Refractive surgery is increasing in popularity and is expected to grow at a compound annual rate of 5.2% from 2017 to 2022, with annual procedure volume increasing from 3.6 million to 4.6 million.1 his includes a range of procedures from laser refractive surgery, presbyopia-correcting surgery, refractive lens exchange, and phakic intraocular lens (IOL) implantation.
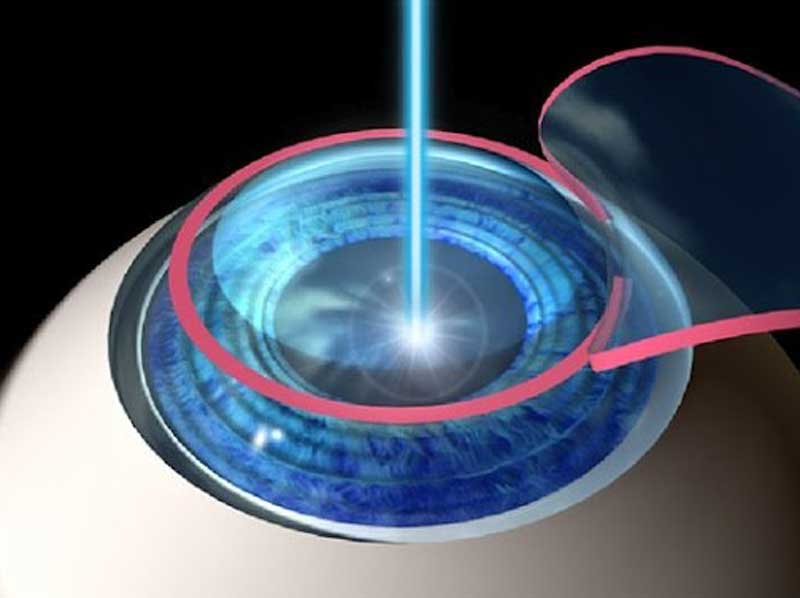
Figure 1: Flap elevation in LASIK procedure
The procedure of choice for each patient depends on their needs, expectations and clinical findings.
Laser vision correction (LVC) is one of the most popular elective surgical procedure, and it has been shown to provide a safe and effective treatment for refractive error. Laser vision correction involves laser removal of corneal stromal tissue and includes LASIK (laser assisted in situ keratomileusis – figure 1 and 2), LASEK (laser-assisted sub-epithelial keratectomy) and PRK (photorefractive keratectomy).
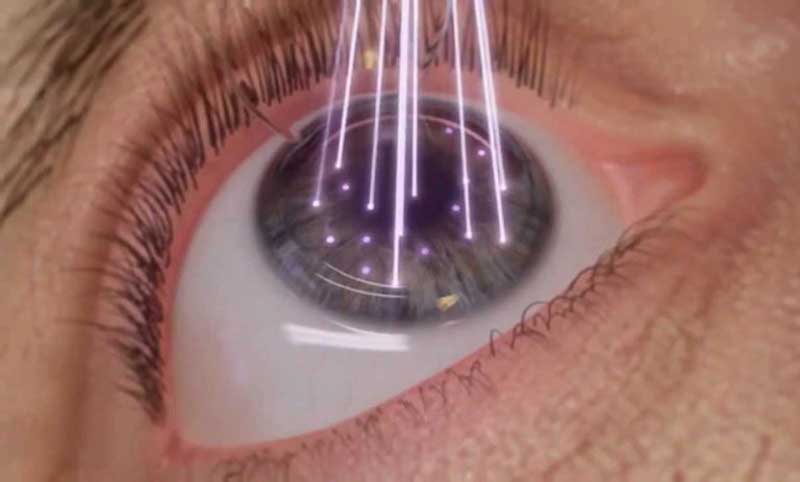
Figure 2: Stromal ablation in LASIK
The current National Institute for Health and Clinical Excellence (NICE) guidelines2 indicate that ‘Corneal reshaping is achieved in photorefractive surgery using excimer laser ablation and is indicated in the range of refractive error from +6 dioptres (DS) of hyperopia to –10 DS of myopia, with up to four cylinders of astigmatism.’
