As noted in the introductory article to this CET series, phakic intraocular lenses (pIOLs) have been commercially available for more than 20 years in Europe, demonstrating excellent visual outcomes with low rates of complications. The primary advantages of pIOLs are rapid visual recovery, a greater range of correction, reversibility, highly predictable outcomes, stability as well as preservation of accommodation.1
These lenses fall into two categories:
- Anterior chamber lenses, which are placed in the anterior chamber.
- Implantable contact lenses, which are placed behind the iris and in front of the natural lens.
The most commonly known of the phakic IOLs include:
- The iris- fixated Artisan/Verisyse and Artiflex/Veriflex (Ophtec BV, Groningen, Netherlands /Johnson & Johnson Vision, Santa Ana, CA, US).
- The Visian Implantable Collamer Lens family (ICL; STAAR Surgical, Monrovia, CA, US).
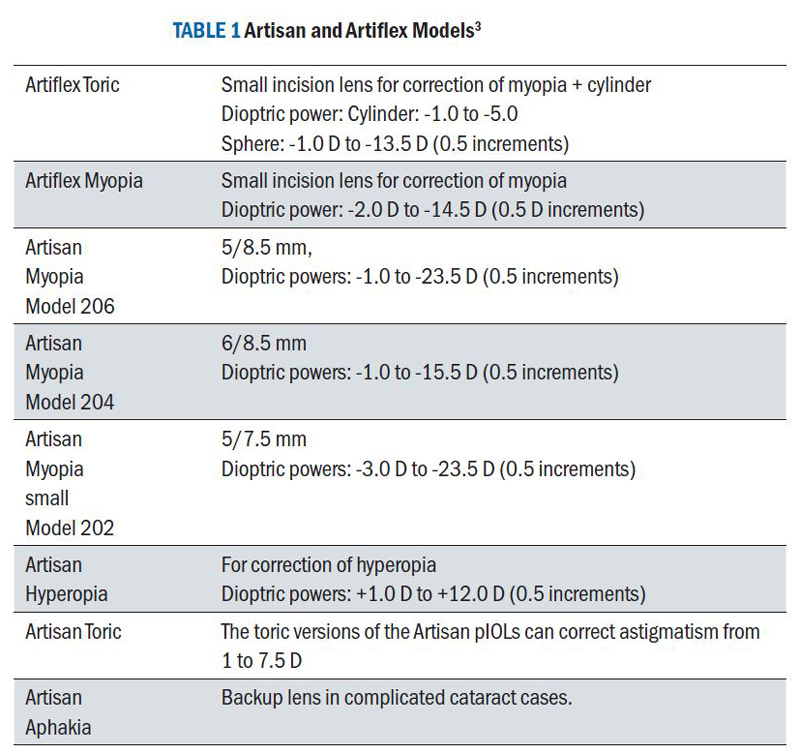
Table 1 Artisan and Artiflex models3
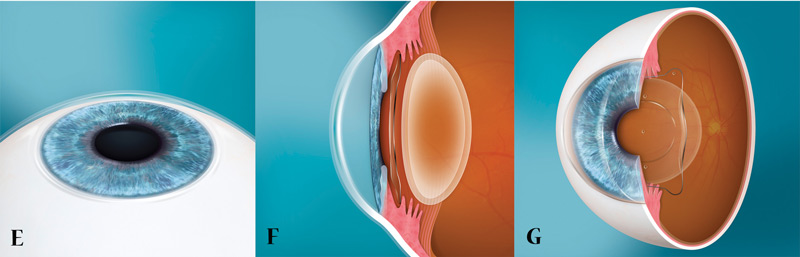
Anterior Chamber, Iris-Fixated Phakic Intraocular Lenses
The concept of an iris-fixated lens was first introduced in 1978 for aphakic eyes after cataract removal. Eight years later the inventor, Dutch ophthalmologist Jan Worst, developed a phakic model to correct myopia. Originally, these lenses were made of PMMA, a hard plastic, but the manufacturer, Ophtec, later introduced a foldable version made of polysiloxane, a silicone/polyacrylate hydrogel material that is also used in contact lenses. The company also developed models for the correction for hyperopia and astigmatism.2
Today, the Artiflex/Artisan pIOLs (marketed as the Verisyse lens in the US) provide one of the largest ranges of refractive correction for phakic correction, as well as in secondary/aphakic cases and in trauma cases.
