With the advent of silicone hydrogels, oxygen is rarely an issue and even extended wear is a practical proposition. Daily disposables even circumvent the chore of cleaning and storing the lenses. The biggest advantage of soft lenses, however, is that they are comfortable from the outset, unlike rigid lenses which require adaptation before acceptable levels of comfort are attained. In this world of instant gratification people are often not prepared to invest the time and effort to adapt to RGPs, but there are still some patients for whom RGP lenses should be first choice:
- Patients with irregular astigmatism due to corneal damage or keratoconus will only attain satisfactory vision with RGP lenses.
- Existing rigid lens wearers may not be satisfied with the visual performance of soft lenses.
- Patients with particularly exacting visual requirements will probably see better with RGPs.
- High minus prescriptions will result in lenses that are thickest at the edge of the optic zone. An RGP lens will leave the metabolically active limbal area uncovered and not restrict oxygen supply.
Initial measurements
HVID
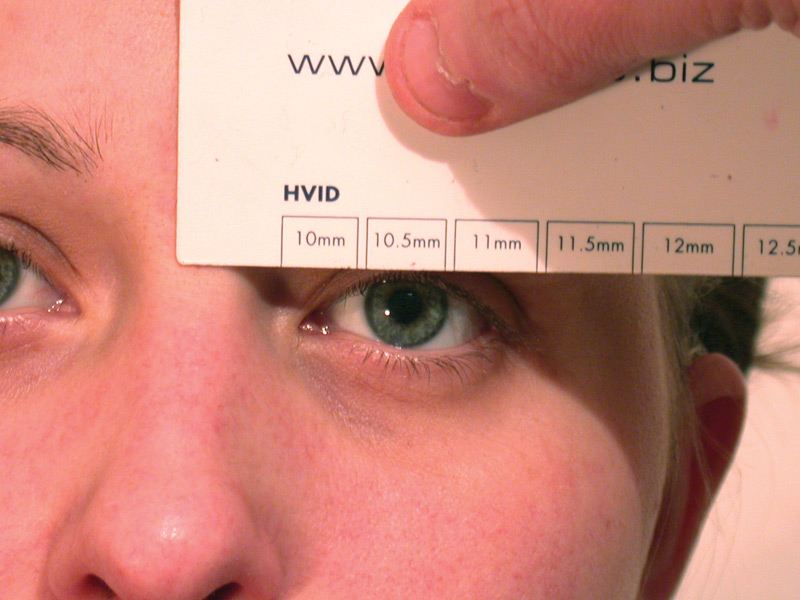
The horizontal visible iris diameter (HVID) is usually measured with a ruler (figure 1) but greater accuracy can be achieved by using a measuring graticule on a slit-lamp, thus eliminating parallax errors. However, even the cruder version is probably more measurement than we really need. The fact is that all ‘system’ lenses and most custom ones have total diameters between 8.5 and 10.00mm, which is going to be 1.50 to 2.0mm less than the normal range of HVIDs anyway, and selection of the total diameter has more to do with interaction of the lens with the eyelids than with corneal diameter. The only RGP patients for whom HVID is worth recording are those with abnormally large or small ones (megalo- and micro-corneal subjects).
Figure 1 Use of a rule to measure horizontal visible iris diameter
VPA
The visible palpebral aperture (VPA) is also measured, and it does at least give some indication as to how small a lens needs to be to be interpalpebral. Experienced practitioners rarely measure the VPA unless it is exceptional, and rather more useful information can be recorded by drawing the position of the lids in relation to the cornea (figure 2).
The position of the upper lid can influence the degree of lid attachment obtainable with a given diameter. The position of the upper lid prior to fitting may also be worth noting because long-term rigid lens wear can induce ptosis. The shape of the lids can influence horizontal centration, particularly if the lids are tight. The lower lid, if particularly low, can be associated with inferior corneal drying and with dropping lenses, particularly with prism-ballasted torics and translating multifocals.
Figure 2 Diagrammatic representation of lid position
Pupil diameter
The pupil diameter is also measured, both in normal ambient conditions and in poor light, using a Burton lamp when available, or a pupil guide if not (figure 3). The idea is to try to prevent flare from unwanted reflections from the peripheral curves of the lens by ensuring the back optic zone diameter (BOZD) of the lens is larger than the pupil.
