P. Contact lenses to slow progression of myopia. Clin Exp Optom. 2017 [Epub ahead of print]
- Dirani M, Tong L, Gazzard G, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009; 93:997–1000.
