Optician CooperVision Myopia Series
Part 1: The concern about myopia prevalence – Professor Desmond Fonn
Part 2: What does a good myopia control study look like? Part 1
– Dr Kathy Dumbleton
Part 3: What does a good myopia control study look like? Part 2
– Dr Kathy Dumbleton
Part 4: Why fitting contact lenses in young children is safe?
– Professor Mark Bullimore
Part 5: Three year milestone results in contact lens myopia control
– Dr Paul Chamberlain
The next two articles in this series will provide clinicians with an overview of current myopia control studies and discuss key aspects of clinical trial design and how they relate to studies intended to investigate the efficacy of methods to control myopia progression, with an emphasis on contact lenses. With this knowledge, Eye Care Practitioners (ECPs) should be better equipped to evaluate the clinical research literature for this important topic. Part 1 will review prevalence and progression, evaluation of clinical research evidence, methods of control and treatment, ethical issues and how progression of myopia can be assessed. Part 2 will discuss the design of clinical studies and how clinical research relating to myopia control is evaluated.
Myopia Prevalence, Progression and Consequences
It has been predicted that the worldwide prevalence of myopia will reach almost 50% by 2050.1 Figure 1 summarises the predicted prevalence of myopia in selected regions by 2050. In the United Kingdom (UK), the proportion of myopic children aged 10 to 16 has more than doubled over the past 50 years and currently nearly one in five teenagers in the UK is now myopic.2 Similar patterns have been reported in Europe.3 Of additional concern are the earlier onset of myopia, and the faster progression that has been reported to occur in pre-teens.2,4-7
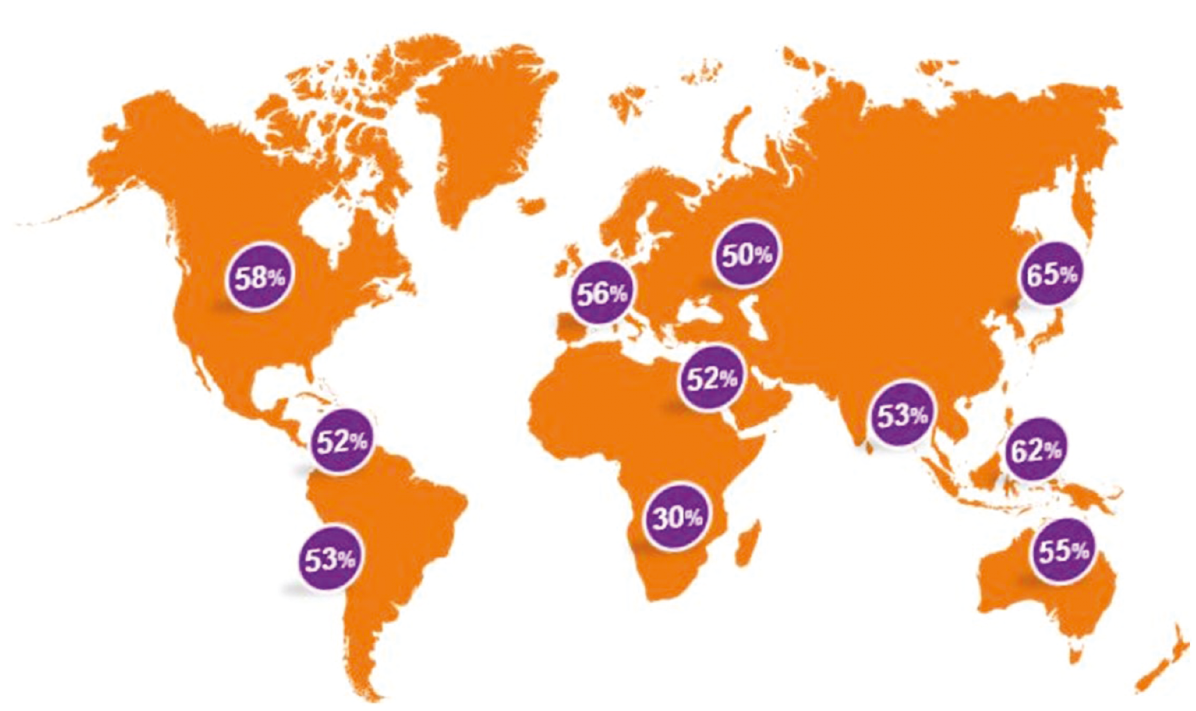
Figure 1: Predicted levels of myopia by 2050. Adapted from Holden et al, Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 20501
Myopia is not simply an inconvenient refractive condition that requires correction, it is a potentially sight threatening disorder that carries an increased risk of developing myopic maculopathy, retinal detachment, cataracts and glaucoma, and these risks rise significantly with increasing levels of myopia.8-10 Table 1 summarises these increased risk levels. Myopia can therefore be considered a serious public health concern.11, 12
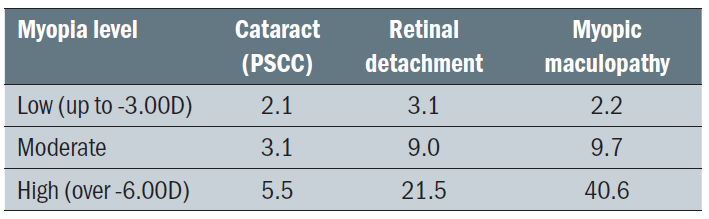 Table 1: Increased risk for development of cataract, retinal detachment and myopic maculopathy according to level of myopia. Adapted from Flitcroft. The complex interactions of retinal, optical and environmental factors in myopia aetiology8
Table 1: Increased risk for development of cataract, retinal detachment and myopic maculopathy according to level of myopia. Adapted from Flitcroft. The complex interactions of retinal, optical and environmental factors in myopia aetiology8
Understanding the Evidence
While the exact mechanisms for the development and progression of myopia are unknown, there do appear to be several genetic, environmental and lifestyle predisposing factors including parental myopia, ethnicity, greater reading and near activity and level of physical and outdoor activity (figure 2).8,13-21 Many ECPs are now discussing these factors and options to control progression with their patients and the parents of their patients.22 ECPs need to use the best evidence available to them when making decisions about the care of their patients and in this respect, prescribing treatments for myopia control is no different from the management of ocular disease. The term ‘evidence-based medicine’ was first coined by Guyatt in 1991 23 and further described by the Evidence-Based Medicine Working Group in 1992. 24 This paradigm shift requires ECPs to integrate their evaluation of current research evidence with their clinical experience, when determining the most appropriate treatment options for their patients.
