While all surgery requires a high level of precision and accuracy of tissue manipulation, ophthalmic surgery is especially demanding on account of the miniscule scale of the tissue structures encountered. Within the scope of ophthalmic surgery, the limitations of hand tremour and degree of control over highly demanding tissue manipulations can limit the scope of procedures possible. In addition, there is increasing awareness of the significant risk of occupational musculoskeletal injuries among surgeons, especially resulting from minimally invasive surgery, where surgeons have restricted freedom of movement and have to maintain postures for extended periods.1,2 Such injuries can present significant challenges for surgeons, necessitating extended periods of sick leave for recovery and with an associated loss of clinical operating capacity. Some observers indicate there may a role for robotic techniques to reduce the physical strain associated with such challenging surgical techniques.
While the term ‘robotic surgery’ is generally applied in the context of a surgeon remotely operating an instrument system within the patient, ‘robotic’ developments can also include specific ‘smart’ instruments which have superior levels of function through, for example, software interface control.
The Surgical Robot Marketplace
Currently, Intuitive Surgical (the company which has developed the da Vinci robot) has a virtual monopoly of the technology behind surgical robots. By the end of 2016, around 3,600 systems were in place around the world, of which around 60 are located in the UK. Such surgical robots represent a significant capital investment of over £1 million per system and require a training process for surgeons that is highly demanding and requires significant resourcing. Currently, the priority in surgical techniques is to develop such systems for minimally invasive surgery, where recovery periods from such surgery are reduced and superior clinical outcomes are able to be demonstrated.
Recently, a range of competitors have sprung up within the surgical robot marketplace to challenge the dominance of Intuitive Surgical. One of these is Verb Surgical (operating as a joint venture between Johnson & Johnson’s Ethicon and Google’s Alphabet’s Verily Life Sciences). Such a coalition combines Ethicon’s knowledge of surgical instruments and Google’s machine vision, imaging analysis, and data analytics expertise. A range of mainstream medical device manufacturers have also identified robotic developments in neurological/spinal column surgery as a specific area for acquisitions. Activity in this area has come from a number of companies, such as Medtronic acquiring Mazor Robotics and Zimmer Biomet acquiring Medtech SA.
Lines of Development
The existing surgical robot technology, in the guise of the da Vinci robot system, has been assessed for suitability for eye surgery by Bourla et al.3 Specific issues, however, were identified in relation to visualisation of the surgical field and also levels of stress at entry points of operating instruments which indicated that its use for ophthalmic surgery was not appropriate.
While research is ongoing at the level of the large corporation, developments in the field of surgical robots is also being undertaken within a wide range of biomedical research establishments. One line of development of next generation surgical ‘robotic’ devices has been undertaken at Kings College London and other centres within the STIFF-FLOP (STIFFness controllable Flexible and Learnable Manipulator for Surgical Operations programme). This was an EC-funded programme within the FP7-ICT (‘Specific Programme “Cooperation”: Information and communication technologies’ initiative). This has developed the ‘soft’ robotic arm which is capable of precision movements and sensory feedback while retaining configuration integrity such as demonstrated by an elephant trunk or the arm of an octopus.4,5 The functionality of this system has been demonstrated as a flexible light source/camera system, where the safety of laparoscopic procedures is enhanced by improved vision of surgical field. This specific approach is designed to overcome the restrictions of conventional robot systems where processes of manipulation are determined by a rigid array of instruments.
A common approach in the development of robotic techniques in ophthalmic surgery physically separates the patient from the surgeon, as is the practice in conventional robotic surgery. This process is described as a master-slave configuration,6 where the set of instruments in the eye follows the remote directions from the surgeon.
Advantages of such a system potentially include:
- a more sustainable and comfortable body posture
- intuitive handling of instruments
- reduced instrument movements
- provision of effective force feedback
- rejection of hand tremour.