Figure 3 A rule with a pupil diameter gauge
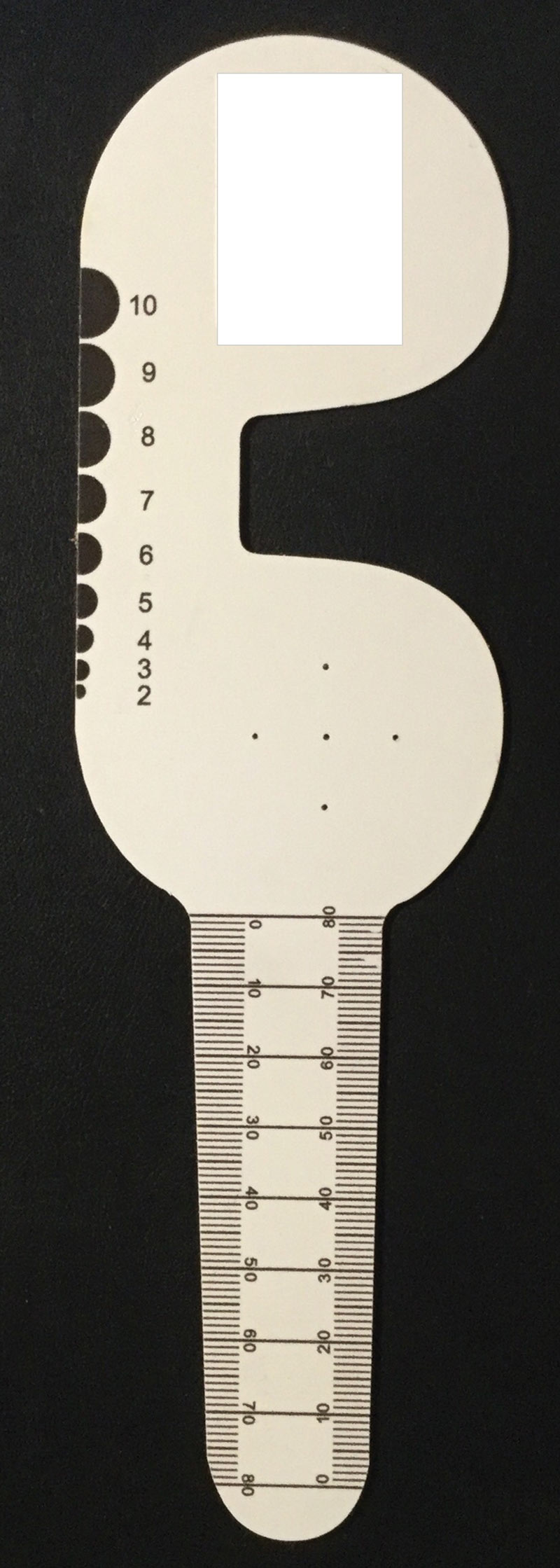
The pupil diameter will be at its largest in the dark. However, in anyone with dark irides, the process is often one of pure guesswork. Direct observation of the lens on the eye is rather more conclusive and patient satisfaction more relevant. It is also worth considering how much we are likely to be able to vary the BOZD. Generally, the BOZD is related to the total diameter, and most lenses fall into the 9.00 to 9.60mm range. 0.5mm is not likely to make a huge difference to flare. The other thing to bear in mind is that flare is not really much of a problem to most RGP patients. It is a bit like the scotoma associated with a spectacle frame. Most people get over it, because they are adaptable.
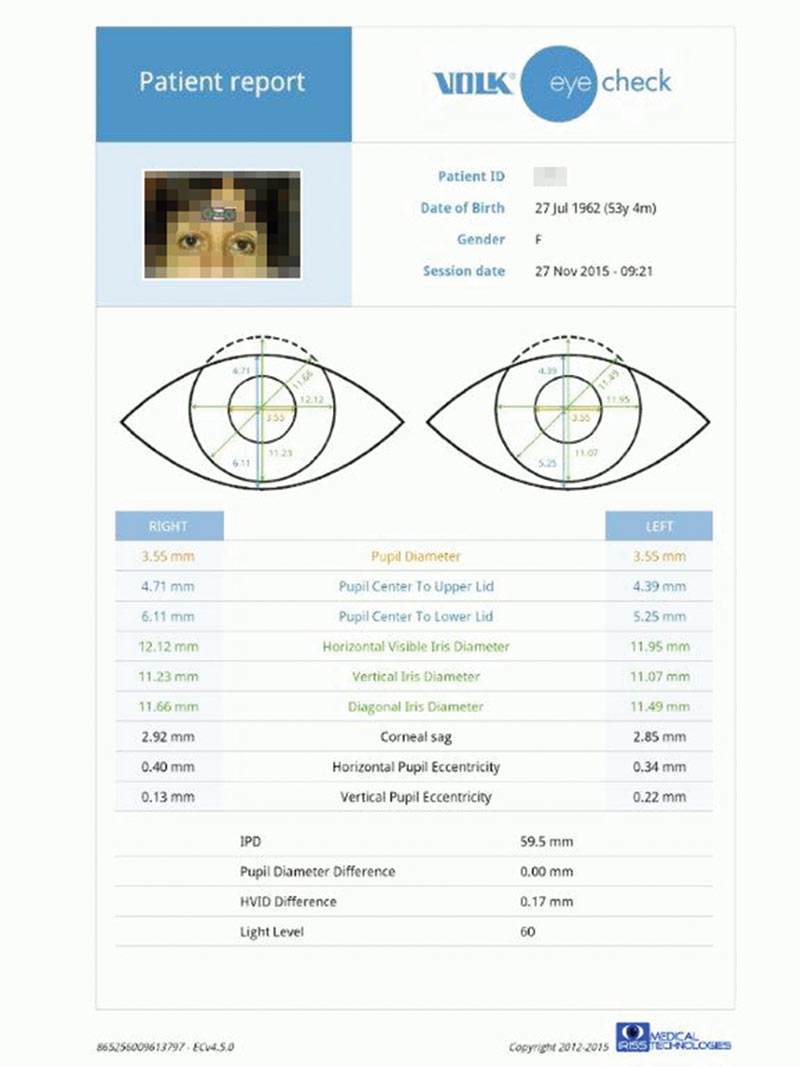
There are now automated photo-ophthalmic devices, such as the Volk Eye Check, capable of accurate measurement of the parameters mentioned here (figure 4).