These iris-fixated pIOLs are contraindicated in patients with:
- Low endothelial cell counts <2000 cell/mm2
- Shallow anterior chambers (<2.8 mm)
- Glaucoma
- Previous retinal detachment
- Macular degeneration or retinopathy
- Any form of cataract
- Recurrent or chronic iritis
- A fixed pupil size >4.5 mm or scotopic pupil size > 6.0 mm (5 mm PIOL optic) or 7.0 mm (6 mm PIOL optic)
- Convex, bulging or volcano shaped iris
- Eyes with corneal pathology4,5
Posterior Chamber Phakic Intraocular Lenses
The most commonly used posterior chamber phakic lens is the implantable contact lens which is implanted behind the iris and in front of the natural lens. As with the anterior chamber pIOLs, the ICL can correct for myopia and hyperopia, as well as astigmatism, covering a wide range of refractive errors.
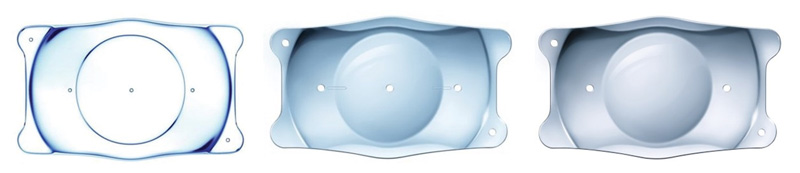
Within this class of lenses, the most frequently used is the Implantable Collamer Lens (ICL) from STAAR Surgical (Monrovia, CA), which has more than 850,000 lenses implanted globally, to date.6 These phakic lenses are made of a proprietary material called Collamer with a well-known track record of safety and efficacy.7-10 This pIOL comes in three models:
- The Visian ICL (myopia, hyperopia and astigmatism correction)
- The EVO Visian ICL (myopia and astigmatic correction)
- The EVO+ Visian ICL (myopia and astigmatic correction with an expanded optic)
The EVO Visian ICL family (figure 1) is indicated for use in phakic eye treatment and for the correction/reduction of myopia in adults 21 to 60 years of age with power ranging from -0.5 D to -20.0 D at the spectacle plane.11
Figure 1 EVO phakic IOL for correction of spherical myopia (left), astigmatism (middle) and hyperopia (right)
ICL vs Iris-fixated lenses
Sizing the ICL is the most important aspect of lens choice for the patient as the ICL is located in the posterior chamber and a large ICL could result in a large vault with angle compromise and too small a lens could result in dislocation and/or lens touch to the crystalline lens. While there are no issues when it comes to sizing the Artisan/Artiflex lenses which are fixated to the iris, they are located closer in proximity to the posterior surface of the cornea which can result in endothelial cell loss over time or if patients rub their eyes.12 Additionally, fixation to the iris can cause irritation and iritis in some instances as well as de-enclavation whereby the lens dislocates. This can lead to endothelial cell loss if not corrected expeditiously.
Advantages of the ICL
High refractive error
Implantation of the ICL is quick, minimally invasive and can be performed under local anaesthesia. Although ICL can be used as an alternative to laser refractive procedures, for any level of correction, the procedure can also correct high refractive errors that cannot be corrected by laser surgery.
No dry eye
Laser eye surgery involves the anterior corneal nerve plexus, which although returns to normal can for a period of time lead to dry eye and in rare cases permanent dry eye problems. As the ICL procedure does not cause dry eye, it is also a better option in those who have ocular surface problems often found in ‘contact lens failures’.
Preservation of accommodation
Because the crystalline lens is untouched, accommodation is preserved, which is a significant advantage over refractive lens exchange procedures, where the natural lens is removed and replaced by an intraocular lens. Refractive lens exchange is also more hazardous with an increased relative risk of retinal detachment.13
No change in corneal shape
Further, the implantable contact lens is an additive procedure, meaning the shape of the eye remains unchanged following surgery. The result is preservation of corneal tissue and maintenance of the corneal shape and corneal optics. In those with thin corneas or at risk of keratoconus where laser eye surgery is contraindicated, ICL is a good option.
