Dispensing well-fitting, appropriate spectacles is of the utmost importance for the development of eyesight. A poorly fitting pair of glasses can cause discomfort, permanent visual harm or even disfigurement.1

According to the Opticians Act (1989), the dispensing of glasses to children (ie those under the age of 16) can only be carried out by, or under the supervision of, fully qualified optometrists and dispensing opticians. The reason for this restrictive supply is that paediatric dispensing requires a different approach and more specialist skills. Any errors in dispensing will have a more profound effect than in adults and children are not always able to communicate if something is uncomfortable or impacting on their vision.
This article will look at some of the key points of dispensing spectacles to children in order to give the best possible fit, cosmetic appearance and visual outcome. There are also some examples of conditions which require a more specialist fitting.
Frame selection
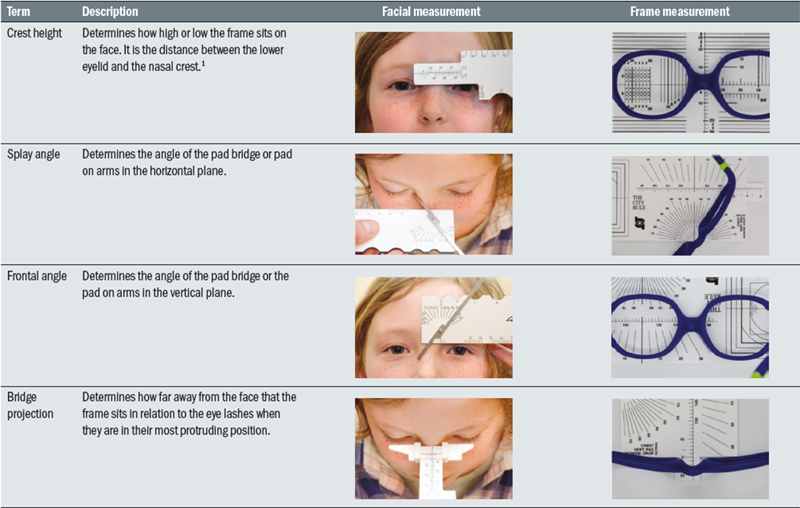
A child’s face is not just a scaled down version of an adult’s face. There are a number of anatomical differences which should be reflected in the choice of frame. The main differences are:2
- Reduced crest height
- Larger frontal angle
- Widened splay angle
- Smaller bridge projection
- Smaller head and temple width
- Less pantoscopic tilt
These facial measurements and the corresponding frame measurements are shown in figure 1.
Figure 1: Frame and facial measurements

The following need to be considered:
Smaller crest height
Children live in a world designed and made by adults and consequently spend a lot of time looking up.1 A frame with a small crest height will help by sitting the frame higher on the face. A profile that follows the line of the eye socket will also help to ensure the child is looking through rather than over their glasses. Ideally, the child’s pupils should sit on, or just above the horizontal centre line (HCL) and just inside of the vertical centre line.3 It is not acceptable for a child to be using only the top 10 to 20% of the lens.
Bridge shape
As a result of the undeveloped nasal bridge, children often have larger frontal and splay angles. A frame must be chosen with a large enough bridge and a frontal and splay angle that matches that of the child’s. The undeveloped nasal bridge may also give children a negative bridge projection or a bridge projection of zero (sometimes known as an inset bridge: Figure 1). This will reduce the back vertex distance (BVD) and consequently may cause the eyelashes to rub on the back of the lenses. A frame with a negative bridge projection will sit the frame away from the face and prevent this from happening. A rough idea of bridge projection can be gained easily by viewing the patient in profile and observing if the eyelashes or the bridge protrude the furthest. Figure 2 shows a patient with a positive bridge projection, where the bridge extends beyond the eyelashes.
Temple/headwidth
Ridges on the side of the patient’s head when the glasses are removed is a sign that the frame is fitting poorly and is probably uncomfortable. Furthermore, if the temple or head width of the glasses is too small, the mechanical effect will be that the glasses will slip and the patient may peer over the top of the frame. The frame should be no wider than the widest part of the face.4 If it is too wide, it will continually slip down the patient’s nose and the glasses will have to be unnecessarily tight behind the ears to compensate for this.
