
As eye care practitioners (ECPs; optometrists and dispensing opticians) working in low vision, there is perhaps a tendency to consider central visual function as our primary concern, as assessed with visual acuity, contrast sensitivity and/or reading function. Partly this is because the commonest cause of low vision in the UK is age-related macular degeneration (AMD),1 which predominantly affects central function and results in the primary complaint of many low vision patients being that of difficulty with reading.2 Potentially it is also because central visual loss is something we can do something about, at least to some extent: reduced distance or reading acuity can be compensated for by magnification, and contrast sensitivity loss by contrast enhancement (for example by using electronic aids, or with practical advice such as the classic ‘put fish on a dark plate, and steak on a white plate’).
However, reduced visual field or loss of peripheral visual function can be equally as debilitating as loss in central function. The impact of field loss is recognised in worldwide and UK specific definitions of visual impairment (table 1), whereby a person can be considered as visually impaired if they have a very restricted visual field even if visual acuity is good. Conditions which affect peripheral vision include those which result in general restriction of the visual field, such as glaucoma and inherited retinal disorders like retinitis pigmentosa (RP). Also to be considered are conditions that result in hemianopic or quadrantopic field loss, such as post-chiasmal lesions or cerebrovascular accidents (stroke). Some conditions affecting peripheral vision, RP especially, tend to have earlier onset than AMD, and people with peripheral visual loss therefore potentially face more ‘blind years’ than someone with central visual loss.
Table 1 Criteria for consideration as having ‘low vision’ or being ‘blind’ according to the World Health Organisation,3 and for being considered for registration as sight impaired or severely sight impaired in the UK through Certificate of Visual Impairment (CVI) registration4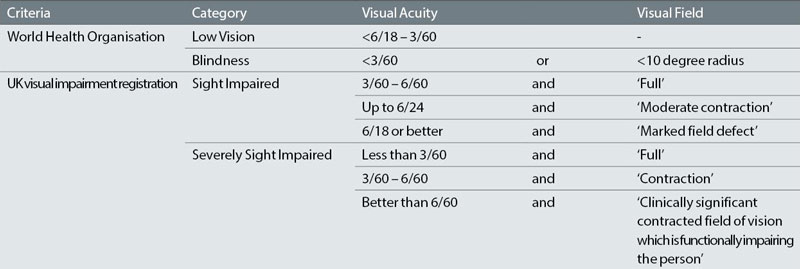
Despite the importance of peripheral visual function, my impression is that visual fields assessment is not often a cornerstone of low vision assessment, and I include my own low vision practice in this observation. Partly this may be due to considering visual fields as a test relevant to disease detection or monitoring disease progression, but not so much to low vision assessment. It may also be because visual field loss is not something that an ECP can actually do much about: the optical options for addressing visual field loss through field expanders such as reverse telescopes or Peli prisms are limited.
In this article, I would like to make the case for why assessment of peripheral visual fields in the low vision assessment is important, how visual fields might be assessed in these circumstances, and what might usefully be done with the information obtained to make it worthwhile having assessed this aspect of visual function.
Why assess visual fields in low vision?
Visual fields are commonly used in routine primary care practice to screen for disorders of the eye and visual pathway; in other words for disease detection. If a progressive disease such as glaucoma is diagnosed, then visual fields can provide evidence of the stability or progression of the disease. In the context of the low vision assessment, the purpose of visual field assessment is different. The key rationale for assessing fields here is to be able to quantify someone’s visual loss, and to relate the loss to functional difficulties that they may have as a result.