Indications for use with the ICL
General criteria for candidate selection include patients between the ages of 21 and 60 with a stable refraction (less than 0.5 D change for one year) and a clear crystalline lens. In addition, an anterior chamber depth that is ≥ 2.8 mm, as measured from the corneal endothelium to the anterior lens capsule, is necessary.11
Ideal candidates must also meet minimum endothelial cell count (ECC) criteria and have no ocular pathology including compromised corneal endothelium, iritis, iris atrophy, rubeosis iridis, cataract, glaucoma, and retinal disorders.14
For myopes, the ICLs are available in a power range from -0.5 to -18 D, as well as in toric models up to -18 D of myopia and up to 6 D of astigmatism. For hyperopic patients, the power range is from + 0.5 and + 10.0 D, with up to 6 D of astigmatism in the toric version.
Sizing is the most critical issue related to ICLs. Thus, it is recommended that measurements are performed using diagnostics systems such as the IOLMaster 700 (Carl Zeiss, Jena, Germany) or the Orbscan (Bausch + Lomb, Rochester, NY) to ensure an accurate white-to-white measurement.
Pre-operative planning
The preoperative assessment includes:
- Manifest and cycloplegic refraction.
- Snellen uncorrected and corrected distance, intermediate and near visual acuity.
- Pupillometry.
- Applanation tonometry.
- Fundus evaluation. A fundus evaluation is required to ensure an intact peripheral retina and to document the status of the macular and vitreous.
- Corneal topography.
- Pachymetry and lens biometry preferably with partial coherence interferometry devices, including the measurement of the anterior chamber depth and white-to-white measurements to ensure selection of the correct ICL model.
- Specular microscopy to assess endothelial cell morphology and density.
- Lens calculations. Just as with intraocular lenses following cataract surgery, implantation of the Visian ICL requires a power calculation to ensure appropriate ICL selection. Typically, the post-operative target is emmetropia, but this is also dependent on the patient’s visual requirements.
Surgical Technique
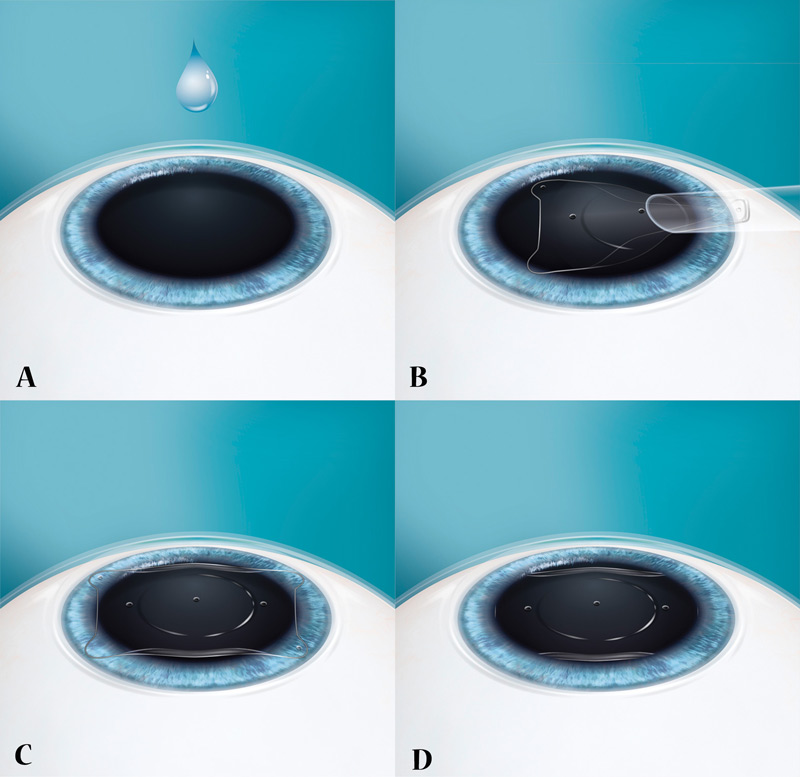
The ICL is implanted through a 3mm clear cornea, self-sealing incision under topical, regional or, in rare cases, general anaesthesia. Good pupil dilation is vital to ensure facile implantation of the footplates behind the iris.
Following incision creation and entry into the anterior chamber (AC), the chamber is filled with a viscoelastic device. The ICL is injected bevel-down into the anterior chamber and a blunt spatula is used to manoeuvre the lens under the iris and then positioned between the iris and the natural lens. The OVD is extracted, and the AC is rehydrated.