Infants and young children may have a small pupil distance (PD) but require a larger head width. By increasing angle of let back and putting a gentle bow in the sides it will ensure there is no pressure on the temples.
As with adult dispenses, choose a frame with a boxed centre distance similar to the patient’s PD. This will reduce the amount of decentration required when glazing and consequently reduce edge thickness, giving a lighter, more comfortable pair of glasses with the best cosmesis.
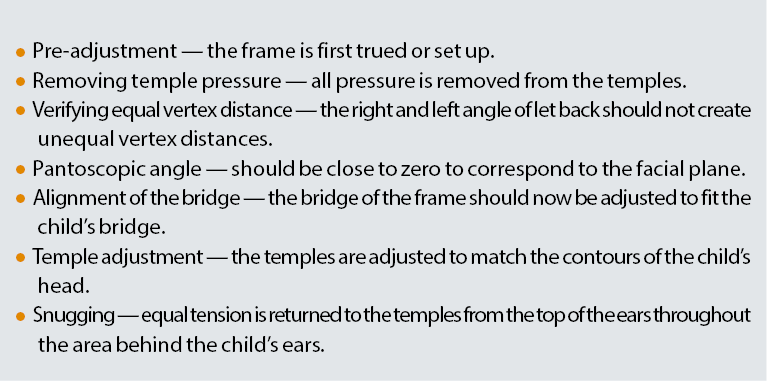
Table 1: Steps to dispensing a paediatric frame1
Pantoscopic angle
An adult frame normally has a pantoscopic angle of between 8º and 12º.5 Children’s frames should have a pantoscopic angle of around zero degrees to prevent them resting on the cheeks1 and causing ridges. Sometimes adding a little pantoscopic tilt may help prevent the lashes from rubbing on the back of the lenses.
There is not one style of frame that will work for all children, so it is important to have a selection of different styles available to try.
The facial anthropometry will change as a patient grows and their facial structure develops. Crest height and bridge projection will increase while splay angle and frontal angle will decrease. By the age of 13 the measurements will generally match those of an adult, although head width and length to bend will continue to increase after this.1 Table 1 summarises some steps to dispensing a paediatric frame.
Frame Material
The ideal child’s frame should be lightweight, flexible and hypoallergenic.6 A frame needs to be robust enough to withstand a child’s active lifestyle. Centrostyle and Miraflex frames are made from specialist plastics that are lightweight and strong, and take into account a child’s developing facial features. Generally, a frame made from one piece of plastic with no metal parts or hinges is most suitable for babies and will reduce the risk of facial trauma from the glasses.
Side Styles
Broadly speaking, there are three types of side styles that can be used on children’s frames:
Figure 2: A patient with a positive bridge projection, where the bridge extends beyond the eyelashes

Drop ends (or hockey ends)
The sides supplied on a frame are frequently too long and require adjustment. The length to bend (LTB) is the distance from the dowel point to the ear point and should be measured carefully. If it is too far forwards, it will cause the side to lift upwards, rub the back of the ear and put a tilt on the front of the frame. Too far back, and the angle of the drop will have to be very steep which will irritate the back of the ear and cause the glasses to slip down. The length of the drop for a child should be around 30mm with the angle of bend approximately 45º. Sides should be cropped if they are longer than 35mm. This is straightforward for both metal and plastic frames.
Figure 3: A well-fitting curl side

For plastic frames, the metal reinforcement will finish approximately 7mm before the tip of the side. The end can therefore be cropped up to this point, filed to an even finish and buffed. Immersing the end tip in acetone for a few seconds will also produce a shiny finish. Alternatively, if the sides need to be cropped beyond the metal reinforcement, companies such as Spec Care (UK) are able to cut the side at the joint and re-sink at the half joint. The inward angle of the drop should allow the drop to rest flush against the head without any pressure to the mastoid bone.
To shorten metal frames, the sides should be straightened and the plastic end tip removed. The metal side and end tip can then be cropped by the required amount and filed to remove any sharpness. After the end tip is replaced, the side can be adjusted to give the correct length to bend.
