Daily disposable (DD) contact lenses continue to gain widespread acceptance with patients and with eye care practitioners. Worldwide around four in 10 soft lenses fitted in 2017 (37%) were for daily replacement.1 In the UK, the latest data for 2017 show that DDs accounted for two-thirds of new soft lens fits (66%).2
Although more DD options in silicone hydrogel (SiHy) materials are now available, the proportion of SiHys prescribed in this category still lags behind the proportion of reusable lenses that are SiHy.1
The enduring satisfaction with hydrogel materials relies heavily on their performance. In a recent clinical study comparing lenses made from SiHy and hydrogel materials, Diec et al3 reported there were ‘no clinically significant differences in physiological variables, vision and contact lens fitting characteristics’ between the materials.
‘Neither material type was shown to be superior in comfort,’ these authors say. They conclude that the outcomes ‘suggest that the choice of material for this modality [DD] may be based on patient and practitioner preference.’
The continuing success of etafilcon A DDs has been reflected in positive reports on safety outcomes and ocular health with these lenses.4 New studies are now emerging that support the excellent record of etafilcon A DD lenses for successful wear with minimal problems (see table 1).
Table 1: Key points from the latest published clinical studies
Focus on what matters
Despite this proven success, some eye care practitioners may still have concerns about fitting hydrogels for new wearers or refitting SiHy wearers into hydrogels. The belief that SiHy materials per se are healthier than hydrogels may be driven by the perception that ‘the higher the oxygen transmissibility (Dk/t) the better’.
Indeed, it is known that as Dk/t increases, other measures of oxygen that are more clinically relevant – such as anterior corneal oxygen flux (the amount of oxygen that passes through a unit area of lens in a given time) or oxygen consumption by the cornea (a direct index of corneal oxygen metabolism) – quickly plateau (figure 1).5
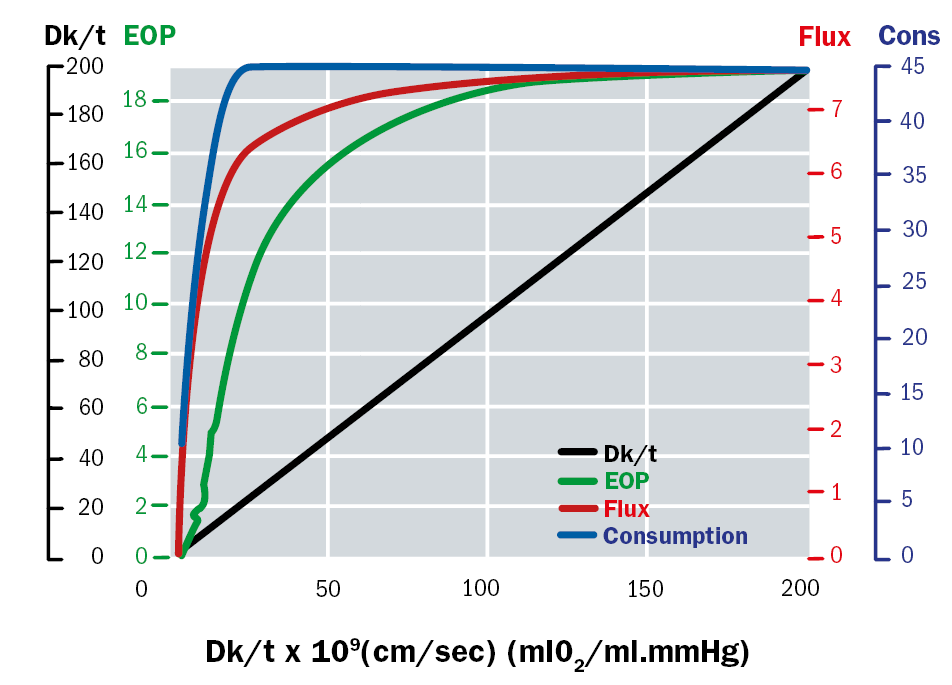
Figure 1: Combined graph showing Dk/t, equivalent oxygen percentage (EOP), anterior corneal oxygen flux (ul/cm2h) and consumption (nl/cm3sec) as a function of Dk/t for the open eye 5
At a Dk/t of approximately 20 units, the central cornea gets all the oxygen it needs for normal functioning in the open-eye state. Therefore, corneal oxygen consumption with etafilcon A lenses (Dk/t of 25.5 centrally) is the same as with lotrafilcon A lenses (Dk/t of 175) under open-eye conditions, despite their very different lab-based transmissibility measurements.5
In fact, the only solid evidence of a benefit from a central Dk/t >20 is a small and likely not clinically relevant reduction in limbal hyperaemia,6 and a reduction in peripheral corneal swelling, which may be important for patients who are predisposed to vascularisation with the thicker designs of some toric lenses.7
There are patients who do better in high Dk/t SiHy lenses (although, in most cases, this is probably not due to increased oxygen supply), just as there are patients who do better in hydrogels. Prescribing according to patient needs and comfort preferences is more likely to lead to success than arbitrarily emphasising one characteristic – Dk/t – that has relatively little impact on performance and no positive impact on comfort.
