Once limited to office use, gaming or telecommunications, digital devices now truly encompass every part of our daily lives. Smartphones, desktop and laptop computers, tablets and e-readers, video games, and televisions are commonplace, and their accessibility has allowed almost everyone of any age to become a ‘user’. The use of these devices has transformed the way we live and work but our widespread dependence on these devices is highlighted by the fact that 90% of Americans use digital devices for more than two hours each day.1 What is more, market research recently re ported that nearly 30% of adults in the United States spend more than nine hours per day using a digital device.2
WHAT’S THE PROBLEM?
The use of digital devices is rapidly increasing, not only for adults, but also for children. For example, a survey conducted by the American Optometric Association (AOA) reported that 83% of children aged 10 to 17 use electronic devices for three or more hours each day.3 Digital devices are also becoming commonplace in education, where tablets and apps are developed for both teaching and learning.
Many individuals experience eye discomfort and vision problems when viewing a computer screen for extended periods of time, a phenomenon sometimes referred to as ‘computer vision syndrome’ (CVS) in the early days of widespread computer use. More recently, the term ‘digital eye strain’ (or ‘digital eye fatigue’), encompasses the symptoms arising from using a broader spectrum of digital devices.2,3
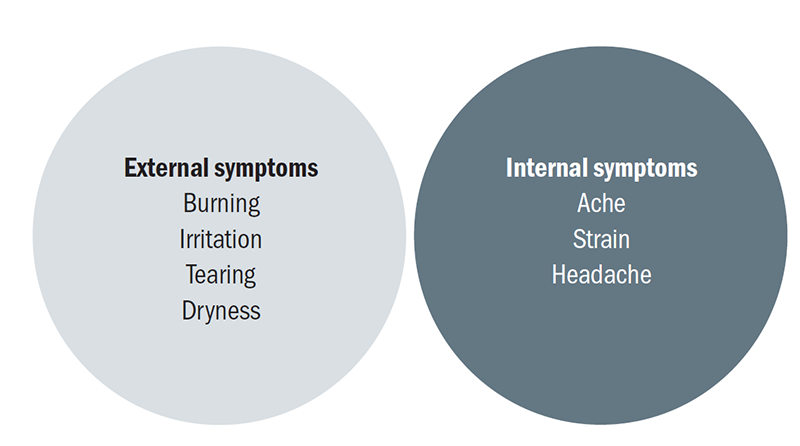
Figure 1: Classification of asthenopic symptoms based on their origin (based on Sheedy et al, 2003)
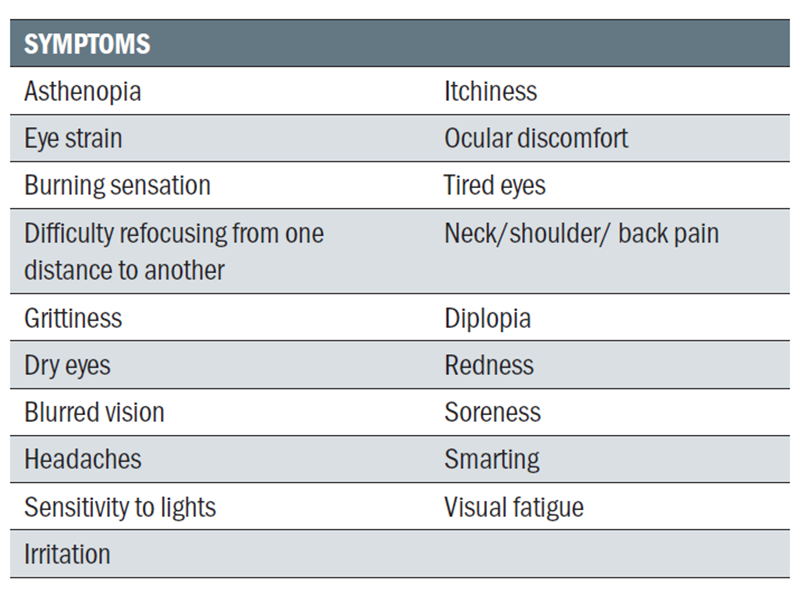
The list of CVS symptoms compiled by the AOA include eye strain, headaches, blurred vision, and dry eyes, as well as musculoskeletal symptoms (eg, neck and shoulder pain) that arise from poor ergonomics.4 Several publications have investigated the occurrence of increased symptomology when using digital devices for different tasks, including working, reading, and playing video games; however, significantly fewer studies have been conducted specifically exploring the effects of smartphones, tablets, and e-readers.
