Twenty years ago, the RNIB Low Vision Centre and Camden Social Services set out to create a partnership that was the first of its kind in the UK and which soon became a gold standard model for adoption elsewhere. It aimed to bring together optometrists and rehabilitation workers one day a week, in the consulting room, to arrive at the best possible outcome for four patients seen on any one day. Fast forward to 2018, and we are still going strong and generating positive feedback from our clients. The ‘joint partnership/holistic approach’ became a winning formula because the skill sets of a rehab worker and an optometrist complement each other so well.
We sit together during the assessment when people come to the centre or visit them at home with our respective equipment. Most importantly, we still only see four people a day to give each patient plenty of time – something that is painfully lacking in a hospital setting due to the various time constraints. It’s a very rewarding way of working.
Yet I’m not sure how many people in the field truly understand the full extent of what rehab workers do? I hope this article will shed some light on our relatively obscure but incredibly valuable profession.
The Rehabilitation Worker
I qualified 20 years ago at the then School of Vision in Surrey. The title ‘rehabilitation worker for the visually impaired’ is a bit of a mouth-full to start with, but it stops people assuming we work for AA or help drug addicts. We have actually been trying to think of a better name for years … to no avail. We’re so much more than ‘mobility officers’, or ‘braille teachers’ hence we had to come up with a job title that encompassed a broader range of skills.
The ‘rehabilitation’ in our job title simply means helping people to safely regain their independence by teaching them different ways of doing things. In reality, there is nothing ‘simple’ about it. It takes an average 12 months of lectures (full-time) and a six-month placement within a social services setting, or similar, to be fit for the job and pass our DipHE in Vision Studies.
LVL/RVI/CVI
- The low vision leaflet or LVL has superseded the letter of Visual impairment (LVI).
- The LVL can be given by optometrists to any patient they feel would benefit from contact with the sensory impairment team at social services. The patient can then complete the leaflet and send it to the sensory impairment team themselves.
- Optometrists in both community and hospital practice can also make a referral to social services using an RVI (referral of visual impairment).
- This may be useful for patients that are either not eligible or have declined registration at the present time or who have not seen an ophthalmologist that are struggling with day to day life due to a sight impairment.
- Certification of suitability for registration as sight or severe sight impaired depends on the completion of a certificate of visual impairment (CVI) by a consultant ophthalmologist
Example of a low vision leaflet
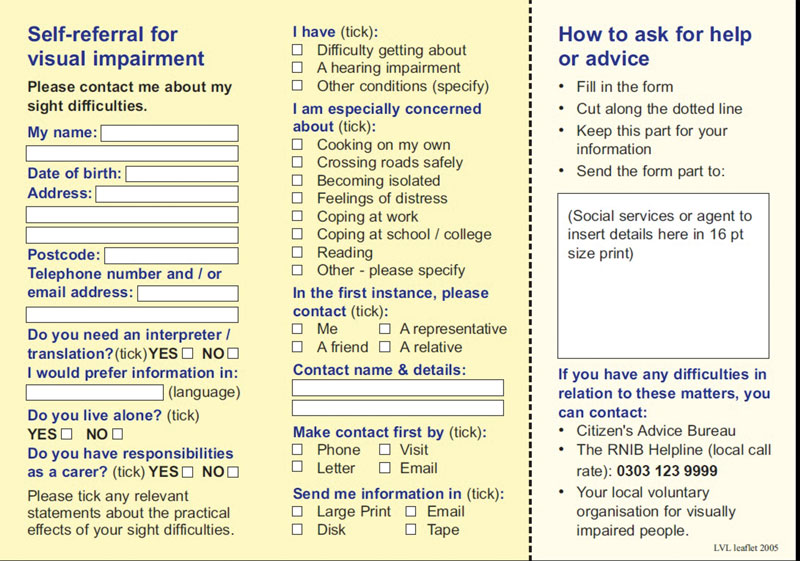
We get referrals from various sources (such as eye care, health and social care professionals, family members, charities) but the most common source is the hospital eye service. Once patients have signed their Certificate of Visual Impairment (see box), their GP and local social services will also get a copy. Upon receiving it we have a duty of care to make contact within two days to check how they are coping and undertake a home visit within 28 days if we mutually agree that a visit would be beneficial.
During the assessment, and especially if the person is newly certified as sight or severe sight impaired, the rehab worker will need to cover everything they need to think about from the moment they wake up, until the moment they go to bed again. Things like:
- How do they even know it’s time to get up?