Switching to hydrogels
A recent study, conducted at the Center for Contact Lens Research at the University of Waterloo, examined physiological response and clinical performance in subjects switched from their usual SiHy lenses to a multifocal etafilcon A lens.8
The study included 39 habitual SiHy lens wearers, with the majority 70% wearing reusable SiHy multifocals. The mean age of the subjects was 54.5 ±7 years. Ocular physiology was assessed at baseline and at four weeks after six hours of open-eye wear. Success factors such as visual acuity, subjective comfort and vision were evaluated.
No clinically significant differences in ocular physiological responses to lens wear were found between baseline habitual reusable SiHy wear and after four weeks of open-eye DD wear of multifocal etafilcon A lenses.
Importantly, comfort and performance were superior with the hydrogel lens. After four weeks of multifocal etafilcon A DD lens wear, the overall CLUE comfort score (Contact Lens User Experience9 – a composite index of multiple comfort questions, validated by the US Food & Drug Administration Guidance on Patient Reported Outcomes10) was significantly higher (72.2 vs 62.1) than at baseline and more subjects agreed with the statement ‘these lenses were comfortable at the end of the day’ (82% vs 69%).
Key clinical signs
The study reveals similarly positive results for these two key clinical signs of hypoxic stress: corneal swelling and limbal hyperaemia. After 6 hours of lens wear, for each of four corneal locations, corneal thickness at day 28 and baseline (SiHy wear) was clinically equivalent (figure 2), for myopes and hyperopes alike.8
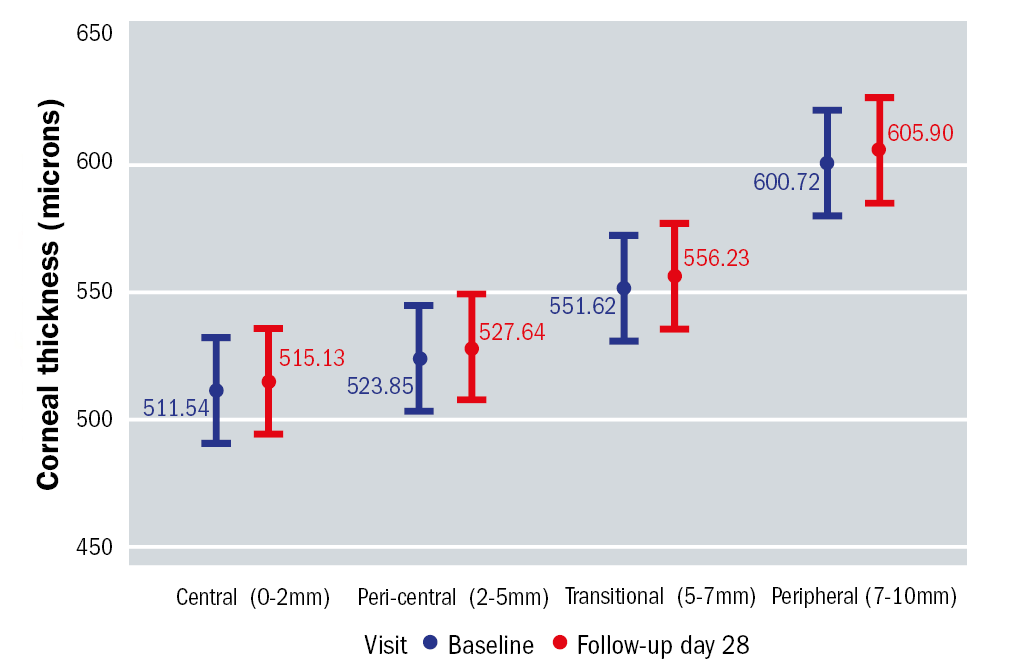
Figure 2: Corneal swelling (μm) in four locations at baseline (SiHy wear) and after four weeks of etafilcon A multifocal DD lens wear (follow-up), as measured by OCT 8
This result is important when considering whether to recommend a switch to hydrogel lenses to existing SiHy wearers in the presbyopic age group.