This system, therefore, has the potential for reducing stress on the surgeon, where in conventional techniques there is the requirement for continuous precise control/manipulation/placement of all of the surgical instruments involved in surgery. Such a system would include an instrument changing facility to allow rapid removal/insertion of surgical tools. A key challenge, however, in this configuration is the development of an appropriate sensory feedback system, such as might be needed to communicate to the remote surgeon details of the force exerted by surgical instruments on the surface of the retina.
Specific Ophthalmic Uses
Microsurgery of the retina is utilised in the management of a range of diseases of the retina which include retinal vein occlusion, diabetic retinopathy, retinal detachment, macular degeneration and management of an epiretinal membrane (figure 1). In the process of peeling of an epiretinal membrane, the inclusion of additional degrees of freedom at the active tool tip used for the delamination process is identified as beneficial to the procedure, in contrast to having to change the peeling angle of the active tip with fixed angle devices.
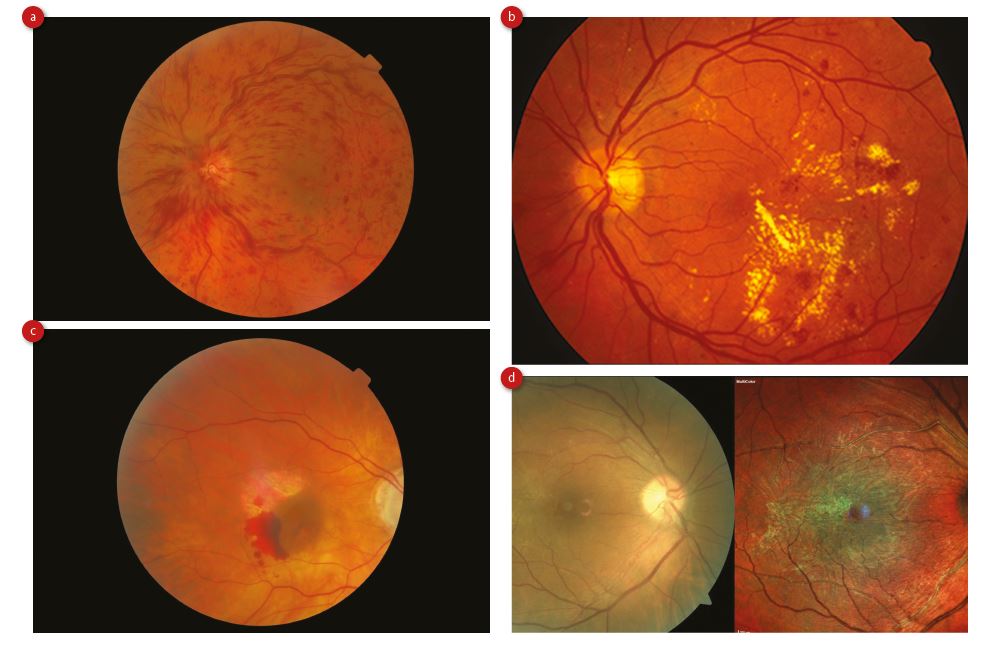 Figure 1: Conditions for which robotic microsurgical techniques have been developed to treat; (a) retinal vein occlusion, (b) diabetic retinopathy, (c) macular degeneration with pre-retinal haemorrhage and (d) an epiretinal membrane (image d courtesy of Heidelberg UK)
Figure 1: Conditions for which robotic microsurgical techniques have been developed to treat; (a) retinal vein occlusion, (b) diabetic retinopathy, (c) macular degeneration with pre-retinal haemorrhage and (d) an epiretinal membrane (image d courtesy of Heidelberg UK)
In treatment of retinal vein occlusion, a therapeutic agent is injected into the vein using a micropipette where the procedure would be simplified if the angle of access of the micropipette could be dynamically altered during the cannulation process (as described by Ergeneman et al7). This procedure is one of the most challenging within vitreoretinal surgery. One approach of achieving this level of instrument tip control is that of the IRIS (Integrated Robotic Intraocular Snake) project,8 where a stack of segmented elements can be controlled through tension in support wires to angle the stack through a specific angular displacement. It is proposed that a series of ‘snap on’ tools are attached to the tip of the device to provide the additional degrees of freedom required. The diameter of the active tip element would be less than 0.9mm and its length 10mm with an angular displacement of ±45˚. The IRIS system has so far been demonstrated as a scaled up system but not developed as a surgical prototype.