Previously, all STAAR ICL procedures required a preoperative YAG iridotomy or intraoperative peripheral iridotomy to avoid pupillary block. However, with the new V4C new generation myopic ICL the central area of the lens has a small opening which allows equalisation of pressure between the anterior and posterior chambers thereby eliminating the risk of pupil block and peripheral iridotomies are no longer necessary. The main steps of the process are illustrated in figure 2.
After surgery, patients are typically prescribed an antibiotic and corticosteroid for approximately one week.
Visual recovery is quick, with most patients seeing very well one or two days following surgery with complete recovery about two weeks, postoperatively. Second eyes are often treated soon after,16 however, increasingly patients are undergoing bilateral sequential surgery on the same day.
Figure 2 Schematic representation of key steps (a to g) in the implantation of the STAAR ICL lens
Potential complications to consider
As with any surgical procedure there are risks associated with ICL implantation, including: infection, raised IOP, over or under correction, damage to the crystalline lens, halos, glare and double vision.
Risks can be reduced with excellent preoperative planning and good technique.
Published Clinical Results
More than 100 peer review publications have evaluated the clinical results of the ICL, as well as the stability of these lenses and rates of post-operative infection. The papers included here are reflective of the data that has been reported.
These studies demonstrate the safety, efficacy, predictability, and stability of ICL for the correction of low, moderate, and high levels of myopia.17,18 Visual recovery time is like LASIK, ~1-2 week, with significantly fewer induced higher order aberrations (HOAs) and improved contrast sensitivity (CS).19
Alfonso, et al, the authors detailed the five-year follow up of 188 eyes implanted with the ICL. The results found that the mean spherical equivalent (SE) decreased from -11.17, + 3.40 D preoperatively to -0.23, + 0.50 D at 1 month postoperatively (95% confidence interval [CI] -0.15 to -0.02), while at 5 years the mean SE was -0.88, + 0.72 D (95% CI, -0.68 to 1.09).20
A Cochrane review compared laser refractive surgery to phakic IOL implantation for the correction of moderate to high myopia examined the published results of studies involving 228 eyes and concluded that phakic IOL surgery was safer than laser surgical correction for moderate to high myopia resulting in significantly less loss of best spectacle corrected visual acuity (BSCVA) at 12 months postoperatively.21 Neither technique resulted in any complication that caused a loss of final BSCVA. Phakic IOL surgery appears to result in better contrast sensitivity than laser correction for moderate to high myopia. The authors also concluded that phakic IOLs were preferred by patients.
Mertens has reported excellent safety and efficacy with the ICL implant, with, to date, no cases of cataract after implantation of the V4C model. He noted in a 2014 article that one of the motivating factors for implanting the ICL is the avoidance of exacerbation of dry eye that can commonly occur with LASIK with dry eye.22 In fact, up to 95% of patients experiencing symptoms of dry eyes after corneal refractive surgery.23
Higueras-Esteban, et al, retrospectively compared intraocular pressure (IOP) after implantation of the Visian Implantable Collamer Lens – the V4c and V4b designs – in 17 and 18 eyes, respectively, over a three-month period.24 In the V4c model, there is the addition of a central 360-µm hole, the KS-Aquaport, differentiates the V4c from the V4. The KS-Aquaport enables the natural flow of aqueous humour, eliminating the need for an iridotomy. In this study, there was no significant difference between pre- and postoperative IOP values. All but one eye was within ±0.50 D of the target refraction.
Conclusion
Phakic lenses have been available for more than 20 years in Europe. These lenses provide excellent visual outcomes, a very good track record of safety with low rates of complications and can be used to treat higher levels of refractive error, compared to laser vision correction. In addition, there is less risk of dry eye, corneal complications, as well as being fully reversible.
Phakic lenses are, unsurprisingly, experiencing considerable growth, increasingly recognised as a safe alternative to other approaches for refractive correction. Given that the procedure is capable of correcting myopia, hyperopia and astigmatism with extreme precision along with reversibility, the procedure is a good alternative to laser vision procedures especially when the latter is not an option.
Sheraz Daya is a consultant ophthalmologist and Medical Director, Centre for Sight, East Grinstead.