Findings for limbal hyperaemia provide even more confidence for practitioners. There was no significant clinical difference in mean bulbar conjunctival hyperaemia with the etafilcon A DD multifocal contact lens compared to the habitual SiHy lenses (figure 3).8
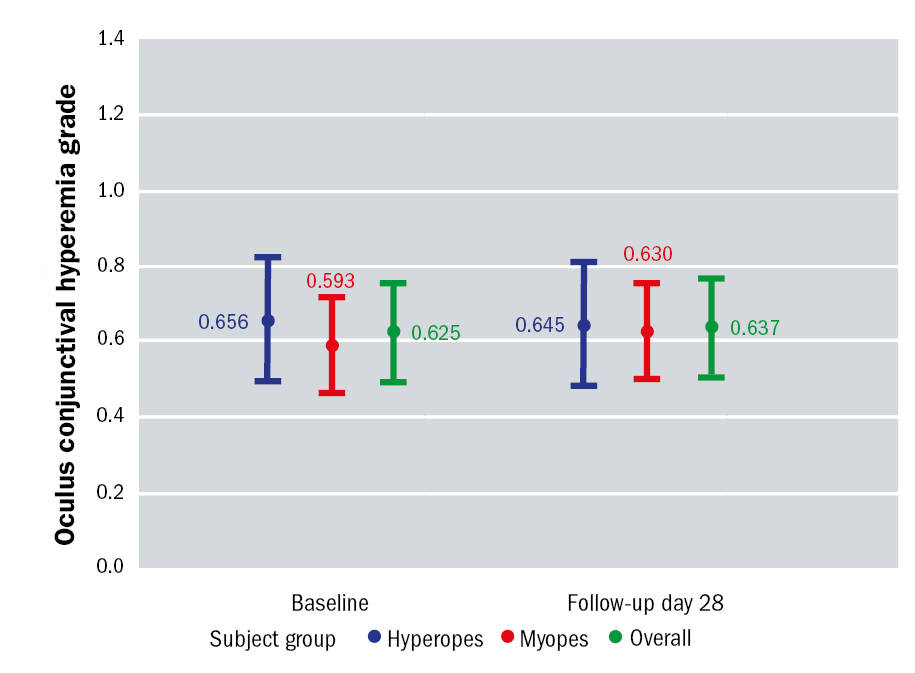
Figure 3: Mean limbal conjunctival hyperaemia at baseline (SiHy wear) and after 4 weeks of etafilcon A multifocal DD lens wear (follow-up), as measured by OCT 8
In fact, the levels of mean bulbar as well as mean limbal hyperaemia at day 28 compared to baseline were equivalent. Again, the same was true in both hyperopes and myopes. The levels of hyperaemia observed were consistent with that seen in non-lens wearing adults (≤grade 1).8
Taking the stress test
Previous studies of these two key clinical signs of hypoxia have provided reassurance that there is more to ocular health than Dk/t and demonstrated the excellent performance of etafilcon A.