 Figure 2: Low levels of time spent outdoors coupled with increased near activity may influence myopia development and progression
Figure 2: Low levels of time spent outdoors coupled with increased near activity may influence myopia development and progression
Myopia Correction, Control and Treatment
It is important to make the distinction between myopia correction, which is generally achieved with prescription spectacles or contact lenses, and myopia control or treatment in which the development of myopia is either prevented, or its progression limited (figure 3).
 Figure 3: Correcting myopia with single vision spectacles does nothing to slow the rate of myopia progression
Figure 3: Correcting myopia with single vision spectacles does nothing to slow the rate of myopia progression
Pharmacological treatments for myopia control with atropine and pirenzepine, while effective, have in general been unpopular as a result of their associated side effects and limited availability of ophthalmic preparations in the lower concentrations required for this indication.25, 26
The peripheral refractive state of the eye has been shown to be important in modulating eye growth with the stimulus for eye growth being a defocused peripheral retinal image with hyperopic blur.27 As a consequence lenses designed to minimise hyperopic defocus, or cause myopic defocus, have been investigated and myopia control with contact lenses has become popular and been shown to be effective, both with orthokeratology and peripheral defocus modifying soft contact lenses.28-30 The advantage of myopia control with contact lenses is that myopia progression can be controlled while the patient’s current refractive error is also being corrected. Progressive myopes have been shown to exhibit relative peripheral hyperopic defocus.27,31,32 Since both orthokeratology and soft contact lenses designed to control myopia induce relative peripheral myopia, these lens designs have the potential to slow or stop eye growth, and as a result control the progression of myopia.27,33,34 Indeed in a recent survey ECPs were reported to believe that myopia-controlling contact lenses are the most effective method of reducing progression.22
In some countries orthokeratology is extremely popular with 86% of all rigid lens fits reported to be for orthokeratology in Hong Kong and the majority of these being to patients under the age of 18, most likely for myopia control;35 however, the popularity of orthokeratology varies significantly by country. This may be due to the lack of availability of corneal topographers in some practices, greater expense and the increased risks associated with overnight wear.36,37