Eye Robot
A group at John Hopkins Hospital in Baltimore has been active developing surgical robot systems in ophthalmology. Initial work to develop Eye Robot 1 (by Iordachita et al9) focused on an operating instrument arm with specific degrees of freedom. As an evolution of this, Eye Robot 210 has been developed which increases the relative modes of movement of the instrument arm and incorporates a highly sensitive force sensing arm to allow modification of surgical technique based on sensed forces at the tool tip. The software used to drive the system utilises a specific software package known as the Surgical Assistant Workstation.11 This force-sensing feature applied by surgical instruments is a key feature of various eye surgery robot developments, as described by Sun et al.12
A novel feature of Eye Robot 2 is the inclusion of optical fibre Bragg gratings (FBGs) to detect force at the instrument tip. Force is communicated to three fibre Bragg gratings via a hooked instrument tip which allows force in a given plane to be measured with a sensitivity of 0.25milliNewtons (mN) and within the range 0mN to 60mN. This allows the operator to be aware of any force exerted on a surface during a cutting procedure and where, using a control algorithm, a limit of 7mN is set which sounds an audible alarm if exceeded.
This was shown to allow the safe completion of tasks simulating stripping membranes from the retina where, when rising force levels were encountered, it was possible to complete the cutting process by selecting areas of reduced contact force. Current techniques of membrane removal from the retina rely largely on visual cues rather than any element of force sensing. The authors also describe upgrading various of the mechanical components within Eye Robot 1 to higher specification elements in Eye Robot 2 and employing linear and rotary control elements sourced as readily available devices from within the robotics industry.
Visual Feedback
Yu et al13 describe a system for real-time intraocular optical coherence tomography (OCT) visualisation of the operating field of ophthalmic surgical instruments. In this mode, a key feedback parameter is the depth of penetration of the operating tool (23 gauge) on the retinal surface. This technique takes advantage of the compact features of optical fibres to provide real time OCT image feedback.
A World First in Oxford
On September 12, 2016, Robert MacLaren, Professor of Ophthalmology at Oxford’s John Radcliffe Hospital used the PRECEYES R2D2 Surgical System to initiate a retinal membrane peel. The specific PRECEYES R2D2 Surgical System (developed by the Dutch company Preceyes BV) provides a means of guided manipulation of the active surgical tool, one where hand tremor is essentially eliminated.
The Preceyes BV company evolved from PhD projects undertaken at the University of Eindhoven and an earlier reference to their development14 indicates the area of technology which was being investigated. This first use of such robotic technology is an important step in the further development of ophthalmic surgery. A key goal of the current robotic use in Oxford is the evaluation of the system for precision injection of stem cells into the retina as a treatment for diseases such as retinitis pigmentosa (figure 2). This specific research is being funded by NIHR Oxford Biomedical Research Centre.