SMILE (small incision lenticule extraction) is another corneal refractive surgery where a femtosecond laser is used for the entire procedure to create a lenticule of stromal tissue, which is then removed via a small incision. As no flap is created, the benefits are a better post-operative corneal biomechanical strength, as well as potentially less long-term dry eye as the corneal nerve plexus is minimally disrupted. SMILE is currently indicated for the correction of myopia of up to -10.00DS with up to 5.00DC of astigmatism, or up to -12.50DS spherical equivalent.3
Implants
Refractive lens exchange (RLE) is a procedure whereby the natural crystalline lens is replaced with an IOL (figure 3). The IOL is calculated to correct the refractive error of the patient, with the aim to achieve emmetropia and therefore enabling freedom from spectacles.
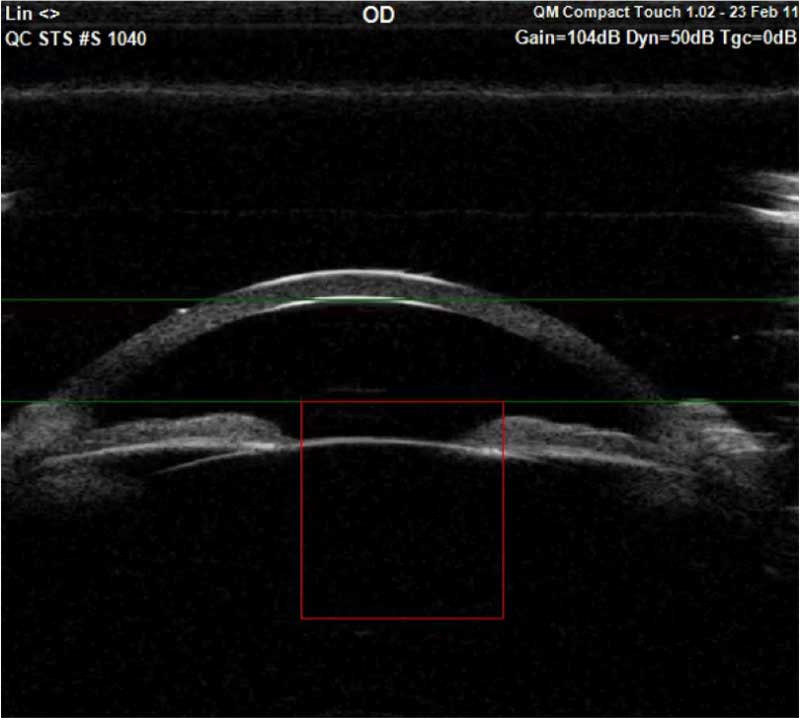
Figure 3: Anterior widefield OCT showing implantable contact lens in situ
However, RLE is normally reserved for patients that have reached presbyopia as the removal of the crystalline lens results in the loss of accommodation. Patients can choose to have a multifocal IOL (figure 4) to achieve spectacle independence at both distance and near.

Figure 4: Trifocal intraocular lens
Phakic intraocular lenses (pIOLs) were developed as an alternative to cornea-based refractive surgery procedures, as well as another option over refractive lens exchange (figure 5). This procedure involves the insertion of an IOL into the anterior or posterior chamber through a small corneal incision. These phakic lenses correct common refractive problems, such as myopia, hyperopia and astigmatism by functioning as a refractive element to optically reduce myopia, hyperopia, and astigmatism. The main advantage over laser vision correction is that larger refractive errors can be corrected with the choice of the correct IOL power. Phakic IOLs are also an alternative for patients unsuitable for laser vision correction, for example because of thin corneas, or dry eye. The main advantage of phakic IOLs over RLE is that the crystalline lens is untouched and therefore accommodation is preserved.