In recent years a number of simultaneous image multifocal soft contact lens designs have been proposed for use in children to control myopia progression. These lenses provide correction of the distance refractive error at the fovea but have an additional correction within the optical zone that is relatively more positive in power (generally by 1.50 to 2.50D) as compared with the distance prescription. The distance correction is in the centre of the optical zone and either gradually changes to the more positive power (or near addition) when moving away from the optical centre (centre distance design),38 or the central correction zone is surrounded by a series of concentric zones of alternating distant and near addition powers (dual focus design).39-41 An alternative design manipulates higher-order aberrations to provide extended depth of focus with variation of the mean power across the optic zone and therefore optimising retinal image quality across a wide range of distances.42,43 Additionally, positive spherical aberration can be incorporated into the optical design to shift the peripheral retinal hyperopic blur that occurs during accommodation in the myopic direction,44 and soft radial refractive gradient (SRRG) contact lenses have been designed to correct the central refraction and simultaneously produce constant peripheral myopic defocus that increased gradually towards the periphery of the optical zone.45
Children and Contact Lens Clinical Trials
Since the typical target group of interest in myopia control clinical research trials is young children, it must be remembered that this is considered a vulnerable population and therefore the trials must be designed to avoid placing the participating children at undue risk. As per the Declaration of Helsinki,46 ‘Medical research with a vulnerable group is only justified if the research is responsive to the health needs or priorities of this group and the research cannot be carried out in a non-vulnerable group. In addition, this group should stand to benefit from the knowledge, practices or interventions that result from the research.’ All clinical trials on the control of myopia progression in children must meet these requirements.
Recent studies have reported that children can manage contact lens wear independently from the age of the age of eight;47,48 however, up until recently ECPs have been reluctant to fit young children with contact lenses.49 This is most likely due to safety concerns. Fortunately, current evidence supports soft contact lens wear in children as being safe and the incidence of corneal infiltrative events in children has been reported to be no higher than in adults and may be considerably lower in children aged eight to 11.50 Figure 4 shows the incidence of corneal infiltrative events in a series of prospective and retrospective studies conducted on children and adults. In four of the prospective studies involving children no infiltrative events were reported,44,51-53 and in those studies where infiltrative events were reported to occur, the rates were lower for the younger children,54-56 than for adults.54,57,58
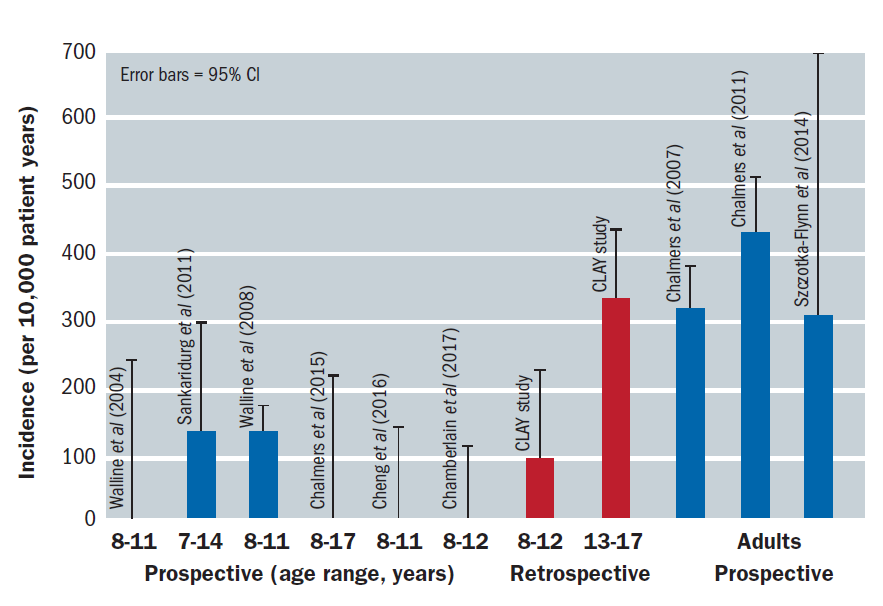 Figure 4: The incidence of corneal infiltrative events in a series of prospective and retrospective studies involving children and adults54-56
Figure 4: The incidence of corneal infiltrative events in a series of prospective and retrospective studies involving children and adults54-56
In a recent survey, ECPs worldwide considered children aged 8.8 years to be old enough for myopia control contact lenses, and in Europe, a minimum age 7.3 years was considered to be adequate for myopia control soft contact lenses;22 however, in clinical practice, and clinical trials evaluating contact lens wear for the treatment of myopia progression, both parents and children should be trained in insertion and removal of the lenses, contact lens care and in identifying signs and symptoms that could be indicative of potential contact lens-related problems.