- How will they colour-match their clothes?
- Can they make a cup of tea or toast?
- Are they able to go to the local park or local shop?
- Will they dare prepare a more substantial meal later?
- Will they see their medication to identify it correctly?
- Can they make a phone call?
- Will they be able to read their post so they don’t miss out on vital hospital appointments?
- Can they read their e-mails?
- Have they been told about the various new benefits they may be entitled to?
The challenges that arise with sight is lost can seem overwhelming. Yet simple strategies, adapted equipment or just specific advice about lighting can help people immeasurably and reduce their anxiety levels accordingly.
Over the last 20 years, the progress in technology alone has been mind boggling and visually impaired people have benefited from a wide range of apps and gadgets that we could not have even dreamt of when I qualified. But for the older generation, who are still the vast majority of our client base, having an app on a phone can feel a bit … well, scary.
Figure 1 A signature guide

But the more simple, rudimental aids stand the test of time: a signature guide will ensure they keep their signature ‘within the box’ for legal documents (figure 1), a large button phone will make it easier to call relatives (most will have one-touch buttons we can programme too), a liquid level indicator (figure 2) will ensure they don’t over spill, a symbol cane will make others aware they struggle to see properly, a talking clock will tell them it’s the middle of the night and they should try and go back to sleep, and so on.
Figure 2 A liquid level indicator

Figure 3 A patient using a mouse linked magnification system

Key Areas
Eye conditions It is essential to have a good understanding of the symptoms, causes and prognosis of sight loss and understand the impact each has. This is important if effective help is to be offered.
Low vision aids The optics of low vision aids needs to be understood so advice on their best use can be accurate. These include the familiar hand-held magnifiers, along with adapted TV, computer mouse linked systems (figure 3), a wide range of electronic magnifiers (figure 4), and monocular and binocular telescopic systems (figure 5).
Figure 4 A portable (a) and a desk top (b) electronic vision enhancement system
A
B
Figure 5 TV viewing telescopic appliance

Various viewing strategies Strategies such as eccentric viewing (for those with a central scotoma) and steady eye strategy (where the viewer maintains fixation while the target is moved) sometimes need to be taught.
Lighting The inverse square law and which light source most benefits various eye conditions is important (figure 6). The downside of glare too, being mindful of reflections, shiny surfaces, shadows, all requires consideration. Even when there is little one can do, increased lighting can usually help as even dementia sufferers will be less confused if we minimise shadows. We will pay for minor adaptations in council and private properties but submit recommendations to housing associations as they will have a duty to help their own disabled tenants.
Figure 6 Stick-on LED light sources

Mobility We cover everything from sighted guide support to teaching complex routes. To do so will require using different canes and tips, and different ways of holding them
Mobility
Mobility alone took up 50% of our training time (with lots of hands-on practice, in various locations). It was substantial because as rehab workers we are essentially encouraging people with limited or no vision to take their lives in their hands by crossing roads. We may be working with people who have never had any cane skills at all, or with competent cane users who need to re-orientate themselves to commute to a new workplace or from a new residence. Either way, it means memorising a route and all its clues – there and back. Some journeys will be more complex than others, and some will include getting on and off buses, trains or the underground.
A rehab worker’s job, before we even start teaching a route, will be to assess which route will be best in the first place. And ‘best’ will not necessarily mean the shortest, but the safest. If, to travel from A to B, there are two or three options, a rehab worker will need to work out, based on an understanding of the impact of any particular eye condition, which option offers the most clues, the least amount of trip hazards or over-hanging branches and the safest crossing points. The ‘clues’ we are looking for can be anything from a slope, a texture, tactile paving (figure 7), manhole cover, grass, gravel), a canopy, a regular sound, a large red mail-box, and so on. Most controlled crossings are fitted with rotating cones in the UK, which helps deafblind people know when it’s safe to cross. Having a visual fields assessment from optometrist colleagues can be a great tool to gauge what clues we can use and which type of cane and tips would best help (the next article in this series will focus on visual fields assessment of the visually impaired).