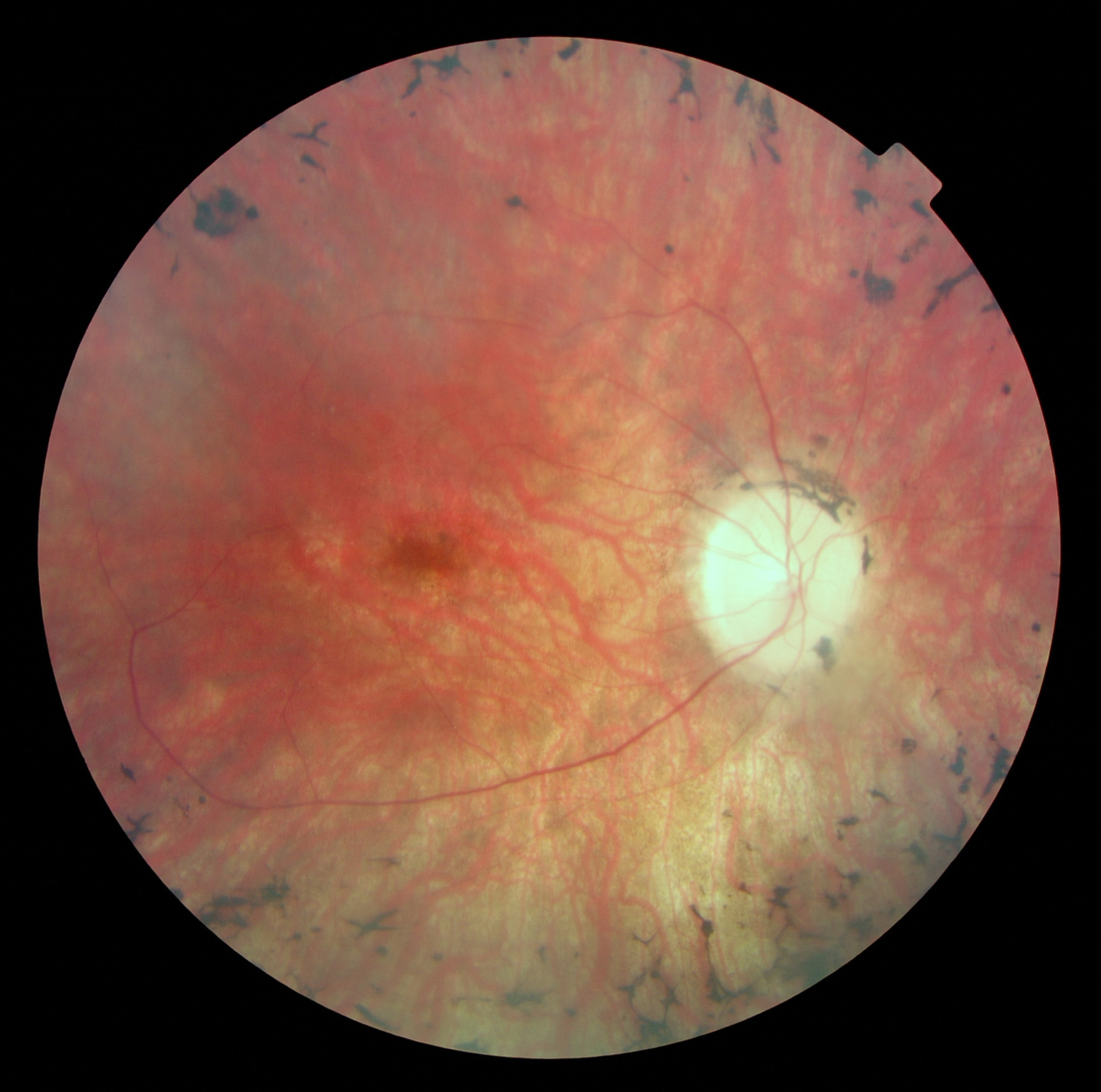
Figure 2: Robotic techniques have been developed to inject stem cells to treat retinitis pigmentosa
By the end of December 2016, a total of six operations demonstrating the macular peeling procedure using the PRECEYES R2D2 system had been successfully completed. In addition, in December 2016, Professor MacLaren used the PRECEYES R2D2 Surgical System to deliver a subretinal tPA injection to treat a subretinal haemorrhage. This was again a world’s first using robotic assistance for prolonged delivery of a drug in the eye. The procedure was carried out under local anaesthesia.