Table 1 2,5-7 provides a list of commonly reported symptoms associated with the use of different digital devices outlined in the literature.
Eye strain, or asthenopia, is a generic term which is associated with multiple conditions. An ‘asthenopia classification system’ was developed by Sheedy and co-authors, who proposed that symptoms of asthenopia in visually normal participants fell into two distinct categories: those associated with external factors and those associated with internal factors.7 Their categorisation of symptoms is shown in figure 1. External symptoms of asthenopia were related to sensations at the front and bottom of the eye, while internal symptoms of asthenopia were related to sensations that are felt in the head or behind the eyes. The authors concluded that external factors are consistent with dry eye symptoms, and internal factors may be related to accommodation and/or binocular vision issues.
Digital eye fatigue has also been described as ‘the physical discomfort of one’s eyes after spending periods of time throughout the day in front of a digital device, such as a computer or smartphone’.8 Under this definition, the three most commonly reported symptoms of eye fatigue were: dryness (95%), tiredness (92%), and sleepiness (82%).8
The extent to which these symptoms are due to the use of digital devices rather than the nature of the tasks being completed with the devices is currently unknown.
HOW BIG IS THE PROBLEM?
Surveys have found that 30% to 65% of office workers report symptoms related to ocular fatigue and dryness.1,9 What is more, in children, 80% reported similar symptoms after prolonged use of electronic devices,3 and the duration of use of these devices
has been associated with the prevalence of dry eye syndrome in children.10
Risk factors for visual discomfort include the amount of time spent using digital devices in the office environment,11-14 and it has been suggested that contact lens wearers are more likely to suffer symptoms of digital eye fatigue than non-contact lens wearers.12,13 Other proposed risk factors for dry eye symptoms among computer users include female gender,9,11,12,14 age,15 as well as meibomian gland dysfunction.16,17
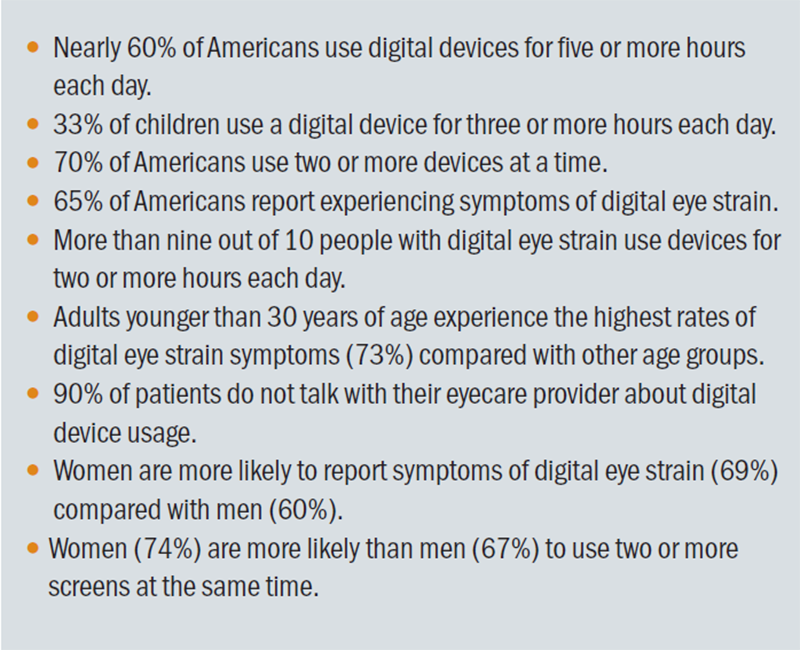
A report in 2016 from the Vision Council in the US revealed statistics about how much time Americans are spending in front of the screen and the results are outlined in table 2.