References
- Srinivasan, B et al, Modern Phacoemulsification and Intraocular Lens Implantation (Refractive Lens Exchange) Is Safe and Effective in Treating High Myopia. Asia-Pacific Journal of Ophthalmology 2016; (5); 6, November/December 2016. Available at; https://pdfs.semanticscholar.org/0137/717c39916a4df03b686a01842c1bc091f97b.pdf.
- https://www.ophtec.com/about-artilens/history. Website accessed on 23 August 2018.
- https://www.ophtec.com/about-artilens/artilens. Website accessed on 23 August 2018.
- Menezo JL, Peris-Martinez C, Cisneros AL, Martinez-Costa R. Phakic intraocular lenses to correct high myopia: Adatomed, Staar, and Artisan. J Cataract Refract Surg. 2004; 30:33–44.
- Huang D, Schallhorn SC, Sugar A, Farjo AA, Majmudar PA, et al. Phakic intraocular lens implantation for the correction of myopia: A report by the American Academy of Ophthalmology. Ophthalmology. 2009; 116:2244–2258.
- https://www.staar.com/. Website accessed on 23 August 2018.
- STAAR Surgical. Available at: https://uk.discovericl.com.
- Saunders DR. Anterior subcapsular opacities and cataracts 5 years after surgery in the Visian implantable Collamer lens FDA trial. J Refract Surg. 2008; 24(6):566-570.
- Packer, M. Meta-analysis and review: effectiveness, safety, and central port design of the intraocular collamer lens. Clinical Ophthalmology 2016: 10 1059-1077.
- Packer, M. Visian ICL: A review of the Literature. Cataract & Refractive Surgery Today Europe. September 2016; pp.8-11.
- https://uk.discovericl.com/about-evo#questions. Website accessed on 25 August 2018.
- Kohnen T1, Kook D, Morral M, Güell JL. Phakic intraocular lenses: part 2: results and complications. J Cataract Refract Surg. 2010 Dec;36(12):2168-94.
- Alio JL, Grzybowski A, El Aswad A, Romaniuk D. Refractive lens exchange.Surv Ophthalmol. 2014 Nov-Dec;59(6):579-98.
- Fechner PU, Strobel J, Wichmann W. Correction of myopia by implantation of a concave Worst-iris claw lens into phakic eyes. J Refract Corneal Surg. 1991 Jul-Aug; 7(4):286-98.
- Nanavaty, MA, and Daya, SM. Refractive lens exchange versus phakic intraocular lenses. Curr Opin Ophthalmol. 2012 Jan;23(1):54-61.
- https://www.centreforsight.com/treatments/implantable-contact-lenses. Website accessed on 25 August 2018.
- Kamiya K, Shimizu K, Igarashi A, Hikita F, Komatsu M. Four-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Arch Ophthalmol. 2009;127(7):845–850.
- Sanders DR, Doney K, Poco M, ICL in Treatment of Myopia Study Group United States Food and Drug Administration clinical trial of the implantable collamer lens (ICL) for moderate to high myopia: three-year follow-up. Ophthalmology. 2004;111(9):1683–1692.
- Igarashi A, Kamiya K, Shimizu K, Komatsu M. Visual performance after implantable collamer lens implantation and wavefront-guided laser in situ keratomileusis for high myopia. Am J Ophthalmol. 2009;148(1):164–170.e1.
- Alfonso JF, Baamonde B, Fernandez-Vega L, Fernandes P, Gonzalez-Meijome JM, Montes-Mico R. Posterior chamber collagen copolymer phakic intraocular lenses to correct myopia: five-year follow-up. J Cataract Refract Surg. 2011;37(5):873-880.
- Barsam A, Allan BDS. Excimer laser refractive surgery versus phakic intraocular lenses for the correction of moderate to high myopia. Cochrane Database of Systematic Reviews 2014, Issue 6. Art. No.: CD007679. DOI: 10.1002/14651858.CD007679.pub4.
- Mertens, E. Lasers or Lenses? The Ophthalmologist, Dec. 2014, Issue 1114: https://theophthalmologist.com/issues/the-stars-of-2014/lasers-or-lenses/. Website Accessed on 25 August 2018.
- Yu EY, Leung A, Rao S, Lam DS. Effect of laser in situ keratomileusis on tear stability. Ophthalmology. 2000 Dec; 107(12):2131-5.
- https://crstodayeurope.com/articles/2014-jun/comparison-of-two-icls/. Website accessed on 25 August 2018.