Both accommodation and convergence alter when changing from spectacles to contact lenses. When wearing spectacles, the eyes look at the image of the object focused by the spectacle lenses, whereas with contact lenses, they are, to all intents and purposes, looking at the object directly.
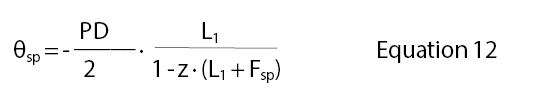
For ease of continuity, the following three equations were outlined in Part 1: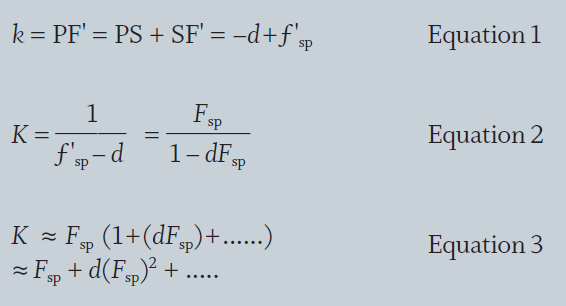
Accommodation
Figure 1 in the first part of that series, shows a myopic eye viewing a near object B positioned l1 from the spectacle lens S of power Fsp.*
(*The symbol F'sp was used in the first part of this article. Since the lenses are assumed to be thin, there is no need to distinguish between front vertex and back vertex focal powers, and Fsp is used in this second part.)
The image, B', is formed l'1 from the lens. Regarding the spectacle lens as being thin:
L'1 = L1 +Fsp
where L1 = 1/l1 (m) = 1000/l1 (mm)
Hence
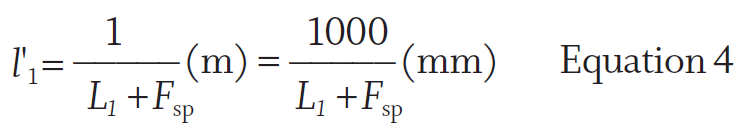
Measured from the cornea, the image B' is distant:
Taking the same eye as in Part 1 (Optician 03.11.17), consider an eye with spectacle correction of -7.00 DS at a vertex distance of 13mm viewing an object at -40cm from the spectacle lens.
Therefore:
L1 = -2.50 D
L'1 = L1 + Fsp = -2.50 -7.00 = -9.50 D
l'1 = 1000/-9.50 = -105.26(mm)
-d = -13(mm)
l2 = -118.26(mm)
Therefore L2 = 1000/ (-118.26) = -8.46 D
But the ocular refraction, K = -6.42 D
Therefore the accommodation required
= K - L2 = -6.42 - (-8.46) = 2.04 D
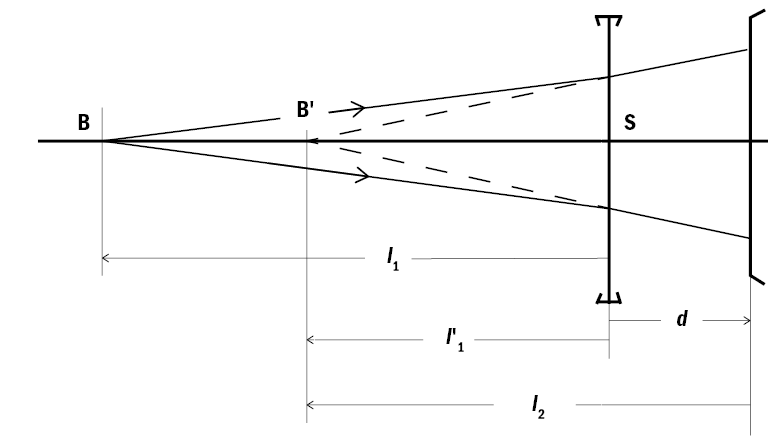
Figure 1: Near vision, accommodation and the myopic eye
For the contact lens wearing eye, the object distance is simply OB, or -d + l1 , and in this example, is -13 -250 = -263mm. Therefore the accommodation required is -1000/(-263) = 3.80 D. This is considerably more than that required by the spectacle corrected wearer. Hence, a myopic wearer changing from spectacles to contact lenses will have to accommodate more. This could cause symptoms for a nearly presbyopic patient. Conversely, a hypermetrope will need to accommodate less when wearing contact lenses.