WHAT CONTRIBUTES TO THE PROBLEM?
Accommodation and vergence
Studies examining the effect of binocular vision and symptoms of digital device users in the past 30 years have reported mixed results. In the late 1980s and early 1990s, studies reported workers who used computer displays exhibited decreased ranges of accommodation and vergence throughout the course of the workweek compared with workers who did not use computer displays. This suggested a possible link between computer use and changes in binocular vision.18-20
However, later studies found no change, or only subtle links between accommodation, vergence and the subjective symptoms of asthenopia associated with the sustained use of digital devices. One study reported subjects with an exophoria tended to show fewer CVS symptoms than those with no phoria, suggesting that reduced vergence response may make the use of digital devices at closer distances more comfortable.21 A separate study also found that closer viewing distances (with greater accommodation and vergence demands) reduced subjective visual discomfort when using a computer screen.22 Therefore, accommodation and vergence do not appear to play a major role in the symptoms of asthenopia that have been associated with computer use. Nonetheless, digital device technology has moved beyond the typical computer. Smartphones and tablets utilise a different range of working distances than traditional near work,23 and although 77% of symptomatic digital device users use two or more devices simultaneously,1 very few studies have addressed the impact on symptoms of repeatedly switching fixation between digital devices positioned at different working distances. Therefore, multitasking at varying distances should be considered and addressed by eye care practitioners (ECPs) during eye examinations.
Table 1: Summary of reported symptoms associated with using digital devices2,5-7
Cognitive fatigue
Current evidence does not indicate an important role for cognitive load or cognitive fatigue in the development of ocular fatigue when using digital devices. The cognitive effort required to read text on a liquid crystal display (LCD) tablet and an e-reader does not differ from reading hard-copy text.24 Furthermore, varying cognitive load was not found to influence symptoms of asthenopia while reading text from a computer monitor.25 However, more cognitively demanding tasks accentuated the effects of other visual stressors, such as low contrast text or induced optical defocus, on subjective reports of asthenopia.26 This suggests that cognitive load may exacerbate the effects of pre-existing visual disorders, such as uncorrected refractive error or mild binocular vision disorders, on visual discomfort while using computer displays.
Table 2: Key statistics about US screen usage (adapted from the Vision Council. Eyes Overexposed: The Digital Device Dilemma; 2016 Digital Eye Strain Report; 2016.)
How bright is that light?
Portable digital devices with shorter viewing distances23 have higher luminance levels than computer screens;27 however, these are still significantly lower that the luminance levels experienced in an outside environment (daylight). These luminance levels do not appear to influence the symptoms of ocular fatigue from prolonged periods of reading on e-readers or backlit LCD tablets.28,29 However, there is strong evidence to support that reflections and glare, which degrade the image quality on digital devices, can cause users to squint or partially close their eyes to reduce the visual discomfort.30 In fact, this was a common complaint about the older cathode ray tube monitors, where the shiny, convex, glass surface typically resulted in a greater proportion of specular reflection. However, even the matte surfaces of modern LCD screens can result in diffuse reflections.31 Evidence supporting the notion that glare plays a role in asthenopia from digital device use comes from studies investigating the use of plastic screen filters with anti-reflective coatings applied to reduce glare. These filters and coatings have been applied to handheld gaming devices, and, as a result, it appears that patients have benefited from an increased blink rate and experienced a reduction in asthenopic symptoms.32,33
Blinking and dry eye symptoms
Blinking is a vital aspect of ocular surface health and tear film maintenance. Suboptimal blink patterns pose a major risk factor for developing signs and symptoms associated with dry eye syndrome. Full, normal blinking spreads tears across the ocular surface, expresses and spreads lipids secreted by the meibomian glands across the ocular surface, minimises tear evaporation, and prevents ocular surface desiccation. It is well established that blink rates are reduced during concentrated computer screen use,5,6,34 and the findings are similar for handheld video games.32,35 A study conducted by Benedetto et al found that blinking is reduced for all reading tasks, irrespective of the platform; however, reading on backlit LCD screens resulted in significantly fewer blinks and appeared to result in greater levels of ocular fatigue.36
Incomplete blinks are considered a greater contributing factor to tear instability than reduced frequency of blinks.37 In addition, the completeness of blinks also has an impact on the likelihood of developing corneal desiccation and contact lens surface dryness.34,38 Even when the same reading task is provided and conditions, such as luminance, font size, and contrast, are controlled, blink completeness is significantly reduced when reading from a desktop LCD screen compared with hard-copy print.