Risks, Burdens and Benefits of Participating in Clinical Trials
The Declaration of Helsinki also recognises that in medical research most interventions or treatments involve risks and burdens and further states that ‘Medical research involving human subjects may only be conducted if the importance of the objective outweighs the risks and burdens to the research subjects’.46 The possible risks and burdens must be assessed before the trial commences and measures to minimise these should be implemented and addressed in publications reporting the results. For example, clear instructions should be provided with respect to swimming and other exposure to water while wearing contact lenses.
Unfortunately few studies evaluating the efficacy of myopia control conducted to date have reported on safety data, and as a result the incidence of adverse events in this population is not known; however, this would be expected to be extremely low, particularly for daily disposable soft contact lenses.51,59,60 Clinical trials should ensure that all adverse events are carefully documented and reported, ideally using a standardised set of diagnoses,54,61 as recommended by Bullimore.50
A further benefit is that contact lens wear has been reported to offer social, sporting and visual benefits and to improve self-esteem in children, when compared with spectacle wear (figure 5).62-64 In addition, myopic children younger than 12 years of age have reported better vision-related quality of life when they are fit with contact lenses than when they wear glasses.65 This was confirmed in a study that was recently conducted in Spain in which vision-related quality-of-life measures were evaluated in children wearing distance single-vision spectacles versus MiSight (CooperVision Inc) contact lenses, a specific concentric design for myopia control.66 The Paediatric Refractive Error Profile (PREP) questionnaire was administered and the ratings for appearance, satisfaction, effect on activities, handling, and peer perceptions were significantly better in the MiSight group at 12 and 24 months than those given by children in the spectacle group, as was the overall score. Only the subjectively rated near vision was superior in the spectacle group, indicating that peripheral defocus modifying soft contact lenses may result in compromise in visual performance under some viewing and lighting conditions and therefore it is important that objective and/or subjective assessments of vision are made during studies evaluating lenses designed for myopia control.
 Figure 5: Children wearing contact lenses report greater ability to participate in sport compared to wearing spectacles
Figure 5: Children wearing contact lenses report greater ability to participate in sport compared to wearing spectacles
Measurement of Myopia Progression in Clinical Trials
The two key measurements that are used to monitor myopia progression in clinical trials are axial length and refractive error. Axial length can be measured with optical and ultrasonic biometry. In studies investigating the progression of myopia in children, optical non-contact biometry is the preferred technique and two instruments are principally used in the collection of data. These are the IOL Master (Carl Zeiss Meditec Inc, Jena, Germany) and the Lenstar LS 900 (Haag-Streit USA, Mason, OH). In clinical trials refractive error should be measured using an autorefractor following cycloplegia. In a recent Food and Drug Administration workshop on controlling the progression of myopia with contact lenses that was conducted in the United States, it was recommended that tropicamide 1% be used in clinical trials since it has shorter effects on cycloplegia and pupil dilation which is important for retention of children where there are multiple study visits.67
Interpreting the Research
The past decade has seen enormous interest in the field of myopia control with a high number of presentations at clinical conferences and publications in journals and trade magazines. Consequently, there is a growing library of research evidence accessible to ECPs. In order for the results to be correctly interpreted, it is important for ECPs to understand exactly how each study has been conducted, with a particular focus on the study duration, number and characteristics of participants enrolled and the control that is used for comparison.
In part 2 we look at clinical study design in more detail to provide a complete understanding of the key elements of a myopia control clinical trial in order to allow ECPs to be better equipped to be able to determine the most appropriate methods of management for the young patients in their practices.