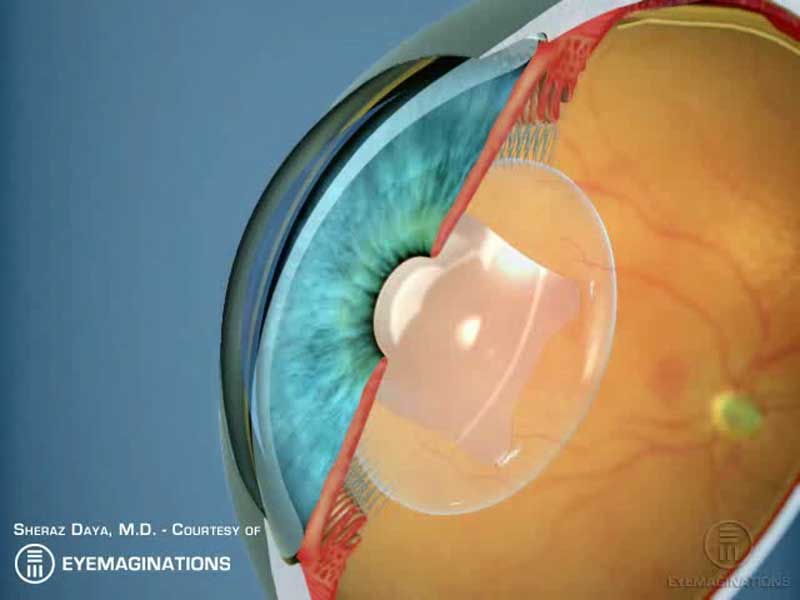
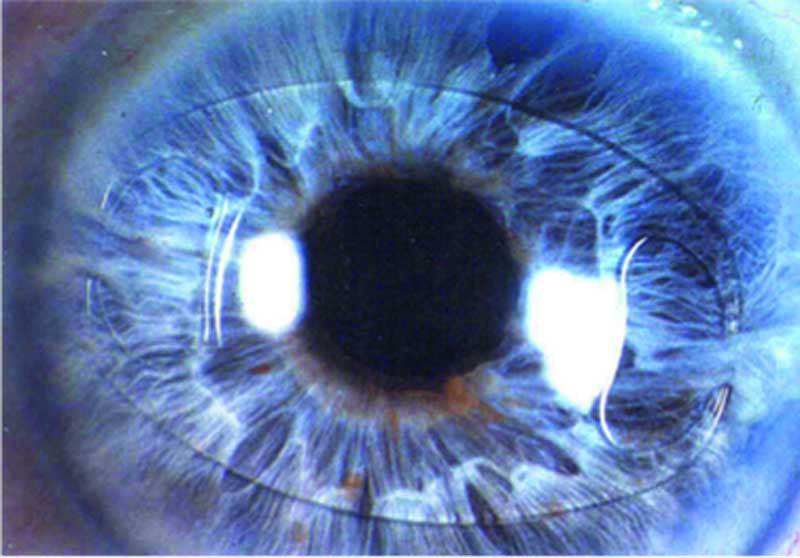
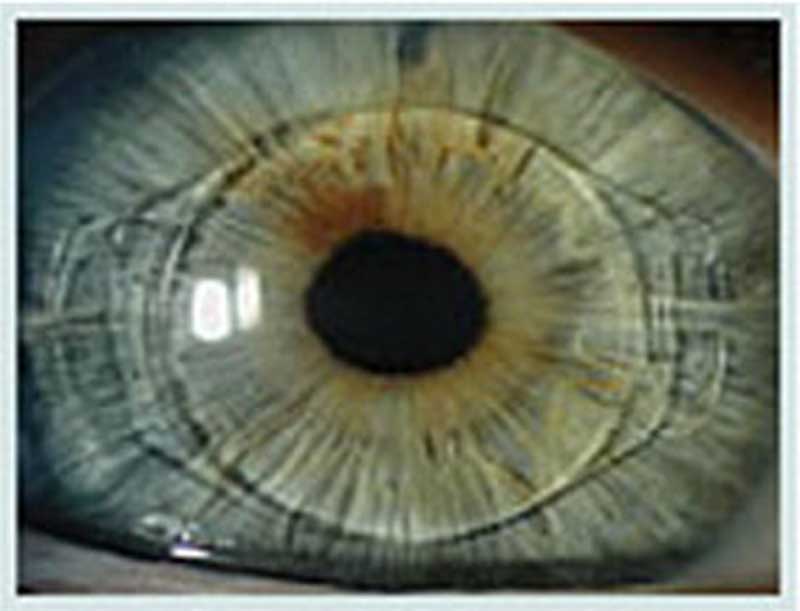
Figure 5: Phakic intraocular lens
Within this category of refractive treatments, there are two types of lenses: anterior chamber IOLs and posterior chamber lenses, which are typically described as implantable contact lenses (ICLs).