Treating this theoretically, combining equations 4 and 5 gives, for the spectacle wearer:
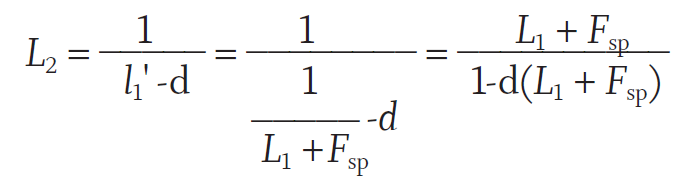
From Equation 3 in part 1 (see box),
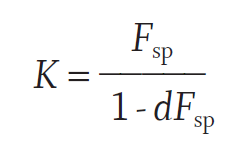
Hence the required ocular accommodation, A0,sp = K - L2
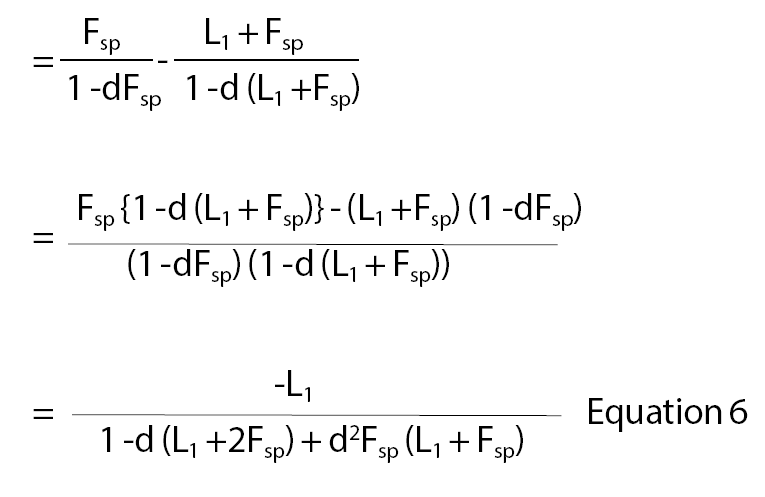
If terms in d2 are ignored, this approximates to:
Ao,sp = -L1 {1 + d (L1 + 2Fsp)} Equation 7
For the contact lens wearing eye, the demand on
accommodation
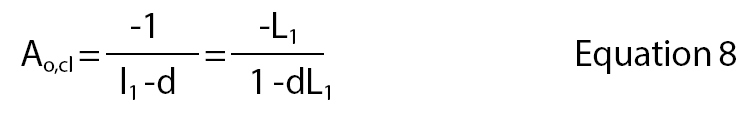
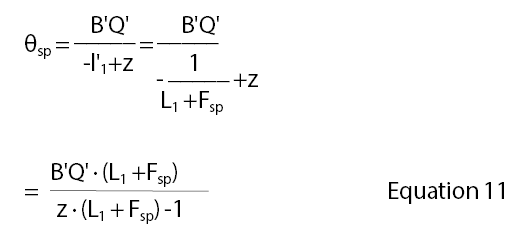
Hence the ratio of the accommodation required for the contact lens wearing eye compared with the spectacle lens wearing eye is (Equation 8 ÷ Equation 6) is,
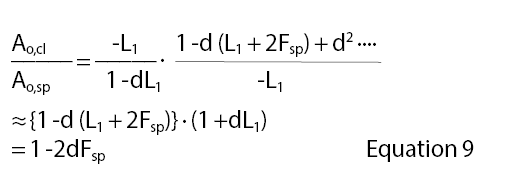
Figure 2 shows the ocular accommodation required for a spectacle lens wearer (from equation 6) for powers from -12.00 to +12.00 D for an object 250mm from the spectacle lens positioned at a vertex distance of 15mm, the amount of accommodation for a contact lens wearer, and the ratio from the calculations. The ratio is positive for myopic eyes, confirming that the myopic wearer has to accommodate more through contact lenses than with spectacles.

Figure 2: The ocular accommodation required with spectacles and contact lenses, and the ratio of accommodation required when wearing spectacles compared with contact lenses
Convergence
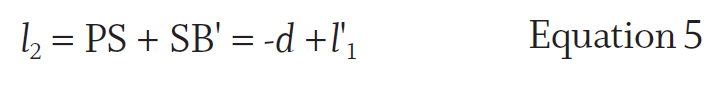
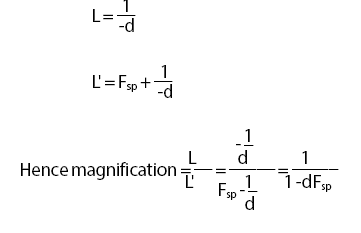
In the upper part of figure 3, for the spectacle lens wearer, the midpoint Q between the eyes in the object plane should be considered as the tip of the object BQ, imaged by the spectacle lens as B'Q'. BQ has “height” (PD/2), so the height of the image:
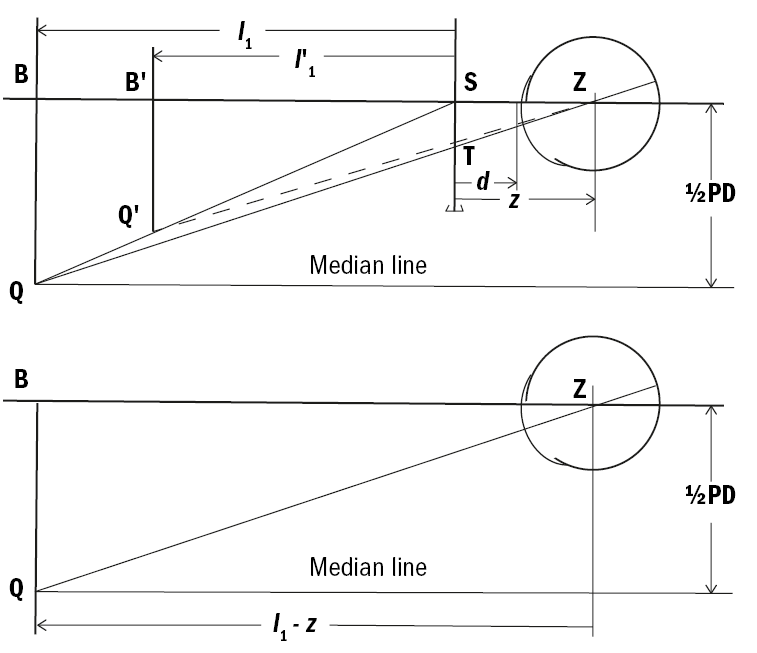
Figure 3: Convergence with spectacles and contact lenses
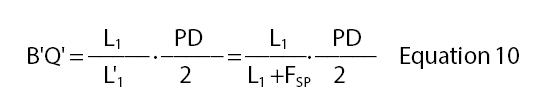
The eye rotates about the centre of rotation, Z, to view the tip of this image. Thus the ocular rotation or the part of the convergence by one eye, θsp, is given by:
where z is the distance from the spectacle lens to the centre of rotation. Multiplying equations 10 and 11 together gives:
If calculated in prism dioptres, this should be multiplied by 100 if all measurements are in mm or m.