Figure 7 Tactile roadside paving

Independent Living Skills
The first thing we usually do on a home visit is to maximise contrast and review the light level. Typical help offered might include:
- Mark-up microwaves or cookers with bump-ons (figure 8) so that people can set temperatures more accurately
- Demonstrate various cooking strategies (different ways of measuring ingredients for instance)
- Demonstrate how to make hot drinks more safely
- Agree upon safe ways of completing basic domestic tasks that might present a hazard, such as ironing and housework
Figure 8 Tactile elastic bands for identifying jars

Some days, the job can feel like ‘stating the obvious’ because I often see people pour hot water into a white cup, on a white saucer, on a white kitchen top and hear them ask why it’s so hard to find the cup. It’s all very well issuing a liquid level indicator that will beep when the mug is almost full, but you first need to ensure you can pour into the cup to start with. So, when people have got a predominantly white kitchen, I will give them a dycem mat (a piece of dark blue sticky plastic – figure 9). It they position the mug on it, it will keep it stable and its outline will stand out against the blue. Problem solved. It will even work with people who are down to 1.0 (6/60) or even hand movements.
Figure 9 A dycem mat
For those who have no light perception, we would teach different pouring strategies – which one is adopted will often depend on what other health issues they may have. No two home settings are the same. If someone has a heavily patterned table cloth yet complains of ‘losing’ things all the time, I will check its underside and, if it’s plain, will suggest they turn it over and use the other side instead. More often than not, rehab is not ‘rocket science’. If they drop things I can also teach them a systematic search pattern technique to increase their chances of not missing an inch.
Communications
This covers anything from being able to tell the time, to using a computer or smart phone. It’s now easier to use a voice command to call a particular person. Smart phones have opened up a world of endless possibilities for blind people. They can use them to play music, listen to talking books, act as GPS navigation aids, as bar code readers, face readers, and new applications appear regularly. For anyone interested in all these gadgets they can contact RNIB On-Line Today and a volunteer will come over to their home to demonstrate the many accessibility features (for some useful apps for the visually impaired, see Optician 8 June 2018). People who don’t (or won’t) have a smart phone, can still use the 195 BT Free Directory service, so long as their friends are in the Yellow Pages.
Reading
In Camden we rely on our optometrist colleagues to undertake low vision assessment and recommend magnifiers. If people are beyond standard optical magnification help and require electronic magnifiers of a particular design or scanners, we can demo these at the RNIB Resource Centre and the RNIB’s IT department (On-Line Today) should be the first port of call for anyone interested.
Multiple Disabilities
We know that 60% of people with a VI will have other health issues (including various learning disabilities, hearing impairment, multiple sclerosis, stroke, diabetes to name but a few). Taking them into account is essential for achieving a realistic and optimum management plan for each client group. Someone with multiple sclerosis or Parkinson’s may struggle to hold a magnifier or to make a cup of tea. We might try a clamp magnifier for the former and probably enrol the help of an occupational therapist (OT) for the latter. They would probably issue a hot water dispenser that will automatically stop when the mug is almost full. This being said, more and more health authorities now expect their rehab workers to undertake a Trusted Assessors course and then take on minor OT tasks to avoid the need for multiple referrals. However, for the purpose of this article, I will only focus on the ‘sight’ side of things.
For most people with additional disabilities, I would try and enrol the help of a carer or family member to reinforce any instructions (with verbal prompts or demonstrations) after I have left. We no longer have the time to visit three to four times a week (as we may have done in the past) as most sensory needs teams have shrunk dramatically in the last 20 years.
Benefits
We need to keep up to date with what visually impaired people are entitled to. However, this now tends to be covered by eye clinic liaison officers (ECLOs) who are based within the hospital eye service and see people immediately after they’ve been certified. They can also refer to local support charities.
Braille
We can read it, type it, teach it… but I’ll admit I have never managed to read it with my finger-tips, just visually. In 20 years, I’ve never been asked to teach it, not even Grade 1 (Grade 2 is far more complex with hundreds more contractions to memorise). Braille certainly has its place but it does take a huge amount of time and patience to learn. It certainly does not come ‘naturally’ for those with acquired sight loss and around 90% of people who are fluent braille readers were born blind.
Processing Emotions
Being certified as sight or severe sight impaired is a big deal and a life-changing moment. You cannot and should not do this job if you do not have the necessary empathy to understand this. We are not counsellors, but we do need to remain sensitive to what people are going through and give them space and time. There is no point forcing someone into using a long cane (even when you know it’s the best thing for them) until they are ready to use it. A long cane (or even a symbol cane) can be the hardest thing to accept because it validates that this is ‘it’ – no going back.