Anterior Chamber
Anterior chamber IOLs include iris-fixated lenses which are secured in the anterior chamber by two haptic claws, which clip on to the iris, and angle-supported lenses which rest in the iridocorneal angles (figures 6 a and b).
A
B
Figure 6: A and B. Two examples of anterior chamber intraocular lenses
Posterior Chamber
Posterior chamber lenses, such as the Visian ICL are placed between the iris and the natural lens or an intraocular lens in the capsular bag.
The most frequently implanted of these devices, the Visian ICL (Staar Surgical, Monrovia, CA), has been implanted in more than a million patients to date.4 The Visian ICL family of lenses include Visian ICL,Visian Toric ICL, + Visian ICL, and Visian Toric ICL.
For myopes, the ICLs are intended to correct/reduce low to high myopia (-0.50DS to -20.00DS), as well as the correction/reduction of myopia and astigmatism in patients with up to -20.00DS of myopia with less than or equal to 6.00DC of astigmatism. For hyperopic patients, correction of mild to severe hyperopia between +0.50DS and +10.00DS, is attainable, with up to 6D of astigmatism. Patients must have an anterior chamber depth (ACD) equal to or greater than 3.0mm, as measured from the corneal endothelium to the anterior lens capsule. All ICLs are intended to be placed entirely within the posterior chamber directly behind the iris and in front of the anterior capsule of the human crystalline lens.
The ICL can correct refractive errors that cannot be corrected with corneal laser refractive procedures and because the crystalline lens is untouched, so accommodation is preserved as opposed to refractive lens exchange procedures.
With more than 15 years of clinical use, there is a large body of scientific data that demonstrates the safety and effectiveness of the ICL, with low rates of adverse events reported.5,6
Implantable Performance
More than 100 peer review publications have evaluated the clinical results of the ICL, as well as the stability of these lenses and rates of post-operative infection. The studies also compare outcomes of the ICL with other refractive procedures, including wavefront-guided laser vision correction and other phakic IOLs. The papers included here are reflective of the data that has been reported.
For example, a 2015 retrospective review looked at long-term outcomes with the ICL. Moya, et al, reported on refractive results and any long-term complications in a group of 144 myopic eyes 12 years after implantation. Mean spherical equivalent refraction was -16.90 ±4.26 DS preoperatively and -1.77 ±1.93 DS 12 years postoperatively. The mean corrected distance visual acuity (CDVA) at the first and last visit were 0.31 ±0.19 logMAR and 0.22 ±0.22 logMAR, respectively. About 9% of the eyes had lost two or more lines of CDVA at the 12-year follow-up.7
Alfonso et al,8 looked at five-year follow up on 188 eyes and found that the mean spherical equivalent (SE) decreased from -11.17 ±3.40 DS preoperatively to -0.23 ±0.50 DS at one month postoperatively (95% confidence interval [CI] -0.15 to -0.02). At five years the mean SE was still close to zero (-0.88 ±0.72 DS (95% CI, -0.68 to 1.09)). Another study by Higueras-Esteban et al reported excellent efficacy of the ICL with almost all eyes (97%) achieving a post-operative refraction within 0.50 DS of the intended refraction.9
Interestingly, the US military has okayed the use of the ICL in fighter pilots who were not appropriate candidates for laser vision correction. Reporting on three-month results of 135 eyes of 69 pilots, the authors found that the mean preoperative spherical equivalent refraction was -6.00 ±1.92 DS (range: -2.63 to -11.50 DS). Three months postoperative, uncorrected distance visual acuity of 6/6 or better was found in 129/135 (96%) eyes and 91/135 (67%) were 6/4.5 or better. Manifest refraction and CDVA data were available for 128 eyes.10
Higueras-Esteban et al retrospectively compared intraocular pressure after implantation of the Visian Implantable Collamer Lens (Visian ICL; STAAR Surgical) V4c and V4b designs in 17 and 18 eyes, respectively, over a three-month period.11 The presence of a central 360-µm hole, the KS-Aquaport, differentiates the V4c from the V4b. The KS-Aquaport allows a more regular flow of aqueous humour, eliminating the need for a laser iridotomy or surgical iridectomy. There was no significant difference between pre-and postoperative IOP values. A significant benefit of the hole ICL is that a laser iridotomy or surgical iridectomy is not required in advance of ICL implantation.
