Amblyopia is the most common cause of monocular vision loss in children and young adults, with an incidence of 1 to 3.5% in the developed world.1 It is defined as diminished acuity in one or both eyes which persists after the correction of refractive error and the removal of any pathological obstacle to vision. Amblyopia is classed as a neural disorder as it results from the abnormal stimulation of the brain during the critical period of visual development.
The initial severity of the visual loss, the age of the patient at diagnosis, and the type and duration of treatment will all influence the final visual outcome for each patient. The cause may be one or a combination of the following three factors:
1 Light deprivation – when there is no stimulation of the retina. This is very uncommon, even in dense congenital cataract.
2 Form deprivation – when the retina receives stimulation but it is defocused, for example in uncorrected refractive error.
3 Abnormal binocular interaction – when incompatible images are formed on each fovea with all types of unilateral amblyopia. It may cause two separate images to form, eg in strabismus, or cause one of the images to be degraded, eg in anisometropia or cataract.
These three factors may be divided further (see below) and if more than one of these factors is present, the amblyopia maybe more severe and the prognosis for a good visual outcome decreases.
• Stimulus deprivation – similar to light and form deprivation above. Resulting from lack of adequate visual stimulation in early life. This can affect either one or both eyes. It may be virtually complete when very little light is able to enter the eye and therefore no image is formed (eg ptosis) or it may be partial when some light enters the eye and forms a sub-optimal image (eg corneal opacity, congenital cataract, vitreous opacity). Von Noorden2 speculated that bilateral stimulation deprivation amblyopia could result from congenital nystagmus when the constant movement across the retinae could prevent the formation of well-defined images.
• Strabismic amblyopia – the consequence of constant (or almost constant) unilateral strabismus with childhood onset. It is most commonly seen in esotropia but while many exotropias may be intermittent at first, they are at risk of decompensation to a constant deviation so should be monitored for any sign of amblyopia. Early onset/infantile esotropia is often alternating at first so there is less risk of amblyopia. However, after surgery some children may develop a fixation preference and thus amblyopia becomes more likely.
• Ametropic amblyopia – the consequence of bilateral insuperable refractive error (spherical or cylindrical) in each eye causing a blurred image at all distances. In high bilateral myopia there is likely to be reduced visual acuity but degenerative retinal changes may also be a factor.
• Meridional amblyopia – resulting from uncorrected astigmatism in one or both eyes. In this type of amblyopia, a clearer image is formed along the emmetropic axis but a blurred image forms along the ametropic axis. Gwiazda3 reported that meridional amblyopia could follow even the small amount of physiological astigmatism common in infancy, but clinically many patients have at least one dioptre of astigmatism and often considerably more than this.
• Anisometropic amblyopia – characterised by a significant difference between the refraction of the two eyes allowing one eye to have visual advantage at all distances. In all subtypes of anisometropic amblyopia accommodation will act to produce a clear image in the more emmetropic eye and there will be a blurred image in the more ametropic eye. A degree of aniseikonia is possible but few patients comment on this.
• Idiopathic amblyopia
Von Noorden4 reported on a group of amblyopic children who had no refractive error and normal binocular single vision apart from foveal suppression (elicited by the four dioptre test). While the amblyopia resolved well with occlusion therapy it repeatedly recurred on cessation of occlusion which he attributed to the continuing effect of inhibition from the normal eye and that these patients had been anisometropic at some time (also supported by Firth and Davis5).
Binocular competition
This is an integral part of normal binocular single vison, for example in retinal rivalry. Abnormal binocular competition occurs in all types of unilateral amblyopia (but not bilateral).
In stimulus deprivation amblyopia, competition is between the normal eye image and the ‘white noise’ degraded image from the affected eye. In strabismic amblyopia competition comes from visual confusion as images from different objects are projected from the fovea and are seen superimposed while in anisometropic amblyopia, competition arises from the defocused, distorted or different sized images of the fixation object being superimposed on the normal image.