Many newly registered people feel like a fraud using a white stick as they wrongly assume that only those in total darkness (with no functional vision) qualify. Thankfully the RNIB offers telephone phone counselling and courses, such as the excellent Living with Sight Loss course, and we will ensure anyone who needs emotional support will be cared for along these lines. Importantly, these courses allow an opportunity for the individual with sight loss to meet other people who have previously experienced what they are going through.
We do some of our training using blindfold or simulation spectacles. This helps us to gauge what it feels like to be sight guided and to put your trust in a stranger. But we can still take the blindfold off at the end of the day. So, I never pretend to know what sight loss really feels like. Interestingly, but maybe not surprisingly, a large number of rehab workers are visually impaired themselves and I’m sure they make great role models.
Working with Children
We have received training in the differences between working with children and adults, but about five years ago habilitation studies were introduced for those wanting to specialise in helping visually impaired children. The ‘re’ is dropped from ‘rehabilitation’ because children will be taught life skills from scratch, not learning adaptive strategies. Children usually have a lower attention span, will need different canes and other strategies, and so working with them was deemed worthy of a dedicated diploma developing a different skills set.
Referral process
In Camden, service eligibility criteria is non-correctable sight loss in both eyes. The Care Act 2014 is vague on this, but our criteria works as a general rule of thumb. We do not need people to be registered, or even registerable, to be able to help them, so long as they need more than just spectacles to function safely. However, the sight loss has to be in both eyes, as one fully functioning eye will be enough to undertake most tasks properly. If sight loss is due to cataract, and since cataracts are technically correctable, we would first need to ascertain the risks involved until the time that surgery can take place. If surgery is imminent, we will only issue the bare minimum to keep a patient safe. Often this is simply the issuing of some UV shields (figure 10).
If surgery is not possible, we would give advice on how to minimise disabling glare and falls risk. This might include;
- Fitting net curtains over windows to diffuse the light
- Explaining the need to avoid reflective surfaces
- Suggesting darker UV Shields or peaked headwear when stepping outside on a sunny day.
The 3 Bs and the importance of good lighting
A visually impaired person’s reading ability can dramatically improve with the three Bs – that, is making things:
- Bigger
- Bolder
- Brighter
As we get older, we all need extra light but with many eye conditions (such as glaucoma or retinitis pigmentosa) one needs up to seven times more light than average. I have had clients who had been issued with higher powered glasses and magnifiers for years, when all they needed was increased lighting.
I once saw a patient who could just about manage N18 when sitting in his armchair, reading the newspapers headlines, but immediately jumped to N8 when I gave him a daylight floor standing lamp, with flexible arm. His glaucoma was severe and he had a significantly constricted visual field. He could see my face in full if I stood about two meters away, but would not have seen me try to shake his hands. He had convinced himself that he would see the TV much better if he sat very close to the screen. This was, in fact, the very opposite of what he needed to do to see the whole picture. By suggesting he moved his armchair much further away from the screen and read his newspaper with a daylight lamp positioned directly above his lap, his home life was completely transformed. He had already bought a floor standing lamp himself, but it was the wrong type of bulb and had been positioned wrongly.
I have lost count, over the years, of the number of people who have proudly stated that they have a lamp ‘just behind their sofa’… as if that is where it should be! But the inverse square law means that distance is more important than wattage and a 13W task lamp positioned below someone’s eye level, across their lap, will be 17 times more powerful than the same lamp in a ceiling light by the mere virtue of it being much closer.
Daylight lamps are usually much better than halogen. Again, numerous people I have visited have been proud to show off their ‘mother and child’ lamps, often bought at great expense, with a tiny bulb casting a narrow beam of line. The halogen lamp temperature is often way too hot to the touch, and therefore dangerous, and may cast a yellow hue, making it harder to read newspaper print.
Daylight quality is far superior because it has a cooler colour temperature and will boost contrast, making colours more vivid and reducing eye strain in the process. It will also radiate further and people will not get a blister if they touch the diffuser by mistake. The energy saving is just the icing on the cake when it makes reading labels on food packaging (usually of various colour contrast) so much easier.
Light emitting diode (LED) lamps (figure 6) have similar properties and cost even less to run, but the bulbs are difficult to replace when they break. LED works well in torches and I always recommend that people who can’t tell their colours apart use LED torches to differentiate them better.
For patients with retinitis pigmentosa who don’t want to use a long cane at night, a zoomable torch can make a big difference. It provides an extra wide beam that can be condensed into a brighter, narrower beam, and helps to highlight finer detail. But what if they have co-morbidities, such as glaucoma and cataracts? This is when it gets creative: I have been known to issue a task light to increase lighting to a reasonable level for glaucoma and combine it with light grey UV Shields or a set of typoscopes to minimise the glare caused by the cataracts.