Implantable versus other techniques
In comparisons that looked at the performance of the ICL vs other refractive procedures, a recent Cochrane review compared laser refractive surgery to pIOL implantation for the correction of moderate to high myopia.12 The review involved 228 eyes and found no significant difference in visual outcomes between either group with the majority of patients achieving 20/20 or better uncorrected visual acuity. However, the reviewers noted that: ‘Phakic IOL surgery was safer than excimer laser surgical correction for moderate to high myopia as it results in significantly less loss of best spectacle corrected visual acuity (BSCVA) at 12 months postoperatively. However, there was a low risk of developing early cataract with phakic IOLs. Phakic IOL surgery appeared to result in better contrast sensitivity than excimer laser correction for moderate to high myopia. Phakic IOL surgery also scored more highly on patient satisfaction/preference questionnaires.’12
In comparative studies vs anterior chamber phakic IOLs, one study looked at the performance of ICLs in comparison to the Veriflex IOL (J&J Vision, Santa Ana, CA) in patients with moderately high levels of myopia.
In this study of 24 patients, the eyes were randomised to receive the ICL in one eye and the Veriflex lens in the fellow eye. At six-months postoperative, the logMAR UDVA and CDVA improved significantly in both groups (P < .001), with no statistical difference between the UDVA and the CDVA between the two groups (P = .36). Postoperative deviation from target refraction was -0.06 ±0.41 DS in the ICL group and -0.07 ±0.49 D in the Veriflex group (P = .15). The main difference in outcomes was in the Veriflex group, which had a higher, but statistically insignificant central endothelial cell count loss occurred in the Veriflex group (P = .11).
Both ICL and Veriflex PIOLs have equally satisfactory objective and subjective visual outcomes after surgery.13
A Turkish study looked at the results in eyes implanted with the ICL and the Artiflex anterior chamber IOL in 60 eyes of 30 patients. In this study, 15 patients were implanted bilaterally with the ICL and 15 patients received the Artiflex bilaterally. Investigators reported that at one-year postoperative, ‘the mean UCVA (p=0.002) and BSCVA (p=0.0001) were significantly better in the ICL group than the Artiflex group. The mean IOP was significantly less in the ICL group than the Artiflex group (p=0.018). The mean ECD was significantly less in the Artiflex group than the ICL group (p=0.006). There was no significant difference in the mean SE between the ICL and Artiflex groups (p=0.809).’14
Various studies have demonstrated the safety, efficacy, predictability, and stability of ICL for the correction of low, moderate, and high levels of myopia.15,16 Visual recovery time is similar to LASIK, ~1–2 weeks.