Centrostyle supply straps that can be fitted onto drop ends to hold the glasses in place. They are made from silicone and can easily be fitted onto the ends of most pairs of glasses.
Figure 4: Loop ends on a metal frame with a Bitterwell strap

Curl sides
Curl sides should fit perfectly to avoid damaging the cartilage at the back of the ear. Poorly fitting curl sides can pull on the ear and deform it.7 The curl side should follow the contour of the back of the ear, be flush against the side of the head and finish just before the ear lobe.7 Silicone covering on the curl sides makes them softer and more comfortable to wear. An example of a well-fitting curl side can be seen in figure 3.
Measure the length to tangent and total length of the side. The length to tangent is the distance from the dowel point to a tangent at the back of the ear (ie the apex of the curl) and the side length is the distance from the dowel point to the tip of the side when straight. Side length can be measured easily on a patient using a length of string to follow the position of the side.
Loop ends
Both plastic and metal frames can be converted to loop ends (see figure 4) and these should be positioned around 10mm past the ear point. A strap can then be fitted to help hold the glasses in place.
Spectacle straps tend to sit at the base of the head owing to the curved shape of the skull. Children have very soft ear cartilage so caution is needed as the straps can cause the ears to be pulled downwards resulting in malformations.
Regardless of which style of side is used, a visual inspection should always be carried out behind the ear to check the fitting of the sides.
Young Infants
There may be a need for babies of only a few weeks old to wear glasses, if, for example, they are left aphakic following cataract surgery. Babies under the age of four months will not be able to support their own head and a frame with long sides that extend beyond the ear or loop ends rarely work. Babies’ heads need constant support whether they are lying down or being held. Long sides or loop ends with straps will be pushed forward causing the glasses to fall down the nose. The glasses need a small eye size of 34mm or 35mm eye or even 32mm for tiny or premature infants. For these patients a frame with perfectly fitted soft curl sides may be the best option. Alternatively, the Tomato baby range can be considered. These have adjustable soft, silicone end tips which curve behind the ear and can also be held in place with a well-adjusted spectacle strap.
Bridge Styles
The fit of the bridge is extremely important as it supports around 90% of the weight of the spectacles.1 Prolonged pressure on the crest of the bridge could cause the fatty tissue to break down and potentially cause deviation of the septum.1 Table 2 shows some mean bridge measurements for children over a range of ages.
The bridge should spread the weight of the frame over as large an area as possible in order to provide the maximum support with the least pressure. The different bridge styles available are:
‘Pad on arms’
‘Pad on arms’ can easily be adjusted but they need frequent adjustment because with wear, the distance between pads becomes too wide causing the glasses to sit too low on the face so that the child ends up peering over the top of the frame. If the pads provided with the frame are not suitable, they should be changed. Silicone pads are softer, hypoallergenic and often help to provide more grip on the nose. Larger pads may be used to spread the weight over a larger surface area, while smaller pads can be useful for small noses in order to avoid the inner canthus. The pad arms can also be removed and re-soldered at a different point on the nasal rim to give a suitable crest height.
Strap bridges
A ‘pad on arms’ bridge can easily be converted to a strap bridge. This style of bridge is better at spreading the weight over a larger surface area but again, needs frequent adjustment in order to prevent the entire weight being carried on the crest of the nose.
Saddle Bridges
A saddle bridge spreads the weight well and is good at absorbing any impact. This is the ideal style of bridge for a young child wearing a metal frame.
Bridges on plastic frames
For plastic frames, the bridge should match the shape of the patient’s nose exactly and be in constant touch all the way round. A gap at the top indicates the bridge is too narrow. A gap at the bottom means the bridge is too wide and will result in the glasses falling down.
To improve the fit of a plastic frame ‘pad on arms’ can be fitted onto the back after the plastic pads have been removed. By attaching the pads below the HCL, the crest height will be reduced and the glasses will sit higher on the patient’s face. Adding the pads will also increase the BVD which may be useful for patients with negative bridge projections to prevent the lashes rubbing on the back of the lenses.
Keyhole bridges
Keyhole bridges can work for some older children as the shape distributes the weight of the glasses along the sides of the nose rather than on the crest.