Impairment of peripheral vision leads to a number of difficulties with specific tasks, more formally termed ‘activity limitations’.3 Key limitations as a result of peripheral vision loss are around orientation and mobility, with specific aspects such as postural stability, gait, crossing obstacles, reaching and grasping tasks, and visual search all affected by loss of peripheral field (eg see5-7). It is therefore unsurprising that people with field loss are at increased risk of falling or have greater fear of falling,8 and that field loss specifically impacts on perceived difficulty with activities such as mobility both outdoors and indoors, shopping, using public transport and taking part in physical activity or sport.7
It should also be noted that although reading might be considered an essentially central visual task, it is reported as difficult by people with glaucoma,9 and people with worse glaucomatous visual field loss also engage less in reading tasks.10
Figure 1 Functional visual fields outputs from binocular threshold assessment (left), suprathreshold assessment (centre) and kinetic assessment (right) for two observers, one with less severe loss (top) and one with greater loss (bottom). Suprathreshold and kinetic results are obtained with a 10dB stimulus. While there are differences between the outputs, they tell much the same story in terms of areas of best and worst visual field. Figure courtesy of Dr Hikmat Subhi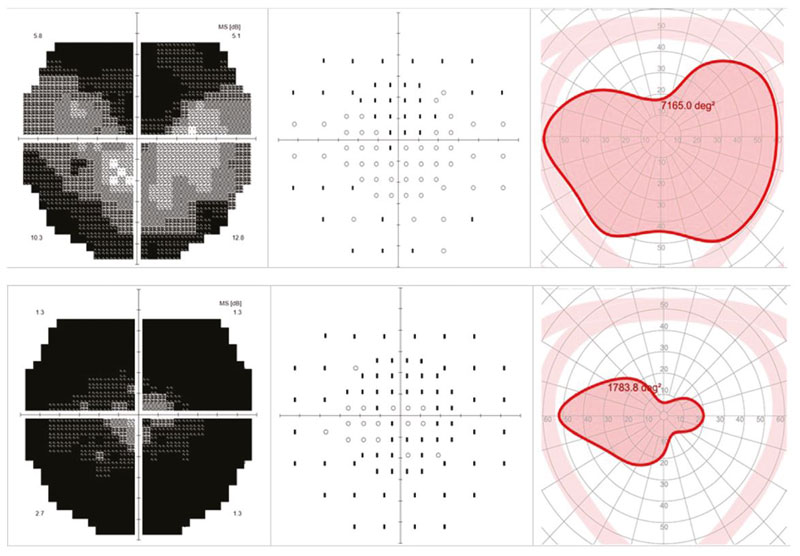 How to assess functional visual fields?
How to assess functional visual fields?
Given that assessing visual fields from a functional perspective could be important in low vision assessment, what sort of test should be used? The majority of commonly utilised visual field tests have been designed for disease detection or assessment of progression, and have not been optimised for functional assessment.
Firstly, it is important to specifically ask a low vision patient about mobility issues in case history. When asked as an open question to report their chief complaints due to their vision, low vision patients do not commonly report difficulties with mobility at rehabilitation assessments.2 However, if a structured questionnaire is used, asking how important and difficult a full range of rehabilitation areas are, mobility is identified as a key issue.11,12 It is possible that patients do not volunteer their difficulties with mobility as they do not perceive this to be an area that an ECP can help with. Equally, ECPs may not routinely discuss mobility issues with patients for the same reasons.
Assessment of functional visual fields should then be with the aim of identifying and illustrating areas of best and poorest vision. Key points to consider are:
Binocular assessment. Assess visual fields binocularly to reflect real world function, either by using a test designed for binocular use such as the Estermann, or by using a monocular test binocularly. Blind spot fixation monitoring will need to be switched off, and fixation monitored manually. It is possible that some patients may struggle with maintaining binocular fusion on the fixation target, but in our experience this has caused only limited issues. It should be remembered that any normative values provided by the test will not apply if a monocular test has been used binocularly. Monocular visual field results, if already available, can also be combined to produce an Integrated Visual Field using Medisoft Progressor software to provide a binocular functional field result.13
Assess fields beyond 30 degrees. Diagnostic visual field tests tend to assess the central 24-30 degrees of visual field. However, for representing functional vision, assessment of the field out to at least 60 degrees is ideal if possible, since peripheral vision beyond 30 degrees eccentricity relates as well or better to function in real-world tasks as the central 30 degrees.14
Use a ‘quick’ test. All types of visual field test (threshold, suprathreshold, or kinetic) relate well to functional ability,15 so any form of assessment can be used. However, quicker tests are unsurprisingly preferable to a patient.15 Examples would include an automated kinetic test, or a suprathreshold test with no additional quantification of defects. Confrontation can also be a useful way of identifying hemianopic or quadrantopic loss, or the approximate extent of a generally constricted field, and can be helpful to use with patients who would be unable to perform a more prolonged field test.
What to do with functional visual field results?
There is only benefit in assessing functional visual fields if something useful can be done with the results. This might include any or all of the following:
Show the patient. Many patients report not having seen results of their visual fields before, despite having undertaken a lot of visual field tests. In general, patients very much value seeing how their vision compares to normative values, as it can be difficult to be aware of the extent of one’s own field in daily life: are you consciously aware of where your own visual field limits are? People with peripheral visual loss certainly do not perceive their own vision as being a ‘black tunnel’ of the type commonly depicted in patient literature,9 and are much more likely to perceive either blurred areas in their vision or to be unaware of any loss at all. The Crabb Lab’s ‘Glaucoma in Perspective’ app (Allergan, Dublin) can also be very useful here.
Use visible output. It can be useful when selecting a functional field test to use to bear in mind the visibility of its output for showing to a patient (figure 1). Greyscales resulting from threshold assessments are intuitive to a patient and provide a high level of detail regarding sensitivity of function. Kinetic isopters are also clear to patients in their meaning, and while they provide less detailed information they highlight areas of good vision as opposed to the areas of vision loss that can be more evident in a greyscale output, and so can be positive from a patient’s perspective. Print-outs from some perimeters’ suprathreshold plots use very small points that can be hard for a visually impaired person to see.
