It’s sometimes said that handling contact lenses is as easy as brushing your teeth. But patients’ real-life experiences suggest that’s not always the case.
While we may assume we’re doing a great job when teaching our patients how to apply and remove their lenses, patients themselves report that we ‘could do better’.
Johnson & Johnson Vision interviewed consumers, eye care professionals, psychologists and industry experts to gain a better understanding of contact lens handling and identify new ways of addressing our patients’ concerns.
Here’s what we learnt…
The problem
What we know about the consequences of difficulties or concerns with contact lens handling is summarised in figure 1. To understand these problems in greater detail we conducted consumer research, first with over a thousand consumers, and then in-depth interviews with a further 21 individuals.
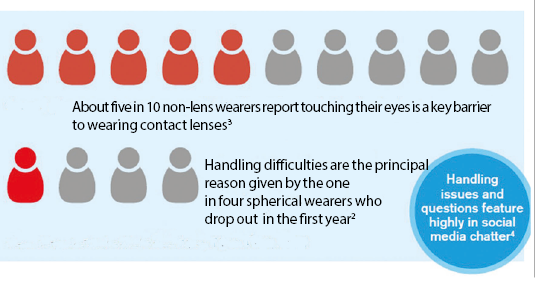
Figure 1: Concerns and difficulties with handling
We interviewed 1,200 consumers in four countries who had either considered, trialled or dropped out from contact lens wear.¹ We identified that 19 individual steps are needed to apply and remove a contact lens (figure 2). But we also found as many as 155 ‘unique needs’ that consumers use to measure the successful completion of the job. For instance, not only do wearers have to remove the lens, they also have to minimise the likelihood of losing it when attempting removal – whether the lens is off-centre, under the eyelid, or in the sink.
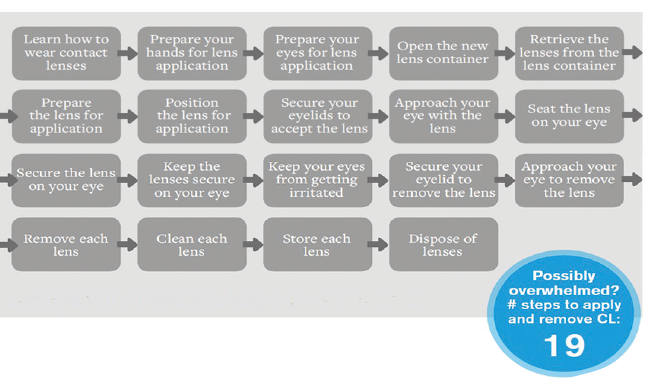
Figure 2: Individual steps in lens application and removal
The complexity of this apparently simple process has also been highlighted in a recent study which suggests that as many as 53 steps may be required for patients to be fully compliant with daily lens wear and care of reusable lenses.5
From our study, we learnt that the key handling steps patients consider of highest importance and lowest satisfaction are:
- Preparing and positioning the lens for application
- Applying the lens to the eye
- Removing the lens
In fact, only one in four triallists were motivated and satisfied enough with the way they were taught to put their lenses on and remove them, to become wearers.¹
Consumer stress levels and time taken
We then conducted 21 in-depth home interviews among contact lens wearers and those who were trialling lenses.6 The aim of this ‘time and motion’ study was to find the time taken to complete each step in the application and removal process and to monitor the wearer’s stress levels (see figure 3).
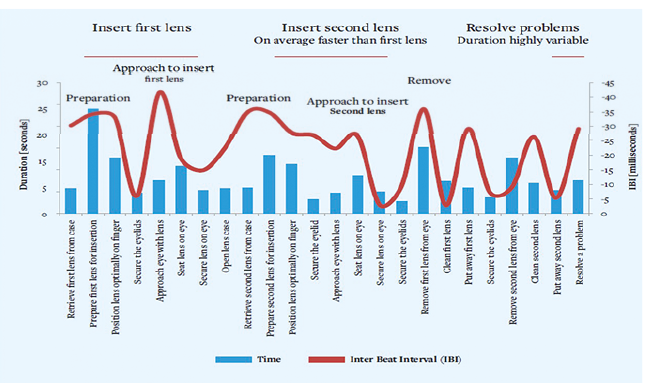
Figure 3: Time and motion study results
Devised by psychologists, this study was designed to help differentiate patients’ perceptions of lens handling issues from the actual difficulties they experience and to understand levels of anxiety at each step in the process.