Critical period
Amblyopia only develops during the critical period, when neural plasticity renders the visual system vulnerable to abnormal experience. Harwerth6 described several overlapping periods, each for a specific visual function and agreed with the work of Chavasse7 that there was a ‘period of flux’ lasting for the first eight years of life.
The most marked improvement in vision occurs in the first six months of life8 so it was originally thought that this is when a baby is most at risk from amblyogenic factors. However, later work has suggested that the visual system is not at risk for the first four months of life.9 Epelbaum et al10reported that the most improvement in strabismic amblyopia was seen if treatment was started before the age of three years, but vision could still improve up until 12 years. Other studies demonstrated that anisometropic amblyopic could be successfully treated until the age of eight years.11 However, more recent work has shown that treatment is worthwhile until much later than this.12
Early research
Causes and effects of amblyopia have been extensively studied in kittens and young monkeys, following the pioneering work of Hubel and Wiesel13 in the 1960s and Blakemore14,15 in the 1970s. They described the arrangement of cells in the striate cortex as ocular dominance columns, and demonstrated that abnormal visual experience results in alterations in the functional properties and anatomic architecture in the primary visual cortex (V1). V1 receives its main visual input from the lateral geniculate nucleus (LGN) of the thalamus. The group found that amblyopia was associated with a reduction in binocularly driven neurons in V1,
a reduction in V1 neurons driven by the amblyopic eye and increased binocular suppression. Importantly, they showed that more profound changes were seen in young animals with very early visual deprivation than in those with (later) aniso- or strabismic amblyopia.
Amblyopia was induced experimentally by:
- Unilateral or bilateral lid suturing (stimulus deprivation amblyopia)
- Unilateral strabismus (strabismic amblyopia)
- Defocusing one image with atropine or high convex lens(anisometropic amblyopia)
- Restricting visual stimuli to stripes orientated in one direction (meridional amblyopia)
The most severe amblyopia resulted from total deprivation of any stimulus following lid suturing, and effects of binocular deprivation were found to be less detrimental to the vision system than monocular suturing.
Crawford16 in 1978 coined the term ‘Visual Deprivation Syndrome’ to describe unilateral amblyopia. The syndrome comprises:
- Decreased visual acuity in the deprived eye
- Loss of binocular summation and stereopsis
- Reduction in the number of cortical neurones receiving input from the deprived eye and loss of binocularly driven cells
- A decrease in cell size in the relevant layers on the LGN
Blakemore showed that some of the cell changes could be reversed but only if the use of the deprived eye is enforced within the critical period by reverse suturing. This resulted in most of the LGN cells relating to the deprived eye regained their normal size.
While it must be acknowledged that all of the early work on amblyopia was carried out on monkeys and kittens, it has been established that the visual systems of monkeys and humans are very similar.1
Proof of anatomical changes in humans has been provided via post-mortem findings on a patient known to have anisometropic amblyopia. Von Noorden17 reported shrinkage of the layers of the LGN receiving input from the amblyopic eye, findings comparable with those reported in monkeys with anisometropic amblyopia.
Conclusions of research
- Severe stimulus deprivation amblyopia should be treated in the first weeks of life.
- Occlusion, optical and atropine penalisation can all cause visual loss if precautions are not taken (see section on cycloplegic drugs).
- Early correction of refractive error is important (particularly with astigmatism) in order to provide an orderly visual environment.
- Bilateral simultaneous occlusion for short periods is less disruptive than unilateral occlusion and was advocated by Harcourt18 for infants with bilateral cataracts prior to removal of the cataracts.
Amblyopia treatment
Before embarking on any treatment for amblyopia it must be established that there is no other pathological cause for reduced vision in either eye and any significant refractive error is corrected. In some cases, vision may improve sufficiently with refractive correction so that amblyopia therapy may be avoided.