When wearing contact lenses, since the lens stays centred on the cornea as the eye rotates, the eyes rotate to look directly at the object B. Hence the rotation, θcl, in radians, is:
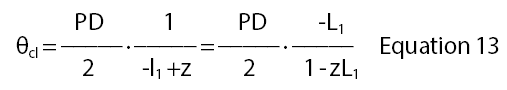
Hence the ratio of ocular rotation with contact lenses compared with that when wearing spectacle lenses is given by equation 13 divided by equation 12:
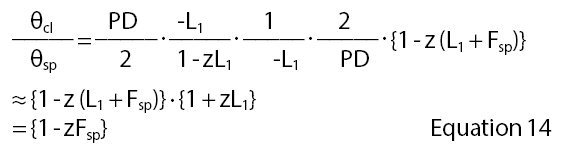
The myopic patient, on first wearing contact lenses has to converge more for near vision than with spectacles, as shown in figure 4, since the ray path from the object no longer passes through the base in prism in the periphery of the lens. Thus a prospective wearer who has poor convergence may report symptoms for near vision. Similarly, an esophoric patient may be troubled by the increased demand on accommodation because of the increased accommodative convergence.
Figure 4: Comparison between convergence with spectacles and contact lenses showing the convergence (in prism dioptres for each eye) for an object at 400mm from the spectacle lens, ocular rotation distance 27mm, PD 64mm and the ratio of convergence needed when wearing spectacle lenses compared with contact lenses
Comparing equation 7 for the ratio of accommodation and equation 12 for convergence,
The distance z (which is often taken as 25 to 30mm) is approximately double1 the typical vertex distance d of 12 to 16mm. The numerator and denominator of equation 15 are therefore very similar, so that the accommodation: convergence ratio is the same whether wearing spectacles or contact lenses. Hence, although the myopic wearer has to accommodate and converge more for near vision when wearing contact lenses instead of spectacles, the two functions are altered similarly, so provided there is plenty of accommodation and convergence in reserve, this should not be too troubling. Conversely, the hypermetropic wearer accommodates and converges less in contact lenses than spectacles, though these effects are small in the range from +4.00 D down to -4.00 D.
Spectacle Magnification
Because a spectacle lens is positioned well in front of the entrance pupil of the eye, it can cause significant magnification of the retinal image. Although this is termed spectacle magnification (SM), it applies also to contact lenses, and describes the size of the retinal image when wearing a lens to the basic size without the lens. The extra dimension resulting from the blur disc in the uncorrected eye is ignored, hence the name ‘basic’ size.
Figure 5 illustrates a spectacle-corrected myopic eye viewing a distant object subtending angle θ at the optical centre of the lens. The image height, h', equals ƒ'sp•θ if θ is small – the diagram is exaggerated and not to scale.
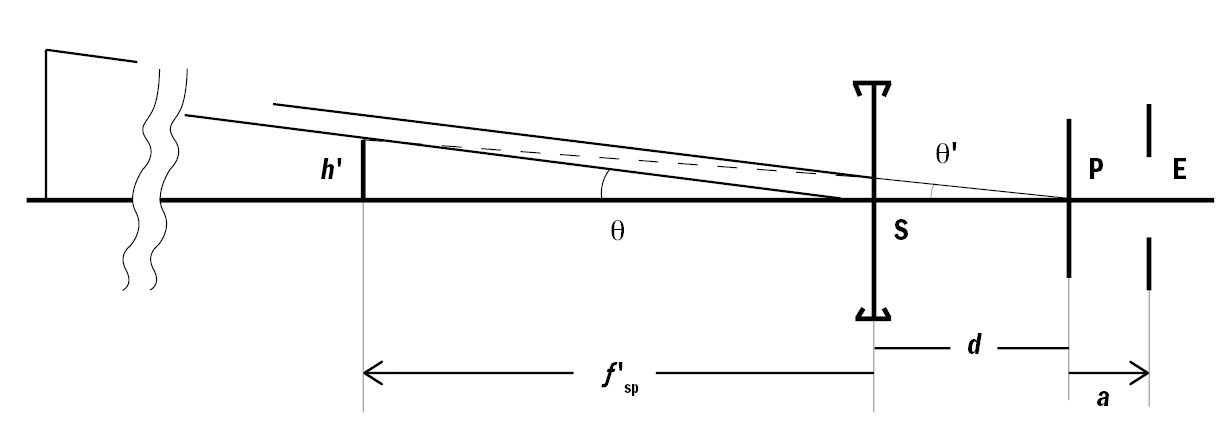
Figure 5: Diagram to illustrate the derivation of the power factor in spectacle magnification
When viewed by the eye, the angular subtense of the image,
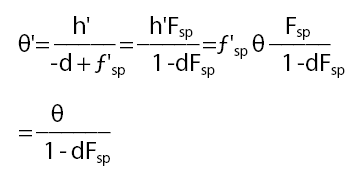
Therefore:
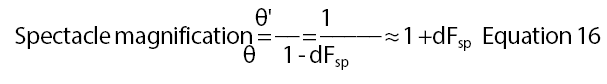
if terms in d2 and higher, when d is expressed in metres, are ignored as being insignificant.
As a rough and ready rule, this is about 1½ % per dioptre of lens power, an increase in size for positive-powered lenses, a decrease for negative-powered lenses. When wearing contact lenses, because the object is distant, the angular subtense remains θ at the cornea so there is no spectacle magnification.
The distance 'd' in figure 5 was shown as being between the lens and the corneal vertex, but strictly it should be measured to the eye's entrance pupil, E, distance a behind the corneal vertex. Hence, using the approximate formula, the spectacle magnification is:
Spectacle magnification ≈ 1 + (d +a) Fsp
When wearing contact lenses, the spectacle magnification ≈1+aFsp and ignoring the effectivity difference in between the spectacle and contact lens powers, named simply F for this expression, the ratio between the spectacle magnifications is
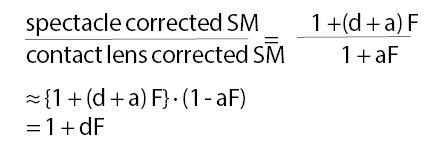
which is the same as equation 16 as above and therefore justifies ignoring the entrance pupil distance in the earlier analysis by measuring just to the cornea.
Strictly, the spectacle magnification is the product of the power factor given in the equations above and the shape factor which is the extra magnification caused by the curvature of the lens and its thickness:
where t is the centre thickness of the lens, n its refractive index and F1 the power of the front surface (see textbooks on spectacle lenses or visual optics for details), and therefore the complete spectacle magnification = power factor x shape factor
Because of their shallow front surface curvatures and low centre thickness, the power factor can be ignored for minus powered spectacle lenses, but it increases the overall spectacle magnification for plus powered lenses. The modern use of higher refractive index materials and flatter aspherical front surfaces that also result in thinner lenses reduces the power factor compared with the spherical surfaced standard index (1.5 or 1.523) lenses used years ago.
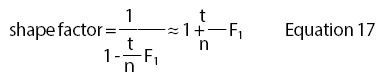
Figure 6 illustrates the effect of spectacle magnification on the retinal image size when changing from a thin spectacle lens (ie ignoring its shape factor) to that of real RGP or soft lenses, including their shape factor. The magnification will be little different for minus powered spectacle lenses if their shape factor is taken into consideration, but will be increased for plus powered lenses.