In the first study researchers compared open-eye corneal swelling between etafilcon A DD lens and no lens in 24 patients.11
After eight hours of open-eye wear, central and peripheral corneal swelling along the horizontal meridian with etafilcon A was <1.5%, clinically equivalent to that observed with no lens. Conjunctival hyperaemia was also clinically unremarkable under both conditions.
A second study compared these same signs of hypoxic stress in 36 habitual contact lens wearers after seven days’ wear of three, reusable lens types: etafilcon A,and the SiHys lotrafilcon B, and comfilcon A.12 Central corneal thickness and limbal hyperaemia were measured two hours after waking and after six to eight hours’ wear.
The etafilcon A reusable lens resulted in corneal de-swelling throughout the day, as did the SiHy lenses, and was within 0.85% mean swelling of the SiHys. Overall (and by quadrant) mean limbal hyperaemia with etafilcon A was within a 0.5 grade step of that induced by the SiHys. Equivalence of etafilcon A with respect to the two SiHy lenses for these key measures of hypoxic stress was demonstrated.
Positive safety outcomes
If ocular physiology findings for etafilcon A DDs are reassuring, results for the safety profile of these lenses are also very positive.
The ‘TEMPO’ (Acuvue TruEye or 1 Day Acuvue Moist Performance Overview) study measured the incidence of adverse events by post-market surveillance registry of wearers fitted with etaflcon A DD.13 This 12-month observational study of 570 patients (equivalent to 471 patient years of lens wear), found there were no symptomatic corneal infiltrative events (CIEs) or other serious adverse events (AEs) (0.0%/year) and only three non-serious events (0.6%/year).
This observational/surveillance registry relied on patient reports of symptomatic adverse events that led them to seek clinical care. The results should be considered in conjunction with other clinical results on the safety and efficacy of DD etafilcon A contact lenses, which also generally show low rates of such events. It should be noted that although no symptomatic infiltrative events were reported in the TEMPO study, such events can occur with DD lenses, including etafilcon A DD, as noted in the product labelling.
The overall CIE rates found in the TEMPO registry are significantly lower than found in previous reusable lens studies, such as an annualised incidence of 4.0% in a retrospective chart review of mainly daily wear hydrogel and SiHy wearers, and 5.0% in a prospective trial with daily wear reusable SiHys.14,15
Additional analysis of the TEMPO study has since explored the influence of age on performance outcomes.16 Among 86 wearers aged over 40 (24% men, age 50.2±7.1 years) completing the registry, 76% were new to DDs and 8% were neophytes.
Existing contact lens wearers older than 40 years experienced many benefits from refitting with etafilcon A; changing to the hydrogel DD significantly improved overall opinion of contact lenses, improved dry eye symptoms, and maintained average and comfortable wear time.
Rates of other AEs in the TEMPO registry were also very low in comparison with prior studies using different designs or other modalities.
This finding is supported by an independent, retrospective analysis that looked at 28 lens/solution combinations, each tested on approximately 40 patients wearing lenses on a daily wear basis for a three-month period.17 Lenses were frequent replacement and DDs, hydrogels and SiHys. Solutions included hydrogen peroxide and multipurpose.
The overall AE rate was 3.6 events per 100 participant-months. Rates were low for the four DD lenses tested and significantly lower in DDs compared with reusable daily wear lenses, at 3.1 vs 10.9. The only lens in the study that did not have any reported AEs was etafilcon A DD, although the study did not show statistically significant differences between the DDs evaluated.
Lower incidence of microbial keratitis (MK)
A new study of MK in DD wearers helps build further confidence on safety outcomes with etafilcon A DDs in particular.
A two-year case control study at Moorfields Eye Hospital in the UK and a one-year national surveillance study in Australia and New Zealand identified new cases of contact lens-related MK in wearers using DD and other soft contact lenses.18 Self-administered (cases) or telephone-administered (controls) questionnaires were used to identify potential risk factors for MK, expressed as an odds ratio (OR).