The principle behind improving vision is to promote the use of the amblyopic eye(s). Traditionally this has been achieved by:
- Occlusion of the better eye
- Cycloplegic drugs +/- optical penalisation
- CAM visual stimulator (rarely used)
- Pleoptic treatment (rarely used)
Occlusion

Figure 1: Types of occlusive patch worn directly on the face
Occlusion may be of varying degrees:
- Total occlusion, all light and form – This is the most common form of occlusion therapy and is often the ‘first line’ treatment. It was first described by a physician, Thabit Al-Harrani, in 836 AD.19 An adhesive patch is worn directly on the skin so that no light can enter the occluded eye. Originally made from strong Elastoplast (that made removal difficult and often painful), today’s patches are made from much lighter, hypo-allergenic materials and are much more child friendly with different colours and designs (figure 1). Patches that fit around the glasses, such as Eze-patch and Kay fun patch (figure 2) also come into this category, but need careful fitting to ensure no light can enter the fixing eye.

Figure 2: Patch worn over spectacles (picture courtesy of Kay Pictures Ltd, www.kaypictures.com)
- Total occlusion, excluding form – light is allowed through the spectacle lens but no form (not even the largest logMAR letter) should be identifiable. A frosted spectacle lens or Blenderm tape applied to the lens constitutes total occlusion.
- Partial occlusion – Some form is appreciated but acuity is diminished. A Bangerter foil (figure 3a and b) that reduces the vision by a set amount, or sector occlusion covering only part of the lens (for example, occluding the lower half of a spectacle lens to promote use of the amblyopic eye for close work) fall into this category.

Figure 3a: Left lens occluded with Bangeter foil
Figure 3B: View with Bangeter foil occlusion
Cycloplegic Drugs
Here, the principle is to blur the vision of the better eye by preventing accommodation and reducing depth of focus, this it is more effective for near fixation. Atropine 1% or 0.5% either as a drop or ointment is most commonly used, and the action of the drug is maintained by instilling on alternate days or only for weekend use as reported by the PEDIG group.29
Care must be taken when instilling atropine to avoid ingestion via the nasolacrimal duct, and information must be given to parents regarding systemic side effects.
Optical Penalisation
The use of lenses is to both blur the vision of the better seeing eye and augment the vison in the amblyopic eye. The eye can be penalised for near, distance or all distances and is often combined with cycloplegia.
Choice of treatment
Main factors to consider when selecting a treatment choice are:
- Age of the child – Due to the critical period, it is thought that the younger the patient, the more rapid and better the response. This is particularly true for cases of stimulation deprivation amblyopia. However, recent studies13 have shown that good results can still be achieved in older children, particularly those with anisometropic amblyopia which suggests more plasticity of the visual system than previously thought.
- General health – Consideration must be made for children with associated systemic conditions for example, children with hearing impairment who may be reliant on good vision for lip-reading, children with skin conditions such as severe eczema or epidermolysis bullosa in whom the wearing of spectacles and adhesive patches may be impossible and children with limited mobility who may be affected if the vision is reduced.
- Social factors – Amblyopia therapy is difficult and requires a lot of effort from both the child and the family/carers. Frequent visits to the hospital are needed which has implications both financially and on the care of other family members. It is crucial that those caring for the child (parents and school/nursery teachers) understand the impact of reduced vision on the functioning of the child so that adaptations can be made.
- Compliance – It is imperative that the child and carers understand the need for treatment and implication of not treating amblyopia. Written information, positive reinforcement, involvement of other professionals (teachers, GP etc) and provision of alternative treatments can all help with compliance
- Nystagmus – If a child has a latent component to their nystagmus, the amplitude and frequency of the nystagmus is likely to increase when occluding the better seeing eye. As this settles over time, it may be beneficial to prescribe whole days per week of occlusion, for example one or two days per week, rather than a couple of hours each day. This provides a prolonged period when the eyes are most still.
How to treat
Traditionally, eye care professionals have treated amblyopia based on the level of acuity and the age of the child, and most treatment plans were based upon experience and ‘gut feeling’ and were individualised to each patient.