Figure 2 Binocular kinetic visual field (red isopter) of a patient with rod-cone dystrophy who was just starting cane training. The pink shaded boundary represents normal visual field extent for comparison. Advice given to the patient, and shared with the rehabilitation officer, was to highlight the restricted inferior field (green arrow) suggesting that cane use to identify floor-based obstacles would be beneficial. Superior visual field (blue arrow) is even more restricted, suggesting the patient needs to be particularly careful to avoid superior obstacles like overhanging branches, possibly by use of extra scanning in this direction, or even by judicious use of hats! Laterally, vision is better, but the patient should be a bit more careful to scan to their left (orange arrow) as they are likely to miss more on this side.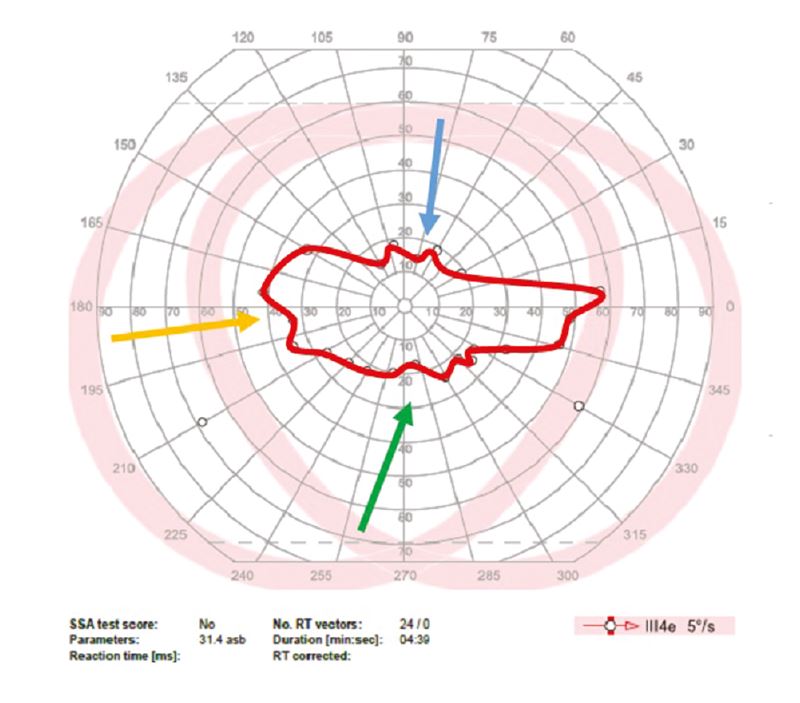
Provide functional advice. In addition to showing a patient their visual field, it is also important to explain the potential functional impact of this loss, and identify potential problems and solutions (figure 2). It can be useful to identify areas of the visual field which are better, which the patient can concentrate on utilising, as well as the problems associated with areas of greater loss. For example, significant loss of inferior field might lead to issues with tripping on obstacles such as kerbs or bollards. Patients with significant inferior field loss might particularly benefit from referral for cane training, since the cane can be used to identify floor-based obstacles. Even if referral is not desired or warranted, the information can still be useful – ‘that’s why I trip over the cat!’ exclaimed one patient being shown their inferior field loss. Patients with superior field loss can have problems with hitting overhanging objects, such as branches or low doors. Suggesting wearing a hat for partial protection might be useful, or again for the patient simply to be more aware that this area of their visual field is a particular issue. People with lateral field loss might experience difficulty in crossing roads, or navigating busy pavements. Additionally, they may have issues with reading since some peripheral field is needed to plan eye movements in the direction of reading, and to navigate back to the start of the next line of text. Hemianopes can be advised on how to best position objects such as food or the television in their working field. For example, someone with a left hemianopia might be advised to sit on the left-hand side of the sofa so that the TV is towards their right visual field.
Provide advice to carers. If a patient attends for assessment with a supporter or carer, such as their spouse or a family member, it also can be very valuable to show and explain the visual field results to them (with the patient’s permission of course). It can be particularly hard for a loved one to get their head around peripheral visual loss – how can they spot a pin on a table, yet walk into doors? Sharing information with carers, or providing copies of a functional field for the patient to use when explaining their loss to others, which can be particularly challenging,16 is a practically helpful outcome.
Provide the visual field information in referrals. Although the ECP may not be able to do anything specific about someone’s field loss beyond making a patient more aware of it, the information derived is valuable in prompting and supporting appropriate referrals to other rehabilitative services. Examples could include:
- Mobility training. Discussion with the patient and / or visual field results might indicate that the patient could benefit from orientation and mobility training, perhaps to include cane training. Service provision varies by area, and may require referral to the local authority or sensory services team, to a local sight loss charity, or via an ECLO (eye clinic liaison officer) if your local hospital has one. Including the field plot in your referral gives extremely useful information to the rehabilitation officer on a patient’s residual vision that helps plan mobility training (figure 2).