Interestingly, increasing the size of text has been found to increase blink frequency but reduce blink completeness.39 Non-maintenance of the tear film due to poor blinking can cause areas of poor wetting on the ocular surface, leading to asthenopia and causing a reduction in visual acuity.40 Part of the eye fatigue experienced by users of digital devices may arise from dryness symptoms.8,13 This includes blurred vision which may be a secondary effect of the inadequate spreading of tears rather than a result of uncorrected refractive error or inaccurate accommodation.
THE CHALLENGES OF THE 21ST CENTURY OFFICE
Using digital devices affects our posture and, if maintained for extended periods of time, can lead to undesired musculoskeletal symptoms. The 2016 Vision Council report on digital eye strain1 found that 36% of Americans reported symptoms of neck/shoulder/back pain arising from digital device use, which increased by 3% from 2015 (see table 2).2 Although a smartphone, tablet, laptop, and a desktop computer all have the capability to send an email, the postures adopted to perform this task differs for each device.
Commonly, the head is tilted forward and down when using a handheld device, which places excess strain on the upper musculoskeletal system, which can lead to symptoms of neck, shoulder and/or back pain.41 Appropriate, ergonomic workstation setup and taking regular breaks from prolonged device use are imperative for minimising the likelihood of musculoskeletal problems.
Another challenge is eye dryness. Dryness is a commonly reported symptom among individuals who identify with digital eye fatigue.8,13 Adverse environments, such as those with low humidity, air conditioning or forced-air heating, are likely to cause corneal desiccation.5,6 Many of the studies that have addressed symptoms of computer users have been conducted in an office environment, where the environment is not readily controllable.9,42
For example, low humidity, in combination with the reduced blink rates associated with digital device use can increase tear evaporation and symptomology significantly.43 As a result, it can be difficult to determine from many studies whether the dryness symptoms are masquerading as asthenopia. Distinguishing digital eye fatigue from binocular vision/accommodation issues and ocular dryness is important, though challenging.
OFFERING RELIEF FOR THE OCULAR SURFACE
Dry eye symptoms, such as soreness, itching, and irritation, are commonly reported by patients in clinical practice, and the use of digital devices might exacerbate the frequency or severity of these symptoms. Efforts to increase blink frequency have been attempted in several studies, using visual44 or auditory cues.45 Although the theory of increasing blinks may seem valid, there is no evidence demonstrating any long-term effects and benefits.
Again, a patient’s environment can affect the ocular surface. ECPs should discuss the option of using humidifiers to increase humidity in the immediate environment, as this may be beneficial in reducing tear evaporation and symptoms of dryness.46 Specifically, increasing humidity can help to reduce tear evaporation, increase tear lipid layer thickness, and improve tear stability, which, in turn, improves ocular comfort.43 A portable, desk-sized humidifier can be easily implemented in the work and home environment. Another option is to employ the use of artificial tears. Using artificial tears or eye drops provides immediate relief of dry eye symptoms related to digital device use.47,48 With the wealth of eye drops available, ECPs should consider the individual needs of the patient before recommending a product and be ready to give advice on the frequency and technique of instillation.