A Health Technology Assessment (HTA) report published in 199720 concluded that the evidence for the value of screening for amblyopia and strabismus did not support any expansion of the existing screening programme, and highlighted specifically the lack of evidence on the long-term impact of amblyopia. This report was partly responsible for the formation of the Paediatric Eye Disease Investigator Group (PEDIG) later in 1997. The group was formed to investigate the treatment modalities for amblyopia by using randomised trials in a multi-centre format. The amblyopia treatment studies from PEDIG and other groups around the world including the UK based Monitored Occlusion Treatment Amblyopia Study (MOTAS) group (see below) have revolutionised the treatment of amblyopia and now form the evidence base for treatment choices.
Over the past 20 years the PEDIG group has published results of trials detailing:
- Patching versus atropine (2002 and 2008)21,22
- Two hours compared with six hours patching for moderate amblyopia (2003)23
- Six hours versus full-time patching for severe amblyopia (2003)24
- Recurrence risk on cessation of treatment (2004)25
- Use of refractive correction alone for anisometropic amblyopia (2006)26 and for strabsimic amblyopia (2012)27
- Two hours patching +/- near activities (2005)28
- Weekend atropine to treat severe amblyopia (2009)29
- Early treatment (under five years) versus after seven years (200830 and 201131)
The main take home points from the PEDIG trials are:
- Treatment for both strabismic and anisometropic amblyopia is successful – around 75% of children under seven years of age achieved resolution of amblyopia with either patching or atropine
- Best optical correction is essential to successful treatment
- Patching and atropine are equally effective for treating moderate amblyopia
- If one treatment modality fails, an alternative method can be initiated
- Younger age is associated with better final acuity, but treatment should be attempted in older children
- VA needs to be monitored closely on cessation of treatment to identify any regression
- Amblyopia treatment has a significant social and physical impact on the child and the family.
The MOTAS group32 looked at the dose response relationship in amblyopia and identified three phases: baseline, refractive adaptation and occlusion. They found that:
- Refractive adaptation period was 18 weeks so occlusion should not be started before the end of this period. This means that children may commence occlusion at a higher acuity level which has better psychosocial and compliance factors, and some children may not need any occlusion at all.
- Most improvement in acuity was achieved by six weeks of occlusion
- Equal final outcomes occurred with two to six hours daily occlusion but the most rapid improvement occurred with a higher dose of patching (as per PEDIG).
Together with the Randomized Occlusion Treatment Amblyopia Study (ROTAS) group,33 MOTAS34 used an objective measure of compliance with occlusion and found overall concordance with treatment to be 48%.
Despite the new robust evidence based treatment options, Jin35 (2013) found that attitudes were hard to change when looking at the PEDIG recommendations in clinical practice and reported that less than 25% of children were prescribed patching in accordance with PEDIG guidelines. This was backed up by Newsham36 (2010) who reported that only 15% UK head orthoptists changed practice due to PEDIG.
Risks of Treatment
- Occlusion amblyopia – most likely to occur when using high levels of total occlusion in young infants (for example with unilateral aphakia). In the majority of cases, acuity can be recovered with careful treatment.
- Intractable diplopia – a rare but theoretically possible occurrence in older children with strabismic amblyopia, due to the disruption of the suppression mechanism
- Dissociation of latent or intermittent strabismus, for example, a child with a distance exotropia who was previously binocular for near fixation may become manifest at near following occlusion – most likely in children under five years or older children with poor motor fusion
- Recurrence of amblyopia – careful tapering of occlusion once best acuity is achieved has been shown to prevent recurrence of amblyopia (PEDIG 2004)26
Looking forward
With the lack of compliance with all forms of amblyopia treatment being a consistent problem, attention is now shifting to alternative forms of therapy that are both more ‘user-friendly’ and more useful across all age groups, including adults.
Amblyz eyeglasses (figure 4), manufactured by the 3-D Solutions company XPAND, work on the same principle as other methods of treatments: obstructing the stronger eye in order to stimulate the weaker eye to develop.