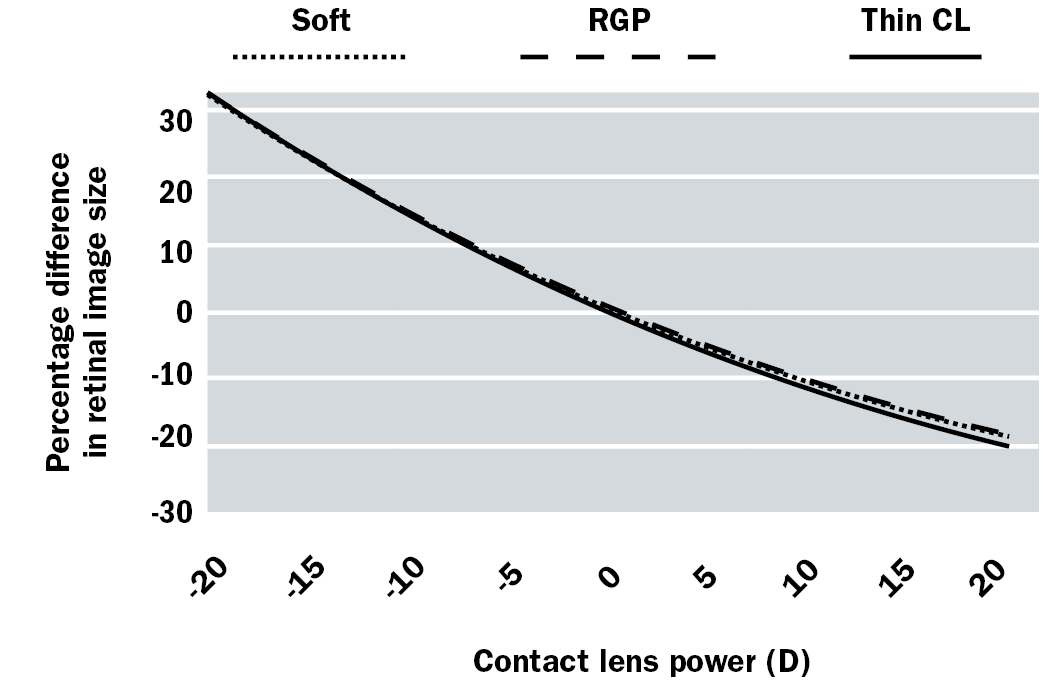
Figure 6: Percentage difference in size of retinal images relative to a thin spectacle lens
The result here is that the retinal image in the contact lens corrected myopic eye is larger than that of the spectacle lens corrected eye, and smaller for the hypermetropic eye. A -10.00 D myopic eye will, using the approximate equation 16, see an image about 15% larger when changing from spectacles to contact lenses, possibly resulting in a slightly better VA. Remember that on a logMAR chart, the difference in size from one line to the next is = 1.2589 or a 26% difference, a bigger change than that resulting from changing from spectacles to contact lenses. The larger image could also result in a misjudgement of distances until adaptation has occurred.
This discussion is based on distance vision; for near vision, an additional factor, the proximity factor, also needs to be taken into account, though this is negligible except for high powered lenses.2
Anisometropia
Eye movements and anisometropia
The previous discussion has considered the effects of spectacle lenses on the angular subtense of the image presented to the eye. The different lens powers present in anisometropia will give rise to different sized images, which in turn will require different sized eye movements to look from one point to another on the object. This causes differential prismatic effects as the eyes move from side to side or up and down. The latter direction is more important because the vertical fusional reserves are lower that the horizontal.
Consider an anisometropic spectacle lens wearer looking at an object 250mm away from the spectacle lens and positioned 100mm below the optical axes of the lenses. Suppose the prescription is R -1.00 DS, the left +3.00 DS. The diagram in figure 3 can be used again, but now this represents a vertical instead of a horizontal plane. A rough, but overestimate, of the induced vertical prism can be deduced by similar triangles and Prentice’s rule.
BQ, now in the vertical plane, is 100mm, and the distance BZ is 275mm if z is taken as 25mm. The intercept height, ST, on the spectacle lens is roughly (25/275)x100 = 9.1mm. By Prentice’s rule, (prism = decentration × lens power, or P = cF), there is 0.9 prism dioptres base down for the right eye and 2.7 prism dioptres base up for the left eye, or 3.6 prism dioptres base up left eye induced vertical prism imbalance.
An accurate calculation, using the images formed by the spectacle lenses, is as seen on table 1.
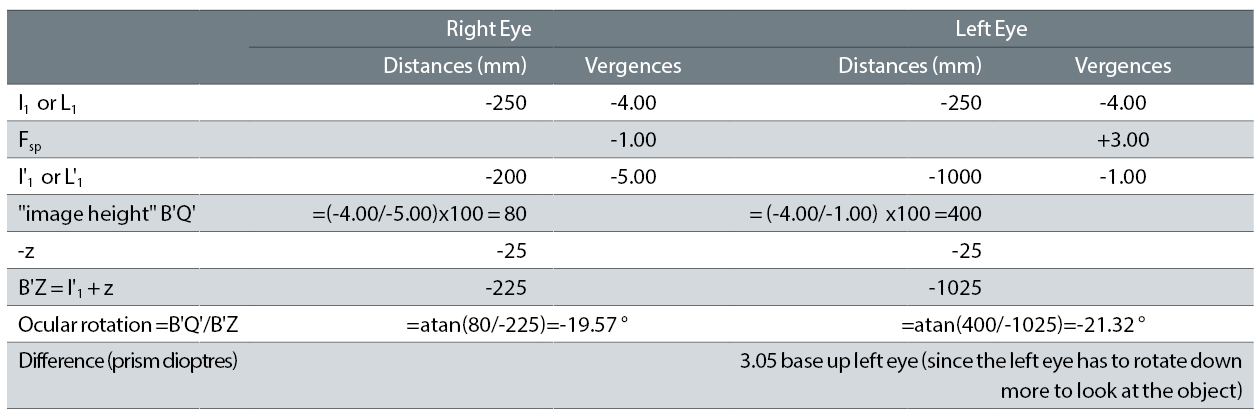
Table 1
When wearing contact lenses, the lenses move with the eyes, so that differential eye movements are no longer required, a great benefit.