Figure 4 Measurements using an automated photo-ophthalmic device
Selecting the diameters
How do we decide how big a lens we want, and why? The diameter of the lens influences the degree and type of lid/lens interaction. Smaller, interpalpebral lenses rely more on interaction with the cornea to determine their centration, but they can be uncomfortable as the edge of the lens may contact the sensitive lid margin during the blink cycle. If we can tuck the edge under the upper lid, away from the margin, the lens is likely to be more comfortable. In addition, the lid could hold the lens in position when the eye is open and then move it during a blink to aid tear circulation. On a cornea without a great deal of astigmatism, a larger optic diameter will allow us to spread the weight of the lens and the force of the blink on the lens over a large area. The greater the area of lens in close alignment to the cornea, the greater is the capillary force generated to hold the lens in place. We should not forget also that the larger the optic zone the less flare the patient will see.
It is possible to order any BOZD you like, if you are prepared to pay for custom lenses, but unless you leave enough room for the peripheral curves the transition from central to flatter peripheral curves is likely to be too abrupt. This can upset the tear exchange under the lens. For this reason, the BOZD is usually about 1.5mm smaller than the TD.
The simple rule when selecting a total diameter is to select a larger diameter, 9.60 or thereabouts, unless there are good reasons not to. Good reasons include:
- Astigmatism. The larger the diameter, the more difficult it is to maintain reasonable alignment in both meridians. If the BOZD is small enough, quite large corneal cylinders can be accommodated.
- Flexure. The degree varies with material and lens thickness, but lenses can flex about 30% of the total toricity of the cornea. Flexure creates uncorrected astigmatism in the over-refraction, and if the lens changes shape during the blink cycle because of the lid forces acting upon it, suction can be created under the lens as it returns to shape after a blink. This can affect the epithelium.
- Lid interference. If the lids are tight they may prevent the lens from centring properly. A lens with a total diameter smaller than the VPA may be required to minimise lid interaction with the lens. However, the result may be uncomfortable.
- Neovascularization. Where a former soft lens wearer is being fitted, a smaller lens may avoid the area where new vessel growth has arisen.
It is always a good idea to select diameters before thinking about radii. This is because of the shape of the cornea, which is the next thing to discuss.
Keratometry and Corneal Topography
Keratometry is still the most common measurement of corneal shape performed in optometric practice, and until fairly recently it was usually the only one. The cornea is known not to be spherical but its precise shape has been difficult to pin down. In general, it can be described as a prolate ellipse as it flattens towards the periphery. The degree of flattening (asphericity) can be expressed in terms of ‘eccentricity’ or as a ‘shape factor.’ The average eccentricity for the human cornea is 0.39, which correlates to a shape factor of 0.85. The problem is that it does not always flatten at the same rate, as shape factors vary by between +0.50 and -0.10. A negative value indicates a cornea that steepens peripherally, which occurs in about 3% of the population. There is little correlation between the rate of flattening and the values found by keratometry. Two eyes with the same K reading can have widely differing rates of flattening, even in the same individual. The rates may be different horizontally and vertically.
Modern topographical studies have identified five groups:
- Round (23% symmetrical, low astigmatism).
- Oval (21% asymmetric, low astigmatism).
- Symmetrical bow-tie (17.5% symmetrical astigmatic).
- Asymmetric bow-tie (32% asymmetric astigmatic).
- Irregular (7%, no pattern).
The asymmetric groups are interesting, because they have different rates of flattening in the upper and lower areas of the cornea, which can restrict lens movement. The numerous astigmatic bow-tie group have different degrees of toricity in the upper and lower corneas. This is worth remembering next time your lovingly prepared back surface toric will not do the decent thing and centre.