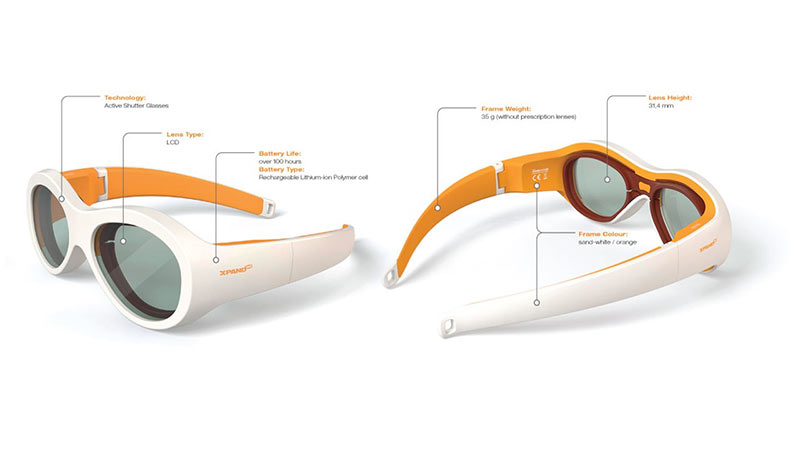
Figure 4: Amblyz occluding glasses (image courtesy of attraining.org)
The glasses obstruct the strong eye in automatic, intermittent 30 second intervals using an electronic shutter attached to one of the lenses, creating an opaque lens. The shutter allows the lens to alternate between transparent and its opaque state at a prescribed rate, enabling the weaker eye to develop, and eventually regain its normal vision.
Researchers at the Glick Eye Institute recruited 33 subjects aged three to eight years and compared treatment with two hours daily occlusion with patches and four hours daily Amblyz wear.37 After three months of treatment, both groups showed the same amount of improvement in visual acuity – two lines.
The use of flicker to stimulate the visual system is also being investigated. Certain flicker frequencies have been found to break suppression.38 Eyetronix flicker glasses (Good-Lite) (figure 5) use liquid crystal technology to deliver precisely controlled alternate occlusion using these flicker frequencies. Instead of occluding or penalising one eye via a patch or drops, the theory is that using flicker can gently stimulate the visual system and encourage both eyes to naturally work together, ultimately aiding in the restoration of binocular vision and depth perception.

Figure 5: Eyetronix flicker glasses (image courtesy of Good-Lite)
A recent study 38 tested 24 patients aged six to 17 years with mild to moderate anisometropic amblyopia. The patients wore the glasses for one to two hours per day and showed significant improvement in acuity and stereopsis, even in the older age group. There appeared to be a high level of compliance and both parents and patients felt the glasses were easy to use.
The Eyetronix study highlights the more recent understanding of neural plasticity and challenges the thought that the visual system has completed its development by the age of around 10 years.
The flicker glasses also take a binocular approach to amblyopia treatment – something that is driving new treatment options. Emphasis is on the use of binocular stimulation to not only improve acuity, but also binocular functions.
The use of video games and similar forms of visual stimulation is thought to combat some of the motivational problems associated with traditional amblyopia treatments, and have very few side effects.
Dichoptic viewing, in which each eye views a separate and independent field, was first used to measure suppression, but has now been modified by researchers at McGill University39,40 to a treatment based on the video game Tetris (figure 6). This aims to hold the patient’s attention over a prolonged period of time. When viewed dichoptically, the amblyopic eye sees moving blocks of high fixed contrast, while the fellow (fixing) eye see the static ground blocks which are of low and variable contrast. This dichoptic perceptual learning which was designed to strengthen binocular combination and reduce suppression has been shown to improve both acuity and stereopsis in amblyopia children and adults.

Figure 6: Dichoptic treatment with the Tetris video game (image courtesy of McGill University Health Cenre)
The same group from McGill University have shown that vision in adults with amblyopia can be improved following application of repetitive transcranial magnetic stimulation (rTMS).41 rTMS is a non-invasive technique for modulating excitability and inhibition in the visual cortex. The group reported that the effects of a single dose of rTMS are transient, however, repeated doses may lead to more sustained improvement in acuity, and it may have a role alongside other treatment modalities.