Table 2: Bridge measurements for age1

Specialist fits/modifications
A study carried out by Woodhouse et al looked at facial measurements for children with Down’s syndrome aged between seven and 14 years.8 The results showed that their facial characteristics do not change with age and are not comparable to those of children without Down’s syndrome. The children in the study tended to have the following:8
- Smaller crest height
- Bridge projection that decreases with age
- Smaller frontal angle
- Larger splay angles
- Smaller PDs
- Smaller apical radii
- Shorter length to bend
- Larger temple width
- A head width larger than expected in younger children and smaller than expected in older children
Clearly, these patients require a more specialist fit with frames that take into consideration their different facial characteristics. This is particularly important given that around 77% of children with Down’s syndrome suffer from a refractive error9 and up to 80% of school age children with Down’s require correction for accommodative problems.10 Despite this clear need for appropriately fitting spectacles, in 2011 the Down’s Syndrome Association conducted a survey of its members and found that 45% reported that their glasses were poorly fitting or uncomfortable.11
Erin’s World is a range of specialist frames for children and adults with Down’s syndrome. The frames have the bridge attached at a point much lower on the nasal rim to account for a smaller crest height, as well as shorter sides that can be easily cropped and adjusted to ensure a suitable length to bend and length of drop. The wider lugs mean that the boxed centre distance can be kept smaller to match the patient’s PD, while allowing for larger temple widths.
Tomato glasses can also work well for children with Down’s syndrome. Fitting the bridge on the lowest of the three settings lifts the glasses and stops the patient looking over the top. The sides can then be cropped to the right length to bend and be held securely in place with a strap to prevent them slipping down.
For children with abnormal head shapes, for example those with craniosynostosis, standard glasses do not usually provide an adequate fit. The NHS spectacle voucher allows high street practices to claim an extra supplement on frames for children with special facial characteristics.12 Glasses should either be handmade or a standard frame can be extensively modified. Although patients with craniosynostosis are normally under hospital care, they may want the spectacles dispensed by a local optician. Practitioners, in conjunction with companies carrying out the required modifications need to ensure that the fit of the glasses is satisfactory. This may require more than one modification.
Lens selection
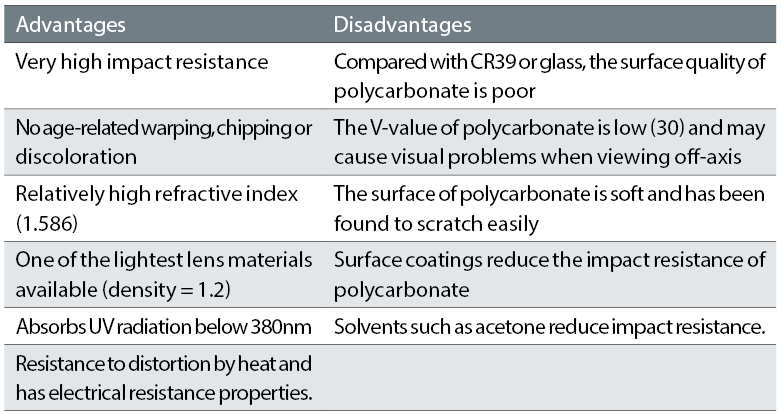
CR39 is the standard lens dispensed in the UK today.3 This is because it is fairly light and durable, has good optical properties while still being relatively low in cost. For children however, there are more suitable lens options which can provide a stronger, more robust lens suitable for their often active lifestyles. Polycarbonate is thinner and lighter than CR39 and has a very high impact resistance but the optical properties are not as good and the V-value only 30 (compared with CR39 which has a V-value of 58). This may induce some chromatic aberrations and some patients may experience colour fringing. Trivex has a much higher V value (45), has good impact resistance, good chemical stability and UV absorption, making it an ideal lens choice for children with low to medium prescriptions.16 Tables 3 and 4 show summaries of the properties of these materials.1
Table 3: Properties of polycarbonate
For higher prescriptions, children may prefer a high index material. However, the cost for parents should be considered if the prescription is being changed frequently.
Small blank sizes are advisable of medium to high hypermetropic prescriptions to avoid unsightly, heavy lenses. While aspheric lenses may produce thinner flatter lenses for adults, this is not always the case for children as the aspheric blanks may not be available in the small sizes.
Aphakic prescriptions
Patients left aphakic following cataract surgery require lenticular lenses with as large a bowl as possible for the frame size in order to reduce any scotomas from the carrier lens. However, as with full aperture lenses, the boxed centre distance of the frame should match the patient’s PD as closely as possible to avoid decentration, and the frame aperture should not be smaller than the bowl size otherwise it will cut straight into the bowl and expose the thickest part of the lens.
Ultraviolet
Children have clearer ocular media than adults, so they may be particularly susceptible to UV damage. Sunglasses should be encouraged, or photochromic lenses may offer an alternative option. For aphakic patients, a lenticular lens must always be dispensed with a UV filter.
For patients with severe photophobia, a wrapped frame is ideal. Figure 5 is an example of a frame dispensed to a patient who had severe photophobia. The wrapped frame still left open areas at both the temporal edges and so leather side shields were fitted to block out any remaining light.
Table 4: Properties of Trivex

Measurements
All measurements should be taken at eye level. Measure vertical heights for high or anisometropic prescriptions in order to avoid any unintentional prismatic effect.
Pupil distance
Because children’s faces do not always develop symmetrically, the PD should be measured monocularly, occluding each eye in turn. Since this is not always possible, one of the following alternative methods may be used:
- Temporal pupil-iris margin to nasal pupil-iris margin.
- Temporal iris-sclera margin to nasal iris-sclera margin.
- Temporal canthus to nasal canthus.
Bifocals
A large segment bifocal (such as a D35) is preferred with the top of the segment set at the lower pupil margin to encourage and enable its use. Executive bifocals are not suitable as they are heavier and thicker, especially for hypermetropes, less cosmetically pleasing and harder to keep clean. After measuring the bifocal line, the demo lenses can be marked up with a marker pen. The child can then be observed to check that they are looking through the correct portions for distance and near.
Figure 5: A frame dispensed to a patient who had severe photophobia

Progressive powered lenses (PPLs)
For older children requiring a reading addition, especially pseudophakic patients, PPLs will give better cosmesis and a better range of working distances. A frame with enough depth is required in order to prevent any reading area being lost. A freeform lens design (individualised lenses designed and produced using computer numerically controlled technology) would be ideal as a child’s smaller pantoscopic angle and PD etc can be incorporated into the design to ensure the widest areas of clear vision are achieved with less distortion and fewer aberrations.
Communication
Being confident, having good communication skills and endless patience is vital when carrying out paediatric dispensing. The practitioner needs to balance the needs and wants of the child, with those of the parent or guardian. This is often referred to as ‘the duality of the patient’.18
For some parents it can be a shock to discover their child requires glasses and they may have many fears and questions that need to be addressed before starting the dispense. Take time to explain what the prescription means, why the glasses are needed and the importance of a good fit. This will help the parents to gain confidence in you as the practitioner and listen to your advice on the spectacles.
The whole process should be a positive experience for the child. A fun dispensing area with bright colours can help to put the child at ease and make the dispensing process run a lot more smoothly for everyone. Flashing toys or mobile devices can be invaluable for getting children’s attention and distracting them, allowing the fit of glasses to be assessed and measurements taken.
With children there may only be a small window of opportunity to try on frames before they lose concentration. It is therefore important to be as accurate and efficient as possible. Always address the child directly and try to use simple terminology they can understand with concise sentences. The entire dispense should be carried out at the patient’s eye level, even if this means sitting on the floor with the patient.
Parent and child should never be left alone to choose glasses without any guidance. Find a suitable selection that fit well and let the patient choose from these. This will avoid the patient choosing something inappropriate and being disappointed when they are told they cannot have them. By letting the child have the final decision, it will help them feel some ownership of the glasses and may encourage wear. For little ones who are reluctant to try glasses on, try to make it into a fun game. A good strategy may be to get mum or dad to try some on first.
For first time wearers, give the parent/carer advice on how to care for the glasses and tips on encouraging the child to wear them such as putting the glasses on the child when they are doing something they enjoy, for example a computer game or colouring. This will help them to associate the glasses with a positive experience. If children are encouraged to take good care of the glasses from an early age, they are less likely to need constant repairs. Frequent breakages may mean the patient has to rely on an older pair that is not the right prescription or fit, while the broken ones are being repaired. Providing the patient with a nice spectacle case and cloth will encourage this.
Outline the professional services you offer. Due to the active nature of children, their glasses may need frequent adjustments. Parents should be encouraged to bring patients back to check the fitting of the glasses at least every two to three months. Ensure that they have your contact details to contact you whenever necessary if they have any concerns relating to their children’s sight or glasses. Further, the NHS entitlements should be explained so that parents know what to do if the glasses get broken or lost. Although the NHS does not provide a spare pair, it might be worthwhile for the parents to consider purchasing a back-up pair in case of an emergency. It is always a good idea to keep spare frames or parts in stock so that the glasses can be repaired with as little delay as possible. •
Jessica Gowing is the senior dispensing optician in the ophthalmology department at Great Ormond Street Hospital for Children (GOSH). The dispensing opticians provide a specialist dispensing service for children with a wide range of conditions and complex prescriptions as part of the multi-disciplinary team which includes optometrists, ophthalmologists, orthoptists and vision scientists.
- This article is based on material first published in Optician 17.10.17 in our Great Ormond Street series on paediatric eye care.
References
- Keirl A, 2010, Paediatric Eyecare - part two, Anthropometry and spectacle frames for children, Dispensing Optics, 25, 10.
- Obstfeld H, 1997, Spectacle Frames and their Dispensing, W B Saunders and Co Ltd London UK, pp188-189.
- Association of British Dispensing Opticians, Pathway to Dispensing to Children, A reference guide for ABDO members, 2017, Available from: http://www.abdo.org.uk/wp-content/uploads/2012/06/Pathway-for-dispensing-to-children-0617.pdf [Accessed online 13th August 2017].
- Grisdale E, 2015, Fashion Weak? How you can make the difference between a fashion hit and a fashion flop, Elaine Grisdall, Dispensing Optics, 30, 8.
- Bates S, 2014, Dispensing handmade frames, Optometry Today.
- Abbott J, 2015, Plastic Fantastic, Dispensing Optics, 30, 1.
- Hughes E, Key Considerations when dispensing children’s spectacles, Dispensing Optics, 29, 1.
- Woodhouse JM, Hodge SJ and Earlam RA, 1994, Facial characteristics in children with Down’s syndrome and spectacle fitting, Ophthal. Phsiol. Opt, 14, 1.
- Pueschel S M, 1987, Health concerns in persons with Down’s syndrome. New perspective in Down’s Syndrome, Paul Brookes Publishing, Baltimore USA.
- Woodhouse JM, Meades JS, Leat SJ, Saunders KJ, Reduced accommodation in children with Down’ Syndrome, Invest OPhthalmo Visual Sci, 34, 7.
- Thompson, 2015, Downs Syndrome Association, Data to Produce better fitting specs, Available from: https://www.downs-syndrome.org.uk/news/data-to-produce-better-fitting-specs-can-you-help-2, [accessed online 13th August 2017].
- Abbott J, 2016, Special Measures, Dispensing Optics, 31, 8.
- Great Ormond Street Hospital, Available from: http://www.gosh.nhs.uk/medical-information/craniosynostosis, [accessed online 13th August 2017].
- Great Ormond Street Hospital, Available from: http://www.gosh.nhs.uk/medical-information/crouzon-syndrome, [accessed online 13 August 2017].
- Taylor D, Hoyt G, 2005, Pediatric Ophthalmology and strabismus, third edition, Elsevier, Edinburgh.
- Cripps A, 2015, An Overview of Paediatric Dispensing, Part 2: Communication and lenses, Dispensing Optics, 30, 10.
- Rideout VJ, Foher UG, Roberts DF, 2010, Generation M2: Media in the Lives of 8-18-Year-Olds: A Kaiser Family Foundation Study. Menlo Park, Calif. Available from: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8010.pdf (PDF, 2.73MB), [Accessed online 13th August 2017].
- Wilson D, 1999, Practical Dispensing Open Training and Education Network South Wales Australia pp265.