MANAGING THE CONTACT LENS WEARER
In the same way that a full refractive assessment is conducted for spectacle wearers, the same consideration is required for the contact lens wearer. Identifying any uncorrected astigmatism and prescribing toric lenses is one way to reduce symptoms of digital eye fatigue by improving visual acuity.6
From an accommodative perspective, educating patients on accommodative changes before presbyopia sets in plays a key role in managing their expectations for a change in contact lens design. Managing the refractive demands in early presbyopic contact lens wearers is crucial to reduce symptoms of eye fatigue and to minimise contact lens dropout. Early symptomatic presbyopes subjectively prefer low addition multifocal contact lenses to other methods of presbyopic correction (such as monovision), and multifocals consistently offer improved ‘real life’ performance.49 For pre-presbyopes, future contact lens designs utilising a unique optical profile may be beneficial in providing ‘fatigue relief for lens wearers suffering from digital eye fatigue’.8
Contact lens discomfort is the most frequently cited reason for discontinuation of lens wear.50 In a survey examining the impact of digital devices on contact lens wearers, up to 74% of contact lens wearers reported removing their lenses when discomfort was experienced.51 The greater rate of dehydration of some high-water-content lenses may be associated with greater levels of discomfort; however, other properties, such as lens material, modulus, and co-efficient of friction, also have an impact on comfort levels.52
Although the management of contact lens discomfort is beyond the scope of this article, evaluation of the care regimen for reusable lens wearers should be considered. One study reported a significant reduction in symptoms of dryness and lower blink rates (suggesting less irritation) in reusable contact lens wearers when using lens care solutions incorporated with wetting agents compared with solutions without these agents.53 Alternatively, the pro-active practitioner may consider a change in lens material or a switch to a more frequent lens replacement modality to reduce the likelihood of discomfort from ineffective lens cleaning or poor surface wettability.
Pall and co-authors reported that 70% of reusable contact lens wearers who experience dryness while using digital devices use rewetting drops for dryness.51 Contact lens wearers can also be reassured that immediate relief from symptoms while using digital devices can be obtained with the use of eye drops,54 particularly in challenging environments (low humidity, high temperature) where dryness and symptoms of ocular fatigue may be exacerbated.12,14
The relief gained from drops may only be temporary, and ECPs should be prepared to find alternative ways to mitigate symptoms of contact lens discomfort if the drops prove to be ineffective long term.
SOLVING THE PROBLEM OF FATIGUE
As discussed, the origins of ocular fatigue while using digital devices are multifactorial. The Vision Council’s report on digital eye strain found that 90% of patients do not talk to their eye care professional about the ocular discomfort they experience with digital device use.1
Practitioners can reinforce the importance of taking regular breaks and encourage patients to adopt the 20-20-20 rule, which recommends that a digital device user take a 20-second break from the screen every 20 minutes by looking at something 20 feet away.
Initiating the conversation with patients is important to be able to address their needs and concerns regarding digital device use. Discussing patients’ ergonomics (or lack thereof) will also enable practitioners to offer better advice and solutions.
People across all generations reporting being affected by digital eye fatigue. As many as 73% of adults in their 20s and 53% of adults aged 60 and older report such symptoms.1 Correcting the refractive error and managing any underlying binocular vision anomalies is important in providing patients with best corrected visual acuity and optimal viewing comfort. For example, correcting residual astigmatic error increases productivity (determined by accuracy and time taken to complete tasks) by 3% to 29%, and also improves visual comfort.55
MOVING BEYOND THE BASICS: SPECTACLE LENS OPTIONS
To match the visual needs for each age group, several spectacle lens manufacturers offer their own optimised lenses designed to help reduce the symptoms associated with digital eye fatigue.
Such solutions include anti-fatigue lenses for the pre- or emerging presbyopic, ametropic, and emmetropic patients that provide accommodative support up to +0.80D in the near zone at the bottom of the lens.56 Fitted as enhanced single vision lenses, at the end of a four-week trial, 76 masked ametropic subjects aged 20 to 55 who were dispensed with these anti-fatigue lenses indicated good acceptance, reduced symptoms of tired eyes, and less difficulty with small characters compared with their previous single vision lenses.57
For established presbyopes, room-distance lenses and high-performance PALs (progressive addition lenses) are able to meet the demands of this subset of digital device users. These PALs can be divided into three categories: restricted distance-vision lenses, office lenses that correct vision from near to up to five metres, and occupational lenses that correct for intermediate/near vision only. These lenses may offer improved ergonomics due to their wider area of transition from distance vision (in the upper portion of the lens), to near vision (at the lower portion of the lens), with an emphasis on maximising vision for the intermediate-to-near working distances.