Figure 3: View of operating field: PRECEYES robot arm system in use at John Radcliffe Hospital, Oxford (image by permission of Eye Research Group, Oxford)
When operating with the current system, the surgeon still observes the surgery through the operating microscope, though the instrument is controlled by means of the robotic hand controls which allow precision control of the operating tip. This reduces the postural stress of the surgeon. Also, the instrument can be withdrawn to a safe ‘holding’ position, which allows the surgeon to rest during a lengthy procedure. The current system does not currently provide any ‘force feedback’ to the surgeon.
Such robotic systems such as the PRECEYES R2D2 system have the ability to record all control manipulations of the surgical instruments. This provides the potential to associate such movements with the ‘quality’ of such surgery, so allowing the identification of ‘successful’ and ‘risky’ manoeuvres. This has the potential to provide a surgical ‘co-pilot’ facility.
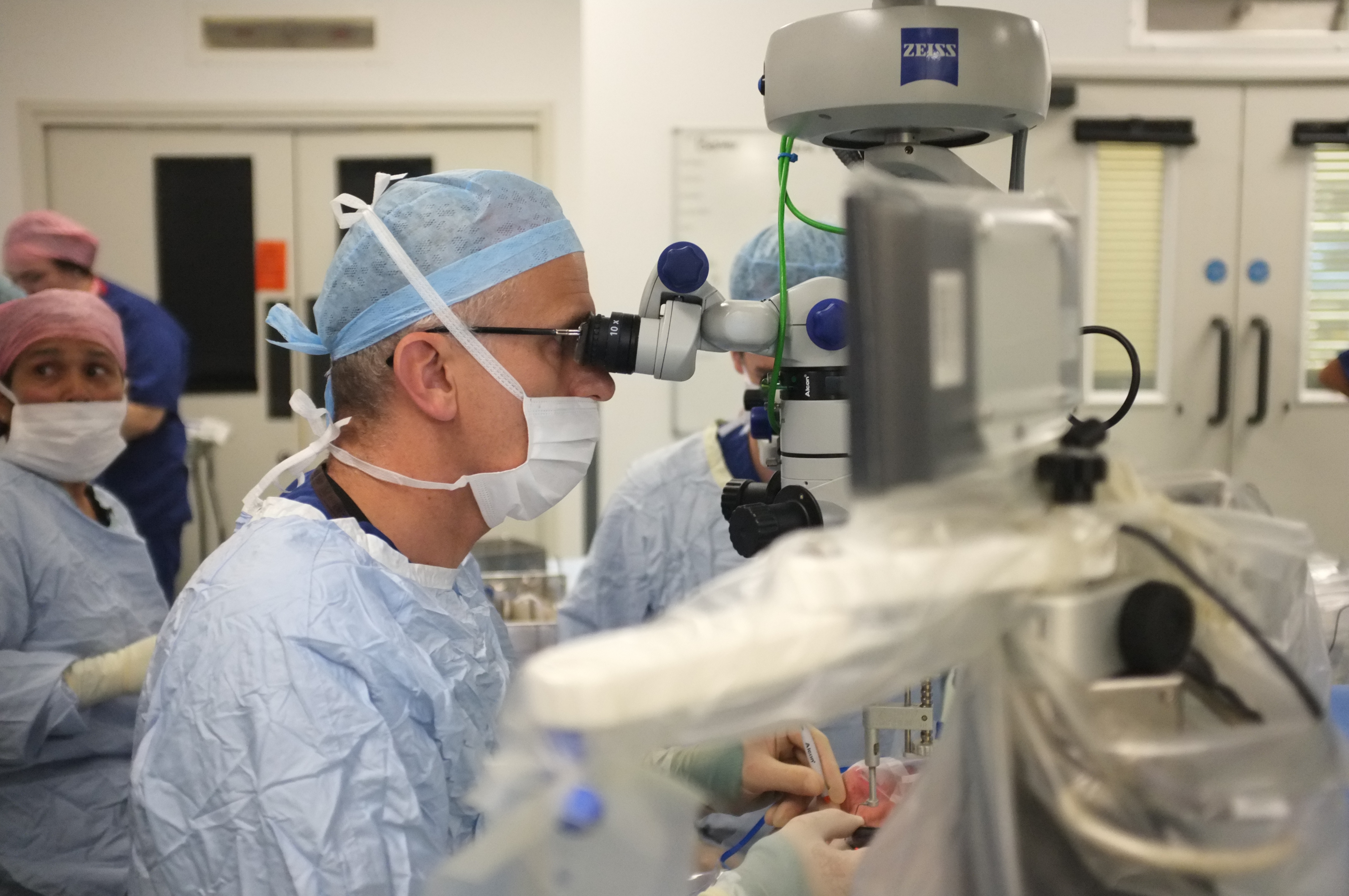 Figure 4: Surgeon operating view: PRECEYES robot arm system in use at John Radcliffe Hospital, Oxford (image by permission of Eye Research Group, Oxford)
Figure 4: Surgeon operating view: PRECEYES robot arm system in use at John Radcliffe Hospital, Oxford (image by permission of Eye Research Group, Oxford)
Currently, the Rotterdam Eye Hospital and the Rotterdam Ophthalmic Institute have signed a co-operative agreement with Preceyes BV to further develop microsurgical techniques. A separate collaborative venture has also been recently signed with the Rigshospitalet in Copenhagen, where the PRECEYES R2D2 surgical system will be used in conjunction with the EyeSi virtual reality training system.
The EurEyeCase Consortium