Image sizes and anisometropia
The myopic eye is frequently found to have a longer axial length than the emmetropic eye.3,4 Hence a difference in myopia between the right and left eyes may well be caused by a difference in axial length. In the author’s experience, the K-readings of the two eyes of a patient with anisometropia were usually similar.
The upper part of figure 7 illustrates two superimposed uncorrected myopic eyes viewing a distant object, assumed to have the same refractive power. The basic image heights, h'1 and h'2, are formed by the ray through the centre of the pupil, which is considered to be in the plane of the refracting surface of the single surface reduced eye in the diagram. These will be roughly proportional in height to the axial lengths. Because contact lenses are positioned close to the entrance pupil and first principal point of the eye, they will have little effect on the image heights, so these will still be different in the corrected eye with axial ametropia.
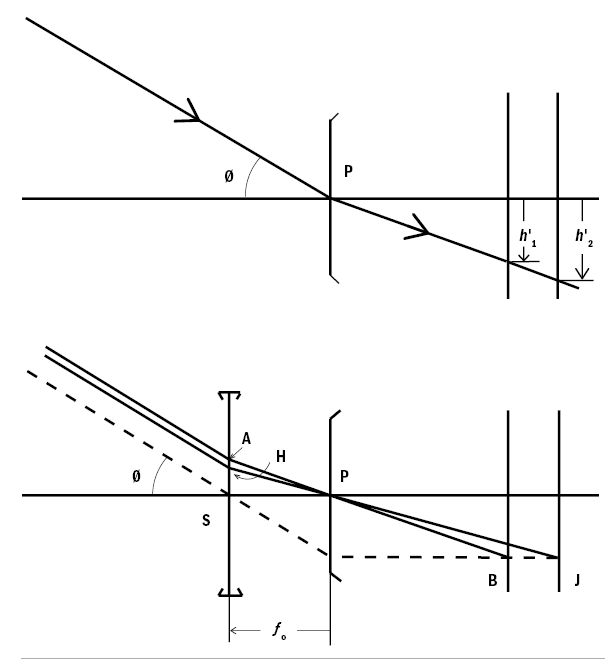
Figure 7: Image size and axial length. Upper diagram: the image size is proportional to axial length in the simple reduced eye. Lower diagram: constant image size with changes in axial length when corrected with a spectacle lens
The lower part of figure 7 shows the same eyes, but corrected by a spectacle lens positioned in the anterior focal plane of the eye. In the emmetropic 60D Bennett Rabbetts schematic eye,5 the anterior focal point is 15mm in front of the corneal apex, a very similar value to that of the typical vertex distance. The lens is assumed to be centred on the optical and visual axis of the eye.
A ray from a distant object point, shown dashed, passing through the optical centre of the spectacle lens will be refracted by the ocular media to be parallel with the axis and hence the retinal image heights are now equal. For the less myopic eye, the ray PB intersected the spectacle lens at A, the angle APS being less than Ø, the angle the object subtends at the uncorrected eye since the incident ray from the object, being distant, must also have subtended angle Ø. For the more myopic eye, the ray PJ intersected the lens at H, closer to the axis than A, but the greater lens power, from Prentice’s rule means that the greater prismatic deviation is such that the incident ray also subtended angle ϑ, so all three rays are parallel in object space before reaching the lens.
This theoretical analysis is an expression of Knapp’s law, which effectively states that if a spectacle lens is placed in the anterior focal plane of the eye, then the retinal image size in the spectacle corrected eye remains constant, irrespective of the power of the spectacle lens (ignoring its shape factor magnification), assuming that the refractive error is caused be a difference in axial length.
The very important caveat is that this describes the physical dimension of the retinal image, not its physiological size. In an eye with a longer axial length, and hence a bigger area of retina, it is likely that the retinal receptors will be more widely spaced rather than having more receptors and the same density. In terms of retinal receptors covered by an image, as in figure 7, there may be similar numbers irrespective of the axial length. A reduced difference in perceived image size (measured as aniseikonia) with anisometropic people was found when they were corrected with contact lenses than when wearing their spectacle corrections.6
For an analogy, the very short focal length camera on a Smartphone may have a 12 megapixel image sensor 1/3 inch in size (about 8mm) with a pixel size of 1.22 microns.7 A compact camera might have a 2/3 inch sensor with a pixel size of 2.2 microns while the larger sensor on a digital single lens reflex camera might have a sensor 22 x 15mm with a pixel size of 5.2 microns, all for the same field of view.
Not all ametropia is caused by differences in axial length; there could be differences in the refractive power of the cornea or crystalline lens, ie refractive ametropia. The extreme case is that of the unilateral aphakic person, where the crystalline lens has been removed completely. Fortunately, the development of intra-ocular lenses has meant that ‘simple’ lens extraction for cataract is generally no longer undertaken and anterior chamber lenses could be used in cases of zonular weakness as in Marfan’s syndrome or trauma. Contact lenses are markedly superior to spectacle correction in these cases, but even they produce significant spectacle magnification at the powers needed even when calculated for the entrance pupil distance.