Dr Kathy Dumbleton is a clinical research scientist and consultant based in Berkeley, California where she is also a clinical Associate Professor at the School of Optometry, University of California, Berkeley.
This article was written with support from CooperVision
References
- Holden BAF, TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123:1036-42.
- McCullough SJOD, L, Saunders KJ. Six Year Refractive Change among White Children and Young Adults: Evidence for Significant Increase in Myopia among White UK Children. PLoS One. 2016;11:e0146332.
- Williams KMV, VJ, Cumberland P, Bertelsen G, Wolfram C, Buitendijk GH, Hofman A, van Duijn CM, Vingerling JR, Kuijpers RW, Hohn R, Mirshahi A, Khawaja AP, Luben RN, Erke MG, von Hanno T, Mahroo O, Hogg R, Gieger C, Cougnard-Gregoire A, Anastasopoulos E, Bron A, Dartigues JF, Korobelnik JF, Creuzot-Garcher C, Topouzis F, Delcourt C, Rahi J, Meitinger T, Fletcher A, Foster PJ, Pfeiffer N, Klaver CC, Hammond CJ. Prevalence of refractive error in Europe: the European Eye Epidemiology (E(3)) Consortium. Eur J Epidemiol. 2015;30:305-15.
- Czepita DZ, M, Mojsa A. Prevalence of myopia and hyperopia in a population of Polish schoolchildren. Ophthalmic Physiol Opt. 2007;27:60-5.
- Donovan LS, P, Ho A, Naduvilath T, Smith EL, 3rd, Holden BA. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012;89:27-32.
- Group C. Myopia stabilisation and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54:7871-84.
- Vitale SS, RD, Ferris FL, 3rd. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127:1632-9.
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31:622-60.
- Saw SMG, G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25:381-91.
- Silva R. Myopic maculopathy: a review. Ophthalmologica. 2012;228:197-213.
- Holden BAW, DA, Jong M, Sankaridurg P, Fricke TR, Smith EL III, Resnikoff S. Myopia: a growing global problem with sight-threatening complications. Community Eye Health. 2015;28:35.
- Holden BS, P, Smith E, Aller T, Jong M, He M. Myopia, an underrated global challenge to vision: where the current data takes us on myopia control. Eye. 2014;28:142-6.
- Guggenheim JAN, K, McMahon G, Ness AR, Deere K, Mattocks C, Pourcain BS, Williams C. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest Ophthalmol Vis Sci. 2012;53:2856-65.
- Jones LAS, L T, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524-32.
- Lin ZV, B, Jhanji V, Mao GY, Gao TY, Wang FH, Rong SS, Ciuffreda KJ, Liang YB. Near work, outdoor activity, and their association with refractive error. Optom Vis Sci. 2014;91:376-82.
- Morgan IGO-M, K, Saw SM. Myopia. Lancet. 2012;379:1739-48.
- Mutti DOM, GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633-40.
- O’Donoghue LK, VV, McClelland JF, Logan NS, Owen CG, Saunders KJ, Rudnicka AR. Risk Factors for Childhood Myopia: Findings From the NICER Study. Invest Ophthalmol Vis Sci. 2015;56:1524-30.
- Pan CWR, D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32:3-16.
- Wojciechowski R. Nature and nurture: the complex genetics of myopia and refractive error. Clin Genet. 2011;79:301-20.
- Wu PCT, CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120:1080-5.
- Wolffsohn JSC, A, Cho P, Gifford K, Jones L, Li M, Lipener C, Logan NS, Malet F, Matos S, Meijome JM, Nichols JJ, Orr JB, Santodomingo-Rubido J, Schaefer T, Thite N, van der Worp E, Zvirgzdina M. Global trends in myopia management attitudes and strategies in clinical practice. Cont Lens Anterior Eye. 2016;39:106-16.
- Guyatt G. Evidence-based medicine. ACP J Club. 1991;114:A16.
- Evidence-Based Medicine Working G. Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268:2420-5.
- Chia AC, WH, Cheung YB, Wong WL, Lingham A, Fong A, Tan D. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012;119:347-54.
- Cooper JE, N, Schulman E, Wang FM. Maximum atropine dose without clinical signs or symptoms. Optom Vis Sci. 2013;90:1467-72.
- Smith EL, 3rd. Prentice Award Lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011;88:1029-44.