A wide range of clear viewing distances is becoming increasingly important with the need for greater interaction with other people and tasks conducted in the working area. ‘Room distance’ PALs may be of particular benefit for digital device multitaskers or in the home environment, where a user’s attention may be divided between two viewing distances (eg alternating between viewing a tablet and watching a television screen). However, patients who are dispensed with any occupational PALS, including ‘room distance’ PALs, may find these options less convenient, as they are not suitable for driving.58
MOVING BEYOND THE BASICS: CONTACT LENS OPTIONS
Patients are subjecting their eyes and vision to demanding tasks in challenging environments. ECPs have reported success with spectacle anti-fatigue lenses for a range of patients, including first-time, moderate hyperopes, over-minused myopes, pre- and emerging presbyopes, and frequent digital device users.59 The spectacle lens industry has identified the need to solve digital eye fatigue and has designed many options for digital device users. However, to date, the evidence that such adapted lenses will reduce digital eye fatigue is weak, and further studies to support this concept are needed.
Nevertheless, perhaps the contact lens wearer is left neglected in this specialised area of optical management of digital eye strain, as such options do not exist in the contact lens world. Innovative products developed by the contact lens industry are required to maintain our patients’ need for visual and physiological comfort, to meet the high demands of this digital device era. The contact lens market is dominated by pre-presbyopic digital device users, of which a considerable proportion are symptomatic.13,51 Contact lenses with an adapted optical profile might be useful to relieve accommodative fatigue in a similar way for pre- or emerging presbyopes.8
IMPROVING THE PATIENT-PRACTITIONER RELATIONSHIP
As the rapid development of digital technology increases, so, too, will the use of digital devices. This means that the number of patients experiencing (and requiring relief from) digital eyestrain symptoms are likely to increase as well. Practitioners who recognize this growing need and choose to embrace and offer innovative products and services to their patients will be better poised to improve their patient-practitioner relationship and retention rates.
ACKNOWLEDGEMENTS
This article is based on material first published in Contact Lens Spectrum and was supported by Coopervision.
Professor Lyndon Jones is based at the School of Optometry & Vision Science, and University Research Chair and Director, Centre for Contact Lens Research, University of Waterloo, Canada where Dr Alison Ng is a Post-Doctoral Fellow and Benjamin Thomson is Associate Professor.
REFERENCES
- The Vision Council. Eyes Overexposed: The digital device dilemma; 2016 Digital Eye Strain Report. 2016.
- The Vision Council. Hindsight is 20/20/20; 2015 Digital Eye Strain Report. 2015.
- American Optometric Association. Survey reveals parents drastically underestimate the time kids spend on electronic devices. 2014 [Accessed 15/10/2014]; Available: www.aoa.org/newsroom/survey-reveals-parents-drastically-underestimate-the-time-kids-spend-on-electronic-devices?sso=y
- American Optometric Association. Computer Vision Syndrome. 2014 [Accessed 06/11/2014]; Available: http://www.aoa.org/patients-and-public/caring-for-your-vision/protecting-your-vi- sion/computer-vision-syndrome.
- Blehm C, Vishnu S, Khattak A, et al. Computer vision syndrome: a review. Surv Ophthalmol. 2005;50(3):253-262.
- Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt. 2011;31(5):502-515.
- Sheedy JE, Hayes JN, Engle J. Is all asthenopia the same? Optom Vis Sci. 2003;80(11):732-739.
- Orsborn G, Vega J, Chamberlain P. Assessment of a new lens design to improve the symptoms of eye fatigue in users of digital devices. Global Specialty Lens Symposium; January 21- 24, 2016, Las Vegas.
- Portello JK, Rosenfield M, Bababekova Y, et al. Computer- related visual symptoms in office workers. Ophthalmic Physiol Opt. 2012;32(5):375-382.
- Moon JH, Lee MY, Moon NJ. Association between video display terminal use and dry eye disease in school children. J Pediatr Ophthalmol Strabismus. 2014;51(2):87-92.
- Uchino M, Schaumberg DA, Dogru M, et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology. 2008;115(11):1982-1988.
- Tauste A, Ronda E, Molina MJ, et al. Effect of contact lens use on Computer Vision Syndrome. Ophthalmic Physiol Opt. 2016;36(2):112-119.
- Meyer D, Huenink S, Rickert M, et al. Symptoms associated with eye fatigue in soft contact lens wearers. American Academy of Optometry; October 7-10, 2015, New Orleans.
- Gonzalez-Meijome JM, Parafita MA, Yebra-Pimentel E, et al. Symptoms in a population of contact lens and noncontact lens wearers under different environmental conditions. Optom Vis Sci. 2007;84(4):296-302.
- Uchino M, Yokoi N, Uchino Y, et al. Prevalence of dry eye dis- ease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol. 2013;156(4):759-766.
- Fenga C, Aragona P, Cacciola A, et al. Meibomian gland dysfunction and ocular discomfort in video display terminal workers. Eye (Lond). 2008;22(1):91-95.
- Wu H, Wang Y, Dong N, et al. Meibomian gland dysfunction determines the severity of the dry eye conditions in visual display terminal workers. PLoS One. 2014;9(8):e105575.
- Nyman KG, Knave BG & Voss M. Work with video display terminals among office employees. IV. Refraction, accommodation, convergence and binocular vision. Scand J Work Environ Health. 1985;11(6):483-487.
- Yeow PT, Taylor SP. Effects of short-term VDT usage on visual functions. Optom Vis Sci. 1989;66(7):459-466.
- Yeow PT, Taylor SP. Effects of long-term visual display terminal usage on visual functions. Optom Vis Sci. 1991;68(12):930-941.
- Collier JD, Rosenfield M. Accommodation and convergence during sustained computer work. Optometry. 2011;82(7): 434-440.
- Rempel D, Willms K, Anshel J, et al. The effects of visual dis- play distance on eye accommodation, head posture, and vision and neck symptoms. Human factors. 2007;49(5):830-838.
- Bababekova Y, Rosenfield M, Hue JE, et al. Font size and viewing distance of handheld smart phones. Optom Vis Sci. 2011 Jul;88(7):795-797.
- Kretzschmar F, Pleimling D, Hosemann J, et al. Subjective impressions do not mirror online reading effort: concurrent EEG-eye tracking evidence from the reading of books and digital media. PLoS One. 2013;8(2):e56178.
- Nahar NK, Gowrisankaran S, Hayes JR, et al. Interactions of visual and cognitive stress. Optometry. 2011;82(11):689-696.
- Gowrisankaran S, Nahar NK, Hayes JR, et al. Asthenopia and blink rate under visual and cognitive loads. Optom Vis Sci. 2012;89(1):97-104.
- Tahir HJ, Murray IJ, Parry NR, et al. Optimisation and assessment of three modern touch screen tablet computers for clinical vision testing. PLoS One. 2014;9(4):e95074.
- Shen IH, Shieh K-K, Chao C-Y, et al. Lighting, font style, and polarity on visual performance and visual fatigue with electronic paper displays. Displays. 2009;30(2):53-58.
- Siegenthaler E, Bochud Y, Bergamin P, et al. Reading on LCD vs e-Ink displays: effects on fatigue and visual strain. Ophthalmic Physiol Opt. 2012;32(5):367-374.
- Thorud HM, Helland M, Aarås A, et al. Eye-related pain induced by visually demanding computer work. Optom Vis Sci. 2012;89(4):452-464.
- Sheedy JE and Shaw-McMinn PG. Reflections from the computer display. Diagnosing and treating computer-related vision problems. Amsterdam, Boston: Butterworth-Heinemann, 2003; 143-155.
- Tsubota K, Miyake M, Matsumoto Y, et al. Visual protective sheet can increase blink rate while playing a hand-held video game. Am J Ophthalmol. 2002;133(5):704-705.
- Miyake-Kashima M, Dogru M, Nojima T, et al. The effect of antireflection film use on blink rate and asthenopic symptoms during visual display terminal work. Cornea. 2005;24(5):567-70.