Contra-indications and Possible Complications
As with any surgical procedures, not all patients are suitable. The main contra-indications are as follows:
- Small anterior chamber depth (<3.00mm)
- Narrow anterior chamber angle
- Decreased endothelial cell density
- Glaucoma and/or previous history of iritis
- Pigment dispersion syndrome
- Pseudoexfoliation
Conclusion
Phakic implantable contact lenses have been around for more than 15 years in Europe. These lenses have been shown to provide excellent visual outcomes, and low rates of complications. Their main advantages are that they can be used to treat higher levels of refractive error, compared to laser vision correction, as well as inducing less risk of dry eye and corneal complications. Another advantage is that the procedure is fully reversible with the possibility of removing the ICL.
- Kristine Morrill is co-founder, Medeuronet, London, UK. Marine Gobbé, MSTOptom, PhD, is a clinical scientist, Medeuronet, London, UK.
References
- Global Demand for Refractive Surgery to Grow 5.2 Percent over Next Five Years. MARKET SCOPE, DECEMBER 20, 2017. https://market-scope.com/pressrelease/global-demand-for-refractive-surgery-to-grow-5-2-percent-over-next-five-years
- Photorefractive (laser) surgery for the correction of refractive errors Interventional procedures guidance Published: 22 March 2006. NICE guidance https://www.nice.org.uk/guidance/ipg164
- https://www.zeiss.com/meditec/int/products/ophthalmology-optometry/cornea-refractive/laser-treatment/femtosecond-laser-solutions/relex-smile.html
- STAAR Surgical. Available at: https://uk.discovericl.com
- Saunders DR. Anterior subcapsular opacities and cataracts 5 years after surgery in the visian implantable Collamer lens FDA trial. J Refract Surg. 2008; 24(6):566-570.
- Packer, M. Visian ICL: A review of the Literature. Cataract & Refractive Surgery Today Europe. September 2016; pp.8-11.
- Moya T, Javaloy J, Montés-Micó R, Beltrán J, Muñoz G,Montalbán R.J Refract Surg. Implantable Collamer Lens for Myopia: Assessment 12 Years After Implantation. 2015 Aug;31(8):548-56.
- Alfonso JF, Baamonde B, Fernandez-Vega L, Fernandes P, Gonzalez-Meijome JM, Montes-Mico R. Posterior chamber collagen copolymer phakic intraocular lenses to correct myopia: five-year follow-up. J Cataract Refract Surg. 2011;37(5):873-880.
- Packer, M. Meta-analysis and review: effectiveness, safety, and central port design of the intraocular collamer lens. Clinical Ophthalmology 2016: 10 1059-1077.
- Parkhurst GD1, Psolka M, Kezirian GM. Phakic intraocular lens implantation in United States military warfighters: a retrospective analysis of early clinical outcomes of the Visian ICL. J Refract Surg.2011 Jul;27(7):473-81.
- Brinton JP, Comparison of Two ICLs. Cataract & Refractive Surgery Today Europe, June 2004. Available at:https://pdfs.semanticscholar.org/2b1e/f0f1e047eb5b79ff74daf168a2b5c0ce894a.pdf
- Schubert, M. Lasers or Lenses? The Ophthalmologist, Dec. 2014, Allan_ Mertens, available at www.theophthamologist.com.
- Awadein, Ahmed & Habib, Ahmed. (2013). ICL Versus Veriflex Phakic IOL for Treatment of Moderately High Myopia: Randomized Paired-Eye Comparison. Journal of refractive surgery (Thorofare, NJ: 1995). 29. 445-452. 10.3928/1081597X-20130617-02.
- Sayman Muslubas IB, Cabi C, Aydın Oral AY, Akcay L, Kaplan AT, et al. (2013) Comparison of Outcomes of Posterior Chamber and Iris-Claw Anterior Chamber Phakic Intraocular Lens Implantation for Moderate to High Myopia. J Clin Exp Ophthalmol 4: 263.
- Kamiya K, Shimizu K, Igarashi A, Hikita F, Komatsu M. Four-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Arch Ophthalmol. 2009;127(7):845–850.
- Sanders DR, Doney K, Poco M, ICL in Treatment of Myopia Study Group United States Food and Drug Administration clinical trial of the implantable collamer lens (ICL) for moderate to high myopia: three-year follow-up. Ophthalmology. 2004;111(9):1683–1692