The time and motion study told us:
- Many contact lens wearers skip preparation steps – preparing the lens and positioning it on the finger – to save time, but this can result in problems
- Application, and resolving difficulties with application, takes most time
- Approaching the eye during application and removal induces the most anxiety
Of special concern were issues with lens application technique. Wearers report difficulty securing the upper lid adequately, which inevitably results in blinking as the lens approaches so that it either falls off the finger or sticks to the lid or lashes.
Contact lens education may also take place in a less than optimal environment. Lack of privacy, lack of hygiene in the teaching area and a lack of empathy or trust in the person conducting the teaching can also undermine success.
The Myths: Many and varied
The consumer interviews also revealed as many as 30 different fears about contact lens use, whether related to the eye, the lens, the wearing process or concerns about complications.1
Although some fears will be familiar to anyone who discusses contact lenses with patients, others may seem surprising. Being aware of all potential anxieties allows us to prepare for reassuring our patients.
Importantly, whilst not all consumers have these concerns, nearly eight in 10 contact lens considerers agreed that such fears could be a barrier to wearing lenses.¹ Considerers fell into two distinct high and low fear groups – in other words, they were either fearful or they weren’t.¹ And this wasn’t the only revealing finding. Although fear could interfere with the education process, there was no correlation between anxiety and ease of application and removal.
What we found was that the stronger the motivation of the patient to succeed, the higher the satisfaction with their ability to apply and remove lenses. Our research therefore dispelled some common myths about lens handling, discussed in Table 1.

Table 1: Common myths about contact lens handling
The Opportunity: Motivation
Since we know motivation drives satisfaction, it’s important to understand individual motivating factors. So we also identified the specific ‘triggers’ that drive consumers to try contact lenses, whether to look good, avoid being awkward, hide their vision problems or not have to wear glasses.¹
The top-ranked motivations were not having to ‘squint’ to see, having ‘180° vision’ and feeling more confident overall. We can use this knowledge to help drive our patients’ motivation to wear contact lenses.
Remember that not all triallists have the same level of motivation. Highly motivated patients – whether their level of fear is high or not – achieve high levels of satisfaction with wearing lenses. Satisfied patients experience anxieties and handling difficulties too, but their motivation enables them to persist.
Top tip
- Once we’ve recognised which driving factor is most important to an individual we can use that to re-motivate that patient during the contact lens teach and encourage them to continue
The opportunity: Best practice teaching methods
A wide variety of methods are used in practice to teach lens handling, and patients introduce different approaches to application and removal themselves. This can lead to variable and unpredictable wearer success. Addressing this through consistent in-practice training, the use of written and digital support materials, and regular practice follow up appealing to patient motivations rather than fears, can help to reduce this variation.
Handling contact lenses can be a challenge for some
There are significant opportunities to improve where, when and how education takes place, especially in this digital age.
If we could make the process more consistent and effective by establishing an evidence-based ‘Best Practice’ for educating our patients, they would have a better chance of enhancing their satisfaction and continuing with contact lenses.
We’ve identified a significant opportunity to combine science with clinical experience to help develop better teaching and learning of lens handling. Attention to environment, approach and process can help make your contact lens teach more effective.
The solutions
From our research and studies, making handling easier from the patient’s perspective depends on optimising three factors in practice; environment, approach and process (Figure 4).