- Gonzalez-Meijome JMP-d-M, SC, Faria-Ribeiro M, Lopes-Ferreira DP, Jorge J, Legerton J, Queiros A. Strategies to Regulate Myopia Progression With Contact Lenses: A Review. Eye Contact Lens. 2016;42:24-34.
- Turnbull PRM, OJ, Phillips JR. Contact Lens Methods for Clinical Myopia Control. Optom Vis Sci. 2016;93:1120-6.
- Walline JJ. Myopia Control: A Review. Eye Contact Lens. 2016;42:3-8.
- Lin ZM, A, Chen X, Li L, Sankaridurg P, Holden BA, Ge J. Peripheral defocus with single-vision spectacle lenses in myopic children. Optom Vis Sci. 2010;87:4-9.
- Shen JC, CA, Soni PS, Thibos LN. Peripheral refraction with and without contact lens correction. Optom Vis Sci. 2010;87:642-55.
- Charman WNM, J, Atchison DA, Markwell EL. Peripheral refraction in orthokeratology patients. Optom Vis Sci. 2006;83:641-8.
- Troilo D. The case for lens treatments in the control of myopia progression. Optom Vis Sci. 2016;93:1045-8.
- Morgan PBW, Craig A; Tranoudis, Ioannis G; Helland, Magne; Efron, Nathan; Jones, Lyndon WJ; van Beusekom, Marco; Grupcheva, Christina N; Jones, Deborah; Beeler-Kaupke, Marion; Qi, Polo; Tan, Kah-Ooi; Krasnanska, Jitka; Pult, Heiko; Ravn, Ole; Santodomingo-Rubido, Jacinto; Végh, Mihály; Fan, Chi Shing; Erdinest, Nir; Jafari, Ali Reza; Montani, Giancarlo; Itoi, Motozumi; Chu, Byoung Sun; Bendorien, Jolanta; Ziziuchin, Veronica; van Der Worp, Eef; Lam, Wanda; Romualdez-Oo, Jeanette; Abesamis-Dichoso, Carmen; González-Méijome, José Manuel; Belousov, Vadim; Gierow, Peter; Stabuc Silih, Mirna; Hsiao, John; Nichols, Jason J. International Contact Lens Prescribing in 2016. Contact Lens Spectrum. 2017;32:30-5.
- Bullimore MAS, L. T.; Jones-Jordan, L. A. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci. 2013;90:937-44.
- Watt KGS, H. A. Trends in microbial keratitis associated with orthokeratology. Eye Contact Lens. 2007;33:373-7; discussion 82.
- Walline JJG, KL, McVey ME, Jones-Jordan LA. Multifocal contact lens myopia control. Optom Vis Sci. 2013;90:1207-14.
- Anstice NSP, JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118:1152-61.
- Lam CST, WC, Tse DY, Tang YY, To CH. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a two-year randomised clinical trial. Br J Ophthalmol. 2014;98:40-5.
- Aller TAL, M, Wildsoet CF. Myopia Control with Bifocal Contact Lenses: A Randomized Clinical Trial. Optom Vis Sci. 2016;93:344-52.
- Tilia D, Bakaraju RC, Chung J, Sha J, Delaney S, Munro A, et al. Short-Term Visual Performance of Novel Extended Depth-of-Focus Contact Lenses. Optom Vis Sci. 2016;93:435-44.
- Bakaraju RC, Xu P, Chen X, Ma M, Song S, Jong M, et al. Extended depth-of-focus contact lenses can slow the rate of progression of myopia. 2015;56.
- Cheng XX, J, Chehab K, Exford J, Brennan N. Soft Contact Lenses with Positive Spherical Aberration for Myopia Control. Optom Vis Sci. 2016;93:353-66.
- Paune JM, H, Armengol J, Quevedo L, Faria-Ribeiro M, Gonzalez-Meijome JM. Myopia Control with a Novel Peripheral Gradient Soft Lens and Orthokeratology: A Two-Year Clinical Trial. Biomed Res Int. 2015;2015:507572.
- Association WM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191-4.
- Walline JJL, S, Zadnik K. Daily disposable contact lens wear in myopic children. Optom Vis Sci. 2004;81:255-9.
- Walline JJL, K. O.; Nichols, J. J. Long-term contact lens wear of children and teens. Eye Contact Lens. 2013;39:283-9.