There are variations between different ethnic groups. For example, Chinese corneas tend to be steeper and flatten less towards the periphery. There is little correlation between spectacle Rx and shape factor, though high myopes often flatten less than expected, so tend to fit steeper than their Ks would suggest.
To see this in its clinical context, consider the ubiquitous keratometer. It measures the corneal curvature at points about 3mm apart (it varies with instrument and corneal curvature), either side of the visual axis. If you like, you can measure each eye three times and average the result. Be it one measurement or three, the value obtained tell us very little about the cornea we are going to be fitting, as we know nothing about the shape factor.
It all sounds a bit of a nightmare, but remember that we have been fitting rigid lenses for years and the ‘system’ lenses available from most manufacturers have undergone a process of evolution. Generally speaking, if you stick to the manufacturer recommendations or simply order on flattest K or thereabouts, the vast majority of lenses turn out to fit quite well. However, be prepared for surprises if ordering lenses empirically from K readings, due to the inherent unpredictability of it all. You should also prepare the patient for this, to avoid looking foolish.
Choosing the Back Optic Zone Radius
The intended relationship between the cornea and the back optic zone of the lens will depend on the fitting philosophy adopted. The lens is held in place on the cornea both by the eyelids and by surface tension, which acts at the lens edge where it is not covered by the lid. If the edge clearance is excessive no meniscus forms and there is no active surface tension. Reduced edge clearance and edge thickness boost surface tension. Broadly speaking, there are two extreme positions that can be adopted.
- Lid attachment. Essentially, the centration and movement of the lens is controlled by the lids, which pass the lens between upper and lower during the blink cycle. Lenses fitted like this do have a habit of riding a little high, especially in the long term, and exposure stain of the lower cornea is common.
- Interpalpebral. The lens is fitted with a small TD and BOZD to minimise lid interference.
Most lenses these days are fitted for an ‘alignment’ fit that is some way between the two extremes. The idea here is to fit the back optic zone in close alignment with the front surface of the cornea, with a uniform thin tear film between the two. This is a goal rather than something that is actually perfectly realised, but perfect alignment probably would not work very well. The advantages of an alignment fit are as follow:
- The weight of the lens and the force translated through the lens during the blink cycle are spread over the maximum area. If either is too localised, corneal warpage can occur.
- Lens flexure is minimised, which will ensure good visual performance and minimise mechanical stress on the cornea. This is quite an important consideration when using modern high Dk lenses.
- Provided that the periphery of the lens is also well designed, the thin tear film under the central part of the lens will be easily replenished with oxygen and never become stagnant. Furthermore, a thin tear film will not produce a major ‘barrier effect,’ slowing the movement of oxygen through the lens to the cornea. A thicker tear film could produce a situation where the rate of flow of oxygen allowed through the tear film was less than the rate that the lens itself is capable of. Barrier effects reduce the oxygen transmission of all RGPs, especially those with high Dks.
It should be remembered that K readings are taken at points not far away from the corneal apex, whereas we are trying to align an area of cornea over twice as wide. For the majority of patients, the spherical curve that will best align with the cornea will be somewhat flatter than K, and the wider the BOZD, the flatter we need to go. In practice, fitting on flattest K seems to work well with conventional designs of 9.00mm diameter or thereabouts. Once we get up to 9.50mm we need to go flatter because the average corneal radius is likely to be flatter. On a larger diameter the primary sag of a spherical curve increases, resulting in a steeper-fitting lens. Therefore, if you increase the BOZD by 0.5mm, you need to flatten the BOZR by 0.05mm to achieve a clinically equivalent fit.
Most lenses fitted on flattest K are probably a fraction steeper than alignment, but this seems to work well and may aid centration without seriously compromising in other respects. With an alignment fit, the practice of steepening the BOZR by a proportion of the corneal toricity is inappropriate as any steepening of the fit along the flattest meridian will only serve to push the whole lens further from the cornea, inducing central clearance. It will therefore have no effect on edge stand-off in the steeper meridian, which is the usual intention. It does sometimes help the lens to centre, however, if a back surface toric is not an attractive option.
If you are fitting an aspheric design, it is probably best to read the manufacturer’s recommendations, as the nominal BOZR initially selected will be related to the degree of asphericity (‘eccentricity’ or ‘shape factor’) of the lens design. The principles are similar though.
The Periphery
The periphery of the lens may be generated either by working a set (typically three or four) of progressively flatter spherical curves onto the back surface, or as a consequence of using an aspheric curve. In either case, it is worth considering what we have a periphery for. Part of the reason has to do with tear circulation under the lens. If we do not have edge clearance, tear fluid will not be able to get under the lens. This will have two effects:
- The lubricative effect of the tear film will be lost. The