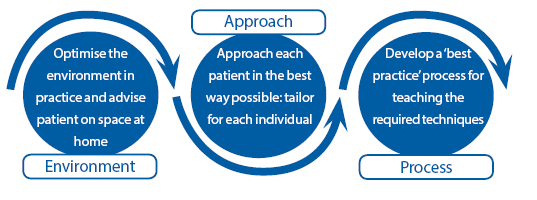
Figure 4: Three factors to consider to make handling easier
Let’s look at each of these in detail and see what our ‘Best Practice’ for teaching lens handling might look like...
1 An optimum environment
It may go without saying but an unhygienic practice environment or a teaching area lacking in comfort or privacy is not conducive to successful patient education.
Lack of hygiene may provoke negative emotions and cause the patient to withdraw. And feeling exposed when trying to overcome barriers can make patients feel uncomfortable and more likely to give up.
So, ensure your contact lens teaches are conducted in a private, clean area with access to a sink, well lit mirror, lint-free tissues, contact lens solutions and support materials. Remember to advise patients that the home environment is just as important. Recommend they select a quiet, dedicated space to practice in at home, away from cluttered bathrooms with their hazards of sinks and toilets.
2 An optimum approach
Using empathy and building trust plays an important part in relieving patients’ fears and anxieties. We found that patients who have a higher level of trust in their eye care professional achieve significantly higher levels of satisfaction.4
Gentle, positive communication is the best teaching approach. Encourage and congratulate the patient after each successful step and allow plenty of time for them to build confidence.
It’s also worth investing time and resources in training staff to ensure all involved in teaching are proficient, well motivated and worthy of recognition as handling experts.
Help set expectations and emphasise that lens handling needs practice and the importance of establishing a routine. Use analogies relevant to their daily life, such as ‘tying your shoelaces’, ‘riding a bike’ or ‘learning a new dance move’. These involve many steps too.
Top tips to relieve anxiety
- Allow your patient to touch a contact lens during fitting
- Ensure your staff are prepared and confident in all aspects of the teaching session
- Give exercises prior to fitting, such as touching the white of the eye with a clean finger, to help desensitise the eye and lid reflex
- Ask patient to relax their breathing and jaw to relieve tension
- First have the patient approach the eye with the lens, but without putting it on
- Regularly mention why the patient first wanted contact lenses to re-motivate
3 An optimum process
Our overall aim should be to apply best practice training to everyone, while remaining aware that not all our patients are the same. We need to appreciate that some patients learn more quickly than others or have difficulty with particular steps. Use your experience in practice to tailor your teaching to each patient. And be aware that patients will adapt their own technique as they gain confidence and experience.
Break the process down into small steps, explaining why each is important. Pay close attention to those steps we know patients struggle with, especially lens preparation, positioning and application. Digital resources should be recommended to supplement your face-to-face contact.
With so many steps to consider it’s easy to lose track of which are most important. Here’s our list of three key tips for patients for successful application and removal overall:
- Ensure hands are dry to make lid and lens handling much
- easier
- Secure the lids by placing two fingers at the lid margins, one above the eye and one below (figure 5)
- Approach the eye slowly, not quickly, and make fewer attempts
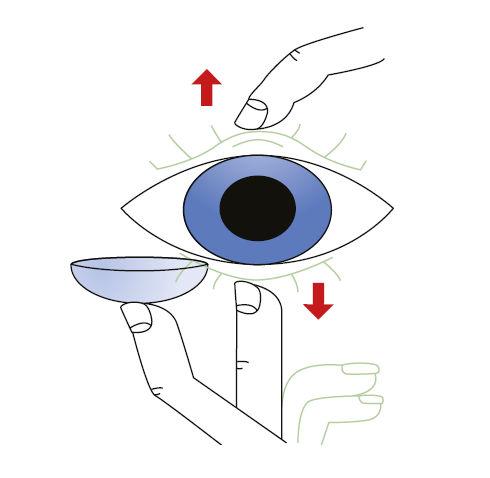
Figure 5: Holding the lids the correct way to secure lids is an essential first step for successful lens application in a new wearer
Also keep in mind the following:
- Approaching the eye to apply the first lens is the most stressful step
- Repeated failures cause anxiety
- The number of failed attempts counts: slow down and concentrate on quality rather than quantity
- Watch your language: talk about ‘applying’ or ‘putting on’ a lens rather than – more alarmingly – ‘inserting’ it.