Other Help Available
Most councils have excellent day centres (most with multilingual staff) and offer a range of courses and IT training particularly useful for older people. A financial assessment may need to be completed though, as most councils now charge for attendance. The Care Act values social inclusion, and a lot of effort is put into linking people with various charities, for befriending services for instance.
The GDBA has its MyGuide scheme, to take people out and about, or teach friends and families how to sight-guide properly.
The Pocklington Trust has set up many support groups (face-to-face or via email and online forums), Blind Sports aims to keep people active. Age UK, BlindAid, Deafblind UK, the Royal Society of Blind Children all have befrienders and organise events. Some offer grants too. Not to forget the many charities that specialise in various eye conditions: The Macular Society, the Glaucoma Association, RP Fighting Blindness, LOOK UK for Children & Families, the Stroke Association, etc, to name a few.
The RNIB Helpline is really good at offering suggestions. Sightlinedirectory.org.uk also lists various charities around the UK (though I’m not sure it’s kept up-to-date).
Contact details for these organisations and a useful resource guide for eyecare practitioners (including a self-filling organiser for you to save useful local contacts -figure 11) is now available to download for free from the Visualise group at: www.visualisetrainingandconsultancy.com/resource-pack-health-pros/
Working Together
As explained earlier, visual ability can increase significantly with a suitable lighting. Clinical findings from my optometrist colleagues, such as contrast sensitivity measurements, allow me to issue task lighting immediately (I have a sub-store in my RNIB based office, funded by social services) and people can take them home, free of charge. If they struggle to hold a lower powered magnifier, I usually issue a lamp with a clamp magnifier attached to resolve this.
Stroke patients often have pretty good (N6/N8) static acuity, and often there is little room for improvement from spectacle correction adjustment. Patients may, however, struggle to read a newspaper because the sheer number of words is often more difficult to process after a stroke. I have had spectacular results using typoscopes with people who suffer from ‘over-crowding’. They are basically a A4 or A5-sized black piece of plastic with a narrow slot cut into it, so that only one line of print can be seen at a time. By reducing the number of words in view, the brain can fine tune the processing. Telephone numbers may need to be written down vertically, instead of horizontally, so that the person can dial out more easily even with a homonymous hemianopia.
If you are not directly working with your local rehab worker and can think of someone who has non-correctable sight loss in both eyes who might benefit from our practical help, then you could issue a LVL to alert their GP or social services (see box). Alternatively, a five-line letter or encrypted email simply stating what the condition is and what their latest vision findings are would go a long way to ensuring your patients get any help they may require. If not certified, they may not yet be entitled to a Freedom Pass, Taxi Card or Blue Badge, but they could still benefit from a daylight lamp, a dycem mat, or typoscopes (to name a few).
A CVI plays a crucial role in making us aware that people are out there. Difficulties of access occurs when people are borderline or are still receiving treatment. If there is any chance at all that a patient’s sight might improve, their consultant ophthalmologist will be very unlikely to certify them. But these people could be struggling already, and perhaps for many more years to come until they are certifiable. Optometrists should see themselves as the stepping stone to bridge that gap.
Sensory needs teams, as the name suggests, specialise in sensory loss and are usually made of rehab workers for the visually impaired, technical and rehab officers for hearing impaired clients and specialists with the deafblind (if councils abide by the Care Act’s guidance). Everybody in our field is very passionate about what we do and the difference we can make so please don’t hesitate to get in touch if you feel that any of what I have mentioned could help someone you assess.
UK-based rehabilitation workers have a Professional Network and a dedicated Facebook page to advertise the latest gadgets, research, or swap ideas on what works in complex cases. Between us all (about 500 of us in the UK and few in the States, Australia and New Zealand) we have ‘seen it all before’ so we should be able to find a solution to most challenges. •
Sylvie Macle is a rehabilitation worker with the RNIB based in Camden.
- To refer anyone to a RNIB service, please call their helpline on 0303 123 9999.
The RNIB is running a CET accredited course on low vision and including a chance to find out more about the various care services available. To book a place on ‘A holistic approach to Low Vision’ at the RNIB, Judd Street, London WC1H 9NE low.vision@rnib.org.uk Deadline for registration: 11th September 2018. Registration fee: £95