A total of 963 DD wearers were identified, from which 67 MK cases and 374 controls were sampled. Independent risk factors for all and for moderate/severe MK were: wearing contact lenses every day vs less frequent use (OR 10.4x), any overnight wear (OR 1.8x), less frequent hand washing (OR 1.8x) and smoking (OR 1.3x).
But the study also found that risk varied with DD lens type and it would seem that certain DDs had lower rates. Using etafilcon A as the referent, a nelfilcon A DD had an OR of 3.98 for all presumed MK (and 4.83 for moderate/severe MK), and a hilafilcon B DD had an OR of 2.06 (and 2.61 respectively) (figure 4).
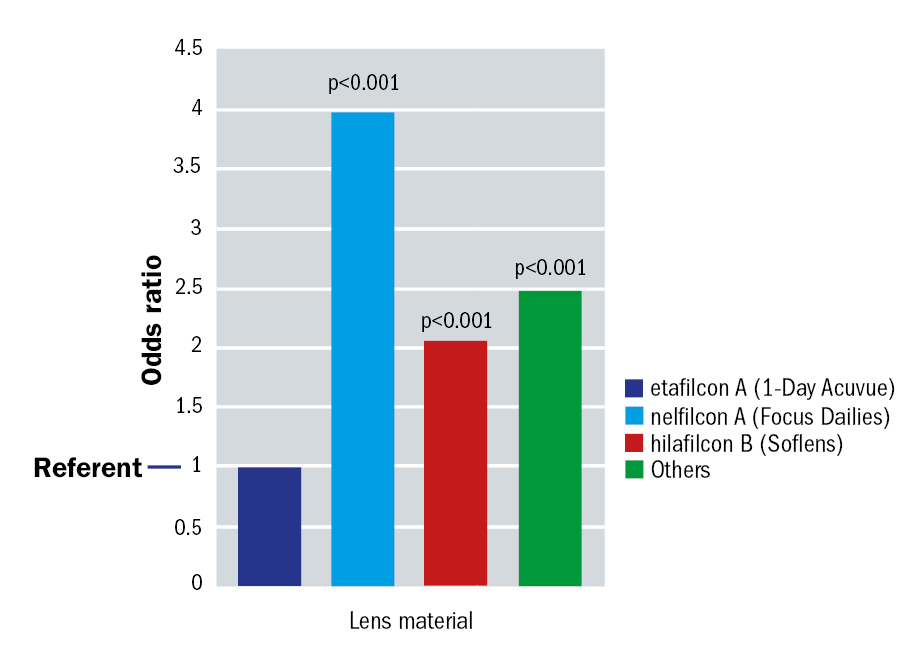
Figure 4: Additional risk factors for all presumed microbial keratitis identified by multiple logistic regression analysis 18
The authors observe that ‘it is unclear why certain DDs are protective for the risk of infection,’ and that ‘some types of DD are more difficult to remove than others, which may increase the risk of mechanical complications’. They conclude that lens type, material properties and design are likely to play a role in the aetiology of MK in the DD modality.
These results add to the analysis of a previous case-control study of MK rates in the UK that again found differences between DDs, again citing handling difficulty as a possible cause and the nelfilcon A lens as more difficult to remove than the etafilcon A lens.19
It is important to note that both the nelfilcon A (Focus Dailies) lenses and etafilcon A (1-Day Acuvue) included in this study have altered since these studies were conducted. The nelfilcon A lenses now have a larger base curve and diameter with two added wetting agents. 1-Day Acuvue (etafilcon A) has since been replaced by 1-Day Acuvue Moist, having the same base material and design with the addition of polyvinylpyrrolidone (PVP).
Conclusions
Both SiHy and high-quality hydrogel contact lenses can provide adequate oxygen for healthy daily wear. Both materials will likely continue to play an important role in contemporary contact lens practice. Practitioners might consider that having ‘extra capacity’ for oxygen transmissibility is a reassurance, however, the balance of all the material properties of the lens should be considered to ensure that the best material for an individual patient is selected rather than basing the decision on a single parameter.
Etafilcon A hydrogel DD lenses have an excellent record for comfortable, successful wear with an excellent safety profile. These lenses have minimal impact on ocular physiology and supply sufficient oxygen levels for open-eye daily wear. Many studies have now shown that these lenses are associated with low rates of CIEs, adverse events and infections.
With evidence from recent studies, eye care practitioners can continue to be confident when prescribing etafilcon A DD lenses to help maintain ocular health.
Dr Noel Brennan is Clinical Research Fellow and Global Platform Lead Myopia Control at Johnson & Johnson Vision. David Ruston is Director Global Professional Education and Development at Johnson & Johnson Vision.
References
- Morgan PB, Woods C, Tranoudis IG et al. International contact lens prescribing in 2017. Contact Lens Spectrum 2018;33:1 28-33.
- Morgan P. The trends in UK contact lens prescribing 2017. Optician 2017;254:6626 12-14.
- Diec J, Tilia D and Thomas V. Comparison of silicone hydrogel and hydrogel daily disposable contact lenses. Eye Contact Lens 2017. doi: 10.1097/ICL.0000000000000363. [Epub ahead of print].
- Chalmers R and Brennan N. New findings with etafilcon A daily disposable contact lenses. Optician 2016;251:6542 28-33.
- Brennan NA. Beyond flux: total corneal oxygen consumption as an index of corneal oxygenation during contact lens wear. Optom Vis Sci 2005;82:6 467-72.
- Diec J, Lazon de la Jara P, Willcox M et al. The clinical performance of lenses disposed of daily can vary considerably. Eye Contact Lens 2012;38:5 313-8.
- Morgan PB, Brennan NA, Maldonado-Codina C et al. Central and peripheral oxygen transmissibility thresholds to avoid corneal swelling during open eye soft contact lens wear. J Biomed Mater Res Part B Appl Biomaterials 2010;92:2 361-5.
- Moezzi A, Varikooty J, Luensmann D et al. Open-eye clinical performance of etafilcon A multifocal daily disposable hydrogel contact lenses compared to habitual silicone hydrogel lens wear. Optom Vis Sci 2016 e-abstract 16559.
- Wirth RJ, Edwards MC, Henderson M et al. Development of the Contact Lens User Experience: CLUE Scales. Optom Vis Sci 2016;93:8 801-8.
- Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. https://www.fda.gov/downloads/drugs/guidances/ucm193282.pdf.
- Moezzi A, Varikooty J, Schulze M et al. Open-eye corneal swelling with etafilcon A daily disposable hydrogel contact lens compared to no lens wear. Presentation at British Contact Lens Association Clinical Conference, June 2014.
- Szczotka-Flynn LB, Raghupathy S, Debanne S et al. Daily wear central corneal swelling with etafilcon A is non-inferior to two silicone hydrogel lens types. Optom Vis Sci 2015; 92.
- Chalmers RL, Hickson-Curran S, Keay L et al. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci 2015;56:654-663.
- Chalmers RL, Wagner H, Mitchell GL et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the contact lens assessment in youth (CLAY) study. Invest Ophthalmol Vis Sci 2011;52:6690-6696.
- Szczotka-Flynn L, Jiang Y, Raghupathy S et al. Corneal inflammatory events with daily silicone hydrogel lens wear. Optom Vis Sci 2014;91:3-12.
- Hickson-Curran SB, Chalmers RL, Keay L et al. Patient-reported wearing experience from hydrogel daily disposable wearers older than 40 years from TEMPO registry. Eye Contact Lens 2017;43:5 313-317.
- Diec J, Papas E, Naduvilath T et al. Combined effect of comfort and adverse events on contact lens performance. Optom Vis Sci 2013;90:7 674.
- Stapleton F, Naduvilath T, Keay L et al. Risk factors and causative organisms in microbial keratitis in daily disposable contact lens wear. PLoS ONE 2017;e0181343.
- Dart JKG, Radford CF, Minassian D et al. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology 2008;115:1647-1654.