In Europe, the EurEyeCase Consortium15 has been established to provide co-operative development in the field of robotic surgery in ophthalmology and includes academic partners in the University of Leuven, the Technical University of Eindhoven and ETH Zurich. Medical device manufacturers include Preceyes BV, OptoMedical Technologies GmbH and Medical Laser Center Lubeck, where the latter two offer OCT imaging expertise.
In addition, clinical expertise will be provided by University Hospital Leuven, University of Milan and Rotterdam Eye Hospital.
The key aims of the initiative are to develop robotic techniques for procedures relating to epiretinal membrane and retinal vein occlusion. Specific goals for removal of the epiretinal membrane include limiting forces to 7.5mN and ensuring that instrument motion does not exceed 80µm/s in order to avoid retinal tear.
Conclusion
It is difficult to predict the likely rate of uptake of surgical robot systems in ophthalmology. What ophthalmologists are anticipating is the clinical trial data from pilot sites where robotic technologies are used so that there can be a comparison of outcomes between conventional techniques and the innovative robot approach. Surgical robots may also be able to assist in improving the productivity of operating theatres, where elements of surgical operations may be able to be safely ‘speeded up’. There are, however, potentially significant issues which should not be underestimated, relating to the training of theatre staff to manage/configure such specialist equipment items.
There are also potential issues relating to the cleaning/sterilisation of such delicate robotic devices, where conventional mass process techniques for conventional surgical instruments are probably not appropriate. Also, while systems with the technical capabilities of force sensing and OCT imaging have been developed, these have yet to be demonstrated in a clinical environment.