Another new treatment is Interactive Binocular Treatment (I-BiT)42,43 which again works by presenting different information to each eye. In this instance the patient plays a computer game or watches a DVD via virtual reality technology. The amblyopic eye sees the more interesting part of the programme and may have a task to perform such as avoiding obstacles or collecting prizes, while the fellow eye only sees the less interesting part of the background. Both eyes may be receiving an image simultaneously, but the brain has to use the weaker eye to properly play the game or watch the DVD.
Both of these new treatments allow treatment to take place without the need for the non-amblyopic eye to be patched. The I-BiT treatment uses shutter glasses to allow each eye to only see the intended image. The right and left eyes are alternately shut off so that only one eye can see the screen at a time, but this happens so rapidly that the brain does not appreciate that each eye is being stimulated separately, and the patient is not aware of any flickering. A multi-centre randomised controlled trial44 has shown modest improvements in amblyopia, and the treatment was well tolerated by patients aged four to eight years.
In a similar study, the PEDIG group performed a multi-centre randomised controlled trial comparing one hour per day of a binocular iPad game with two hours per day occlusion in 385 children.45 While there was an improvement in visual acuity in both groups, it was shown that the iPad treatment was not as effective as conventional occlusion.
Our improved understanding of the mechanisms of amblyopia, coupled with the rapid expansion in innovation and technology is allowing the development of new treatment modalities which are more engaging and may result in better compliance and thus better outcomes for patients with amblyopia.
Bronwen Walters is Lead Orthoptist at Great Ormond Street Hospital
The author would like to thank Danielle Eckersley, lead orthoptist at Moorfields Croydon for assistance with this article.
References
- Facts about amblyopia. National Eye Institute 2013; September
- Von Noorden G K Amblyopia: a multi-disciplinary approach. Invest Ophthalmol Vis Sci 1985; 26: 1704-1716
- Gwiazda J et al Meridional amblyopia does result from astigmatism in early childhood. Clinical Visual Science 1986; 1: 145-152
- Von Noorden G K Idiopathic Amblyopia. American Journal of Ophthalmology 1985; 100: 214-217
- Firth A Y and Davis H Idiopathic amblyopia – the role of anisometropia in aetiology : a case report. Binocular vision and eye muscle surgery quarterly 1994; 9 (2) 129-132
- Harwerth R S et al Multiple sensitive periods in the development of the primate visual system. Science 1986; 232 235-238
- Chavasse F B Worths squint or the binocular reflexes and the treatment of strabismus 115 -116 Balliere-Tyndall London
- Dobson V and Teller D Y Visual acuity in human infants: a review and comparison of behavioural and electro-physiological studies. Vision Research 1978; 18: 1469-83
- Held R Normal visual development and its deviations. In Strabismus and Amblyopia 1988 : Werner Green International Symposium Series 247-258
- Epelbaum M et al The sensitive period for Strabismic amblyopia in humans. Ophthalmology 1993; 100: 323-327
- Hardman Lea S J et al. The sensitive period for anisometropic amblyopia. Eye 1989; 3:783-790
- PEDIG Group Randomized Trial of Treatment of Amblyopia in Children Aged 7 to 17 Years. Arch Ophthalmol. 2005;123(4):437-447
- Hubel D and Wiesel T Laminar and columnar distribution of geniculo-cortical fibres in the macaque monkey. J Comparative Neurology 1972; 146:421-450
- Blakemore C and Cooper G Development of the brain depends on the visual environment. Nature 1978; 228: 477-478
- Blakemore C et al The physiological effects of monocular deprivation and their reversal in the monkeys visual cortex. Journal of Physiology 1978; 283: 223-262
- Crawford M The visual deprivation syndrome. Transactions of the American Academy of Ophthalmology 1978; 85: 465-469
- Von Noorden G K et al. The Lateral Geniculate Nucleus in human anisometropic amblyopia. Invest Ophthalmol Vis Sci 1983; 24: 788-790
- Harcourt R et al Discussion in:Strabismus and Amblyopia: 1988 Wenner Gren International Symposium Series
- Loudon S and Simonz H The history of the treatment of amblyopia. Strabismus 2005; 13 (2) 93-106
- Snowden S K and Stewart-Brown S Pre-School Vision Screening. Health Technology Appraisal 1997; 1: 8
- PEDIG A randomized trial of atropine vs. patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120(3):268–278
- PEDIG Patching vs. atropine to treat amblyopia in children aged 7-12 years. Arch Ophthalmol. 2008;126(12):1634-1642
- PEDIG A randomized trial of patching regimes for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121(5):603-611
- PEDIG A randomized trial of patching regimes for treatment of moderate amblyopia in children. Ophthalmology 2003;110:2075-87
- PEDIG Risk of recurrence of amblyopia after cessation of treatment. J AAPOS 2004; 8 : 420-428
- PEDIG Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology. 2006 June ; 113(6): 895–903.