While textbooks on visual optics may divide refractive errors into axial and refractive ametropia for the purposes of retinal image sizes, there is a continuum of all the components of the focusing of the eye, ie of K-readings or corneal power, depth of the anterior chamber, crystalline lens power and vitreous chamber depth. For a reduced eye, these reduce to just the power and axial length.
Amblyopia and contact lenses
This article has shown that the differential prismatic effects in peripheral gaze and relative image sizes between the two eyes with spectacle lenses are eliminated with contact lens wear. Although the simple wearing of a spectacle correction is a good procedure to correct unilateral amblyopia, if the wearer is anisometropic these differential prismatic effects would be likely to perpetuate or even reinforce unilateral suppression to avoid diplopia. Hence contact lens wear is likely to be beneficial from both differential prism and image size points of view.8-10 Surprisingly, there may be differences between contact lens and orthokeratology on the binocular status of patients.10
Other optical effects
Equation 16 for spectacle magnification was derived for the wearer. Surprisingly, the same formula applies to the observer's view of the wearer’s eyes. Figure 8 is rather like figure 1, but in reverse. Since the vertex distance, d, is regarded as being positive when measured from the lens to the cornea, the object distance for the spectacle lens, l, should now be taken as (-d).
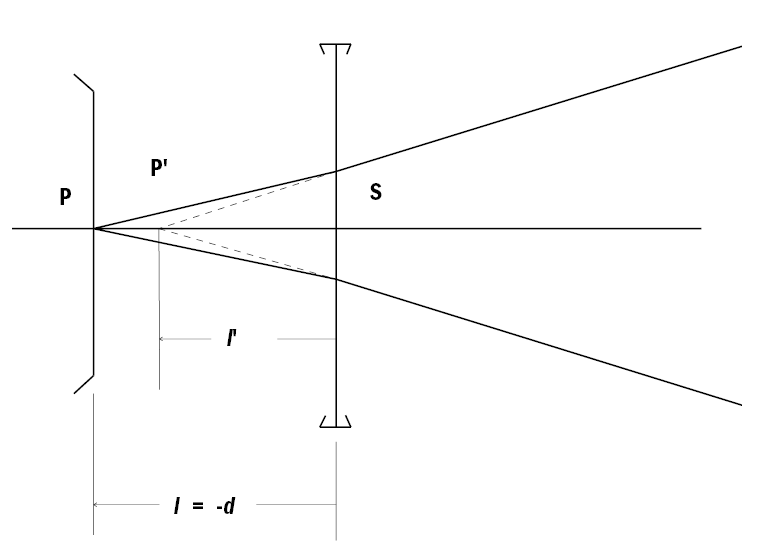
Figure 8: Diagram to illustrate the magnification of the eye, as seen by an observer
Hence:
The power factor will also have to be taken into account, since the image size is dependent upon the equivalent power of the spectacle lens, not its back vertex power.
The magnification produced by a spectacle lens inversely affects the field of view through the lens, a myopic wearer gaining field of view with the smaller image. The field of view is limited by the size of the frame and hence lens, combined with the prismatic effects of the lens near its edge. Figure 9 illustrates positive and negative lenses in front of an eye with centre of rotation Z. In the upper part of figure 9a) for the ‘macular field of view’ with the roving eye, the centre of rotation Z is imaged at Z', with the prismatic effects at the edge of the lens giving rise to a ring scotoma, shown shaded, while conversely the negative lens in figure 9b) acts like a field expander; indeed, depending upon the prescription and thickness of the rim of the spectacle frame, it may be possible to see objects both through the lens and, uncorrected, outside. The lower parts of the diagrams apply to the peripheral field of view with the stationary eye, with the reference point now being that of the eye’s entrance pupil, E.