- Access to Work. Visually impaired people in the workplace can request adjustments to make their workplace more accessible through the Access to Work scheme. Provision of a visual field plot can provide helpful evidence of impairment to allow appropriate adjustments to be made.
- CVI registration. Although visual impairment registration can take place on the basis of visual field status, quite what represents ‘moderate’ or ‘marked’ field loss for registration purposes (table 1) is not always clear. Even the consultant ophthalmologists completing the CVI can be inconsistent in their judgements.17 Therefore, if a patient has obvious field loss and the patient would potentially benefit from visual impairment registration, ECPs are encouraged to refer patients for consideration for VI registration, providing functional visual field information to support that referral.
In conclusion, assessing visual fields and utilising the results obtained to advise patients on their visual loss and to facilitate appropriate referrals can be a valuable part of the low vision assessment.
Dr Keziah Latham is a Reader in Vision & Hearing Sciences at Anglia Ruskin University, where she leads the low vision service within the University Eye Clinic.
Acknowledgments
Some of the work referenced here is the PhD research of Ahoora Baranian (funded by Anglia Ruskin University) and Dr Hikmat Subhi (funded by the College of Optometrists). Their hard work and the support of the funders is gratefully acknowledged.
References
- Owen CG, Jarrar Z, Wormald R, Cook DG, Fletcher AE, Rudnicka AR. The estimated prevalence and incidence of late stage age related macular degeneration in the UK. Br J Ophthalmol. 2012;96:752–6.
- Brown JC, Goldstein JE, Chan TL, Massof R, Ramulu P. Characterizing Functional Complaints in Patients Seeking Outpatient Low-Vision Services in the United States. Ophthalmology [Internet]. 2014;121:1655–1662.e1.
- World Health Organisation. ICD-11 for Mortality and Morbidity Statistics (ICD-11 MMS) [Internet]. 2018 [cited 2018 Jul 3]. Available from: https://icd.who.int/browse11/l-m/en
- Department of Health and Social Care. Registering vision impairment as a disability [Internet]. 2017 [cited 2018 Jul 3]. Available from: https://www.gov.uk/government/publications/guidance-published-on-registering-a-vision-impairment-as-a-disability
- Crabb DP. A view on glaucoma—are we seeing it clearly? Eye [Internet]. 2015;30:304.
- Ramulu P. Glaucoma and disability: which tasks are affected, and at what stage of disease? Curr Opin Ophthalmol [Internet]. 2009;20.
- Latham K, Baranian M, Timmis MA, Pardhan S. Difficulties with goals of the Dutch ICF activity inventory: Perceptions of those with retinitis pigmentosa and of those who support them. Investig Ophthalmol Vis Sci. 2015;56:2381–91.
- Ramulu PY, van Landingham SW, Massof RW, Chan ES, Ferrucci L, Friedman DS. Fear of Falling and Visual Field Loss from Glaucoma. Ophthalmology [Internet]. 2012
- Crabb DP, Smith ND, Glen FC, Burton R, Garway-Heath DF. How Does Glaucoma Look? Ophthalmology [Internet]. 2013;120:1120–6.
- Nguyen AM, van Landingham SW, Massof RW, Rubin GS, Ramulu PY. Reading ability and reading engagement in older adults with glaucoma. Investig Ophthalmol Vis Sci. 2014;55.
- Bruijning J, Van Nispen R, Knol D, Van Rens G. Low vision rehabilitation plans comparing two intake methods. Optom Vis Sci. 2012;89:203–14.
- Macnaughton J, Latham K, Vianya-Estopa M. Principal difficulties of low vision patients entering rehabilitation. Optometry Tomorrow. Birmingham; 2018.
- Asaoka R, Crabb DP, Yamashita T, Russell RA, Wang YX, Garway-Heath DF. Patients Have Two Eyes!: Binocular versus Better Eye Visual Field Indices. Invest Ophthalmol Vis Sci [Internet]. 2011;52:7007–11.
- Subhi H, Latham K, Myint J, Crossland MD. Functional visual fields: relationship of visual field areas to self-reported function. Ophthalmic Physiol Opt [Internet]. 2017;37:399–408.
- Subhi H, Latham K, Myint J, Crossland M. Functional visual fields: a cross-sectional UK study to determine which visual field paradigms best reflect difficulty with mobility function. BMJ Open [Internet]. 2017;7:e018831.
- Latham K, Baranian M, Timmis M, Pardhan S. Emotional health of people with visual impairment caused by retinitis pigmentosa. PLoS One. 2015;10:1–17.
- Guerin E, Bouliotis G, King A. Visual impairment registration: evaluation of agreement among ophthalmologists. Eye [Internet]. 2014;28:808–13.