- PEDIG Optical treatment of strabismic and combined strabismic –anisometropic amblyopia. Ophthalmology. 2012 January; 119(1): 150–158.
- PEDIG A randomized pilot study of near activities versus non-near activities during patching therapy for amblyopia. J AAPOS. 2005 Apr;9(2):129-36
- PEDIG Group Treatment of severe amblyopia with weekend atropine – results from two randomised controlled trials. J AAPOS 2009; June (13) 3: 258-263
- PEDIG A randomized trial of near versus distance activities while patching for amblyopia in children 3 to < 7 years old. Ophthalmology. 2008 Nov; 115(11): 2071–2078.
- PEDIG Effect of age on response to amblyopia treatment in children. Arch Ophthalmol. 2011 Nov;129(11):1451-7
- MOTAS Co-operative Refractive Adaptation in amblyopia –qualification of effect and implications for practise. Br J Ophthal 2004; Dec 88 (12): 1552-1556
- ROTAS Co-operative Objectively monitored patching regimen for the treatment of amblyopia:a randomised trial. BMJ 2007; Oct 6; 335 (7622): 707
- Stewart C et al Treatment dose response in amblyopia – the Monitored Occlusion Treatment of Amblyopia Study. Invest Ophthalmol Vis Sci 2004; 45:3048-3054
- Jin Y P et al Clinical translation of recommendations from randomized clinical trials on patching regimen for amblyopia. Ophthalmology 2013; 120 (4); 657-662
- Newsham D The effect of recent amblyopia research on current practise in the UK. Br J Ophthalmol 2010; 94 (10): 1352-1357
- Wang J et al A pilot randomized clinical trial of intermittent occlusion therapy liquid crystal glasses versus traditional patching for treatment of moderate unilateral amblyopia. J AAPOS 2016; 20(4): 326-331
- Hussey E et al The Eyetronix flicker glass amblyopia treatment study: acuity, binocularity, compliance and satisfaction. Vision development and Rehabilitation 2015 Vol 1 Issue 1
- Li S et al Dichoptic movie viewing treats childhood amblyopia. J AAPOS 2015; 19 (5): 410-405
- Li S et al Dichoptic training enables the adult amblyopic brain to learn. Current Biology 2013; 23 (8):308-309
- Thompson B et al Brain plasticity in the adult – modulation of function in amblyopia with Repetitive Transcranial Magnetic Stimulation (rTMS). Current Biology 2008;22 (14): 1067-1071
- I-BiT Study Group Interactive Binocular treatment (I-BiT) for amblyopia : results of a pilot study of a 3D shutter glass system. Eye 2013; 27: 1077-1083
- Foss A et al Evaluation and development of a novel binocular treatment (I-BiT) system using video clips and interactive games to improve vision in children with amblyopia: a study protocol for a randomised controlled trial. Trials 2014; 14:145
- Herbison N et al Randomised controlled trial of video clips and interactive games to improve vision in children with amblyopia using the I-BiT system. Br J Ophthalmol 2016; 100: 1352-1357
- PEDIG Group The effect of a binocular IPad game versus part time patching in children aged 5-12 years with amblyopia : a randomised controlled trial. JAMA Ophthalmol 2016; Dec 134 (2):1391-1400