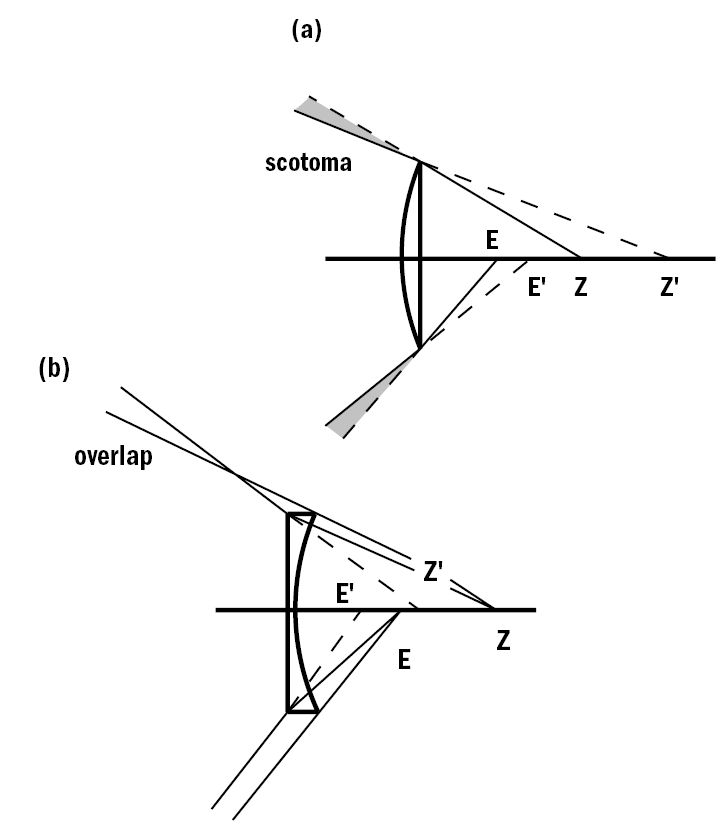
Figure 9: Field of view: upper part – the macular field with the moving eye, lower part the peripheral field with the static eye. a) the hypermetropic eye, b) the myopic eye. The narrower lines in b) denote the uncorrected view outside the edge of the lens
Because contact lenses move with the rotating eye, the macular field of view is limited only by the extent of ocular rotation. The peripheral field might be limited by the diameter of the front and back optic zones relative to that of the pupil, coupled with any decentration, particularly for RGP lenses.
Again, because contact lenses move with the eye, the peripheral aberrations of spectacle lenses such as distortion, tangential focal and mean oblique errors will not be present. The availability of free form spectacle lenses individualised to the wearer may reduce some of the effects, particularly with frames with a significant as-worn face form (wrap) angle or pantoscopic angle. These lenses, however, have to be positioned carefully in the frame when mounting.
The ability of contact lenses to move with the eyes means that the presbyopic wearer if fitted with monovision, progressive-power (varifocal) or, unless prism ballasted, bifocal lenses will be able to see near objects clearly in any direction of gaze. Such lenses, however, may compromise the sharpness of vision in all directions, which spectacle lenses will not, eg distance vision for driving. Also, the moderately myopic spectacle wearer has the ability to remove their spectacles, also to gain the ability to see close at any orientation. Moreover, the uncorrected -4.00 DS to, say, -7.00 DS myopic person has inbuilt magnification for near vision, particularly if the myopia is able to be supplemented by accommodation.
Summary
For the myopic wearer, contact lenses offer a larger retinal image, but at the expense of needing more accommodation and convergence in near vision than a spectacle wearer. The converse applies to the hypermetropic wearer. Their eyes will look a more normal size to the onlooker. In anisometropia, the absence of differential prismatic effects and the probability of more equal neural retinal image sizes is an advantage, and may help treatment of ambyopia.
Ronald Rabbetts is a retired optometrist and chairman of BSI spectacles (frames and lenses) committee and member of the sunglasses committee.
References
- Stone J. (1967) Near vision difficulties in non-presbyopic corneal lens wearers. Contact Lens, 1(2), 14-25
- Mei-Ju Chen, Yin-Tzu Liu, Chia-Chen Tsai, Yen-Cheng Chen, Ching-Kuang Chou, Shu-Mei Lee (2009) Relationship Between Central Corneal Thickness, Refractive Error, Corneal Curvature, Anterior Chamber Depth and Axial length. J. Chin Med Assoc, 72(3):133-137
- Rabbetts, RB (2007) Bennett and Rabbetts Clinical Visual Optics, 4th ed, Butterworth-Heinemann, Oxford, 248-249 (3rd Ed, 232-233)
- Mutti DO, Hayes JR, Mitchell GL, Jones LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD and Zadnik K for the CLEERE Study Group (2007) Refractive Error, Axial Length, and Relative Peripheral Refractive Error before and after the Onset of Myopia. Invest Ophthalmol Vis Sci, 48(6), 2510-2519
- Rabbetts, RB (1998 3rd Edn, 2007 4th ed) Bennett and Rabbetts Clinical Visual Optics, Chapter 12, Butterworth-Heinemann, Oxford
- Winn B, Ackerley RG, Brown CA, Murray FK, Prais J, St JMF. (1988) Reduced aniseikonia in axial anisometropia with contact lens correction. Ophthal Physiol Opt. 8, 341–344
- https://www.ephotozine.com/article/complete-guide-to-image-sensor-pixel-size-29652#APS-C-Sensor (accessed 1 Nov 2017)
- Roberts CJ and Adams GGW (2002) Contact lenses in the management of high anisometropic amblyopia. Eye, 16, 577-579
- Evans BJW (2006) Review: Orthoptic indications for contact lens wear. Contact Lens & Anterior Eye, 29, 175-181
- Moseley MJ, Fielder AR, and Stewart CE. (2009) Review: The Optical Treatment of Amblyopia. Opt Vis Sci, 86(6), 629-633
- Gifford K, Gifford P, Hendicott PL and Schmid KL. (2017) Near binocular function in young adult orthokeratology versus soft contact lens wearers. Contact Lens & Anterior Eye, 40(3), 184-189