- Cardona G, García C, Serés C, et al. Blink rate, blink amplitude, and tear film integrity during dynamic visual display terminal tasks. Curr Eye Res. 2011;36(3):190-197.
- Jansen ME, Begley CG, Himebaugh NH, et al. Effect of contact lens wear and a near task on tear film break-up. Optom Vis Sci. 2010;87(5):350-357.
- Benedetto S, Drai-Zerbib V, Pedrotti M, et al. E-readers and visual fatigue. PLoS One. 2013;8(12):e83676.
- Hirota M, Uozato H, Kawamorita T, et al. Effect of incomplete blinking on tear film stability. Optom Vis Sci. 2013;90(7): 650-657.
- McMonnies CW. Incomplete blinking: exposure keratopathy, lid wiper epitheliopathy, dry eye, refractive surgery, and dry contact lenses. Cont Lens Anterior Eye. 2007;30(1):37-51.
- Argiles M, Cardona G, Perez-Cabre E, et al. Blink rate and incomplete blinks in six different controlled hard-copy and electronic reading conditions. Invest Ophthalmol Vis Sci. 015;56(11):6679-6685.
- Goto E, Yagi Y, Matsumoto Y, et al. Impaired function- al visual acuity of dry eye patients. Am J Ophthalmol. 2002;133(2):181-6.
- Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014;25:277-9.
- Wolkoff P, Nojgaard JK, Troiano P, et al. Eye complaints in the office environment: precorneal tear film integrity influenced by eye blinking efficiency. Occup Environ Med. 2005;62(1):4-12.
- Abusharha AA, Pearce EI. The effect of low humidity on the human tear film. Cornea. 2013;32(4):429-434.
- Nosch DS, Foppa C, Toth M, et al. Blink animation software to improve blinking and dry eye symptoms. Optom Vis Sci. 2015;92(9):310-315.
- Portello JK, Rosenfield M. Effect of blink rate on Computer Vision Syndrome. Invest Ophthalmol Vis Sci. 2010;51(5):950.
- Tsubota K. Tear dynamics and dry eye. Prog Retin Eye Res. 1998;17(4):565-596.
- Acosta MC, Gallar J, Belmonte C. The influence of eye solu- tions on blinking and ocular comfort at rest and during work at video display terminals. Exp Eye Res. 1999;68(6):663-669.
- Skilling FC, Jr., Weaver TA, Kato KP, et al. Effects of two eye drop products on computer users with subjective ocular discomfort. Optometry. 2005;76(1):47-54.
- Woods J, Woods CA, Fonn D. Early symptomatic presbyopes— what correction modality works best? Eye Contact Lens. 2009;35(5):221-6.
- Nichols JJ, Jones L, Nelson D, et al. The TFOS International Workshop on Contact Lens Discomfort: Introduction. Invest Ophthalmol Vis Sci. 2013;54(11).
- Pall B, Wales M, Roussopoulou E. Eye care professional and contact lens wearer perspectives on digital screen devices. Optom Vis Sci. 2014;91: e145197.
- Jones L, Brennan NA, González-Méijome J, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):37-70.
- Yang SN, Tai YC, Sheedy JE, et al. Comparative effect of lens care solutions on blink rate, ocular discomfort and visual performance. Ophthalmic Physiol Opt. 2012;32(5):412-420.
- Guillon M, Maissa C, Pouliquen P, et al. Effect of povidone 2% preservative-free eyedrops on contact lens wearers with computer visual syndrome: pilot study. Eye Contact Lens. 2004;30(1):34-39.
- Daum KM, Clore KA, Simms SS, et al. Productivity asso- ciated with visual status of computer users. Optometry. 2004;75(1):33-47.
- Santini B. Going mobile. 20/20 Magazine. 2013;40(1):56-62.
- de Larrard B. The new range of Eyezen lenses: what are the benefits perceived by wearers during screen use? Points de Vue - International Review of Ophthalmic Optics. 2015;N72.
- Hughes E. Occupational dispensing: Dispense with Confidence Part 3. Optometry Today. 2012;52(20):25-29.
- Coronis T. Anti-fatigue lenses: RX for overworked eyes. 20/20 Magazine. 2010;37(7):72-76.