- Efron NM, PB, Woods CA. International Contact Lens Prescribing Survey, Consortium. Survey of contact lens prescribing to infants, children, and teenagers. Optom Vis Sci. 2011;88:461-8.
- Bullimore MA. The Safety of Soft Contact Lenses in Children. Optom Vis Sci. 2017;94:638-46.
- Chalmers RLH-C, SB, Keay L, Gleason WJ, Albright R. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci. 2015;56:654-63.
- Chamberlain P, Back A, Lazon De La Jara P. 3-year Effectiveness of a Dual-Focus 1 day Soft Contact Lens for Myopia Control. British Contact Lens Association Clinical Conference. Liverpool2017.
- Walline JJ, Jones LA, Mutti DO, Zadnik K. A randomised trial of the effects of rigid contact lenses on myopia progression. Arch Ophthalmol. 2004;122:1760-6.
- Chalmers RLW, H, Mitchell GL, Lam DY, Kinoshita BT, Jansen ME, Richdale K, Sorbara L, McMahon TT. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci. 2011;52:6690-6.
- Sankaridurg PH, B, Smith E 3rd, Naduvilath T, Chen X, de la Jara PL, Martinez A, Kwan J, Ho A, Frick K, Ge J. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52:9362-7.
- Walline JJJ, LA, Sinnott L, Manny RE, Gaume A, Rah MJ, Chitkara M, Lyons S. Achieve Study Group. A randomized trial of the effect of soft contact lenses on myopia progression in children. Invest Ophthalmol Vis Sci. 2008;49:4702-6.
- Szczotka-Flynn LJ, Y, Raghupathy S, Bielefeld RA, Garvey MT, Jacobs MR, Kern J, Debanne SM. Corneal inflammatory events with daily silicone hydrogel lens wear. Optom Vis Sci. 2014;91:3-12.
- Chalmers RL, McNally JJ, Schein OD, Katz J, Tielsch JM, Alfonso E, et al. Risk factors for corneal infiltrates with continuous wear of contact lenses. Optom Vis Sci. 2007;84:573-9.
- Chalmers RLK, L, McNally J, Kern J. Multicenter case-control study of the role of lens materials and care products on the development of corneal infiltrates. Optom Vis Sci. 2012;89:316-25.
- Stapleton FC, N. Contact lens-related microbial keratitis: How have epidemiology and genetics helped us with pathogenesis and prophylaxis. Eye. 2012;26:185-93.
- Sankaridurg PC, X, Naduvilath T, Lazon de la Jara P, Lin Z, Li L, Smith EL 3rd, Ge J, Holden BA. Adverse events during two years of daily wear of silicone hydrogels in children. Optom Vis Sci. 2013;90:961-9.
- Dias LM, RE, Weissberg E, Fern KD. Myopia, contact lens use and self-esteem. Ophthalmic Physiol Opt. 2013;33:573-80.
- Walline JJG, A, Jones LA, Rah MJ, Manny RE, Berntsen DA, Chitkara M, Kim A, Quinn N. Benefits of contact lens wear for children and teens. Eye Contact Lens. 2007;33:317-21.
- Walline JJJ, LA, Sinnott L, Chitkara M, Coffey B, Jackson JM, Manny RE, Rah MJ, Prinstein MJ. Achieve Study Group. Randomised trial of the effect of contact lens wear on self-perception in children. Optom Vis Sci. 2009;86:222-32.
- Rah MJW, JJ, Jones-Jordan LA, Sinnott LT, Jackson JM, Manny RE, Coffey B, Lyons S. Achieve Study Group. Vision specific quality of life of pediatric contact lens wearers. Optom Vis Sci. 2010;87:560-6.
- Pomeda AR, Perez-Sanchez B, Canadas Suarez MDP, Prieto Garrido FL, Gutierrez-Ortega R, Villa-Collar C. MiSight Assessment Study Spain: A Comparison of Vision-Related Quality-of-Life Measures Between MiSight Contact Lenses and Single-Vision Spectacles. Eye Contact Lens. 2017.
- FDA. Public Workshop - Controlling the Progression of Myopia: Contact Lenses and Future Medical Devices. FDA White Oak Campus, Silver Spring, MD2016.