- Watch for increasing anxiety levels – patients cannot retain information when feeling stressed.
Top tips
- Not all lenses are the same to handle. Modulus can affect handling, and some lenses have low surface adhesion which can aid removal.8
- Design features such as a visibility tint or the inversion indicator can help with preparation.9
Once home, experiencing repeated application and removal failures may result in frustration. We need to provide effective learning aids – written information, video links and apps – that are available 24/7, to support patients in their home environments through the early stages.
We should offer practical tips on the optimum environment for trialling contact lenses at home. Examples might be trying them first at the weekend or during school holidays – without the pressure of getting to work or school – or during practice hours, when help is at hand if needed. Don’t forget to provide a contact number to call with any questions or concerns.
Finally, arrange ongoing contact with the patient. In addition to a follow up appointment, a phone call from a member of the practice team after a couple of days can be invaluable to address any difficulties that may have arisen early on, and keep motivation high.
The early stages of contact lens wear are crucial to ongoing success. Use our checklist to communicate with new wearers:
- Congratulate and encourage
- Give information on the product and why it was prescribed, and reassure them that other lenses are available if for any reason they are not satisfied
- Give written information, supply link to application and removal video and apps, and provide contact details for any concerns
- Arrange a progress phone call after a few days and a follow-up appointment
- At follow up, check performance (vision and comfort) using 1-10 scales and offer alternatives if not working well
There are many opportunities to help improve retention among those new to contact lenses. While both vision and comfort are important factors, confidence in lens handling and habit formation play significant roles in new wearers, especially in the first few weeks of wear.10
So in summary, there’s a huge opportunity to help our patients achieve success and to keep them in contact lenses. Implement simple changes to optimise the environment, approach and process to deliver ‘Best Practice’ handling education and support for your patients
Key points
Problem
- Only one in four wearers are satisfied with the way they are taught handling1
- Handling difficulties are a key reason for dropout in new wearers2
- Preparing and positioning the lens for application are key issues for patients1
Opportunity
- Optimising the teaching of contact lens handling can reduce dropout and benefit patient and practice
- Recognise patients’ personal motivations: these, rather than fear or anxiety drive satisfaction with lens handling
Solutions
- A better environment, approach and process can all help in patient success
- Use a full range of resources for contact lens teaching and learning
- Direct patient to digital support which is available 24/7 to supplement face-to-face teaching
Jane Veys is Director, Global Professional Education & Development at Johnson & Johnson Vision
References
1 JJV Data on file 2014. Training Wheels Research. n=1,200 Quantitative interviews in China, Japan, Russia and US with considerers, triallists and dropouts
2 Sulley A, Young G and Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye 2016; 40:1 15-24
3 JJV Data on file 2017 Quest Study
4 JJV Data on file 2016 Social Listening Project
5 Efron N and Morgan PB. Rethinking contact lens aftercare. Clin Exp Optom 2017; 100:411-431
6 JJV Data on file 2014. Training Wheels Research. n=21 wearers. Qualitative home interviews and observations. China and US
7 Court H, Greenland K and Margrain TH. Evaluating patient anxiety levels during CL fitting. Optom Vis Sci 2008;85:7 573-80
8 Scales C, Popwell S, Pall B et al. Sticky business: How cross-linker content can have a profound effect on the adhesiveness of contact lenses. Invest Ophthalmol Vis Sci; 2017; 58: ARVO E-Abstract 3094 (AO348)
9 Sulley A, Osborn Lorenz K and Jubin P. Handling: the forgotten factor in soft contact lens success. Optician 2013; 246:6426 25-30
10 Veys J and Sulley A. Pay attention to retention. Optician 2017; 253: 6604 26-30
Thanks to Audrey Adams, at Johnson & Johnson Vision, for her input, and Alison Ewbank for help in preparing this article