Dr Douglas Clarkson is development and quality manager at the department of clinical physics and bio-engineering, Coventry and Warwickshire University Hospital Trust
References
- Gutierrez-Diez MC, Benito-Gonzalez MA, Sancibrian R, Gandarillas-Gonzalez MA, Redondo-Figuero C, Manuel-Palazuelos JC. A Study of the Prevalence of Musculoskeletal Disorders in Surgeons Performing Minimally Invasive Surgery. Int J Occup Saf Ergon. 2017;1-19. doi: 10.1080/10803548.2017.1337682
- Janki S, Mulder EEAP, IJzermans JNM, Tran TCK. Ergonomics in the operating room. Surgical Endoscopy. 2017;31(6):2457-2466. doi:10.1007/s00464-016-5247-5
- Bourla DH, Hubschman JP, Culjat M, Tsirbas A, Gupta A, and Schwartz SD, Feasibility study of intraocular robotic surgery with the da vinci surgical system, Retina. 2008; 28(1):154-158
- Arezzo A, Mintz Y, Allaix ME, Arolfo S, Bonino M, Gerboni G, Brancadoro M, Matteo Cianchetti M, Menciassi A, Wurdemann H, Noh Y, Althoefer K, Fras J, Glowka J, Nawrat Z, Cassidy G, Walker R, Morino M, Total Mesorectal Excision Using a Soft and Flexible Robotic Arm: A Feasibility Study in Cadaver Models. Surg Endosc. 2016; 31 (1): 264-273
- Noh Y, Secco EL, Sareh S, Würdemann H, Faragasso A, Back J, Liu H,Sklar E, Althoefer K. A continuum body force sensor designed for flexible surgical robotics devices, 2014, 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, 2014, pp. 3711-3714. doi: 10.1109/EMBC.2014.6944429
- Meenink HCM, Hendrix R, Rosielle PCJN, Steinbuch M, Nijmeijer H, de Smet MC, A master-µslave robot for vitreo-retinal eye surgery, Proceedings of the euspen International Conference – Delft – June 2010, available at: http://www.mate.tue.nl/mate/pdfs/12266.pdf, accessed 23.09.2017
- Ergeneman O, Pokki J, Počepcová V, Hall H, Abbott J J and Nelson B J (2011). Characterization of puncture forces for
- retinal vein cannulation. Journal of Medical Devices, Transactions of the ASME, 5(4), [044504]. DOI: 10.1115/1.4005318
- He X, van Geirt V, Gehlbach P, Taylor R, Iordachita I. IRIS: Integrated Robotic Intraocular Snake. IEEE International Conference on Robotics and Automation: ICRA: [proceedings] IEEE International Conference on Robotics and Automation. 2015;2015:1764-1769. doi:10.1109/ICRA.2015.7139426
- Iordachita I, Sun Z, Balicki M, Kang J, Phee S, Handa J, Gehlbach P, Taylor R. A sub-millimetric, 0.25 mn resolution fully integrated fiber-optic force-sensing tool for retinal microsurgery. International Journal of Computer Assisted Radiology and Surgery (IJCARS). 2009;4(4):383–390
- Uneri A, Balicki MA, Handa J, Gehlbach P, Taylor RH, Iordachita I. New Steady-Hand Eye Robot with Micro-Force Sensing for Vitreoretinal Surg Proc IEEE RAS EMBS Int Conf Biomed Robot Biomechatron. 2010;2010;(26-29):814-819
- Vagvolgyi B, DiMaio S, Deguet A, Kazanzides P, Kumar R, Hasser C, Taylor R. The Surgical Assistant Workstation: a software framework for telesurgical robotics research. MICCAI Workshop on Systems and Architectures for Computer Assisted Interventions. 2008 Sep. Midas Journal: http://hdl.handle.net/10380/1466
- Sun Z, Balicki M, Kang J, Handa J, Taylor R, Iordachita I. Development and preliminary data of novel integrated optical microforce sensing tools for retinal microsurgery. IEEE ICRA. 2009 May:1897-1902
- Yu H, Shen JH, Shah RJ, Simaan N, Joos KM.Evaluation of microsurgical tasks with OCT-guided and/or robot-assisted ophthalmic forceps.Biomed Opt Express. 2015;6(2):457-72 doi: 10.1364/BOE.6.000457.
- Meenink TH, Naus GJ, Beelen MJ, Steinbuch M, Rosielle NP, de Smet MD. Ex-vivo Experiments With A Microrobotic Surgical System For Vitreo-retinal Surgery. Invest. Ophthalmol. Vis. Sci. 2012;53(14):3789
- Vander Poorten EV, Esteveny L, Gijbels A, Rosa B, Schoevaerdts L, Willekens K et al, Use Case for European Robotics in Ophthalmologic Micro-Surgery, available at www.eureyecase.eu/about/publications/papers/vanderpoorten-cras2015.pdf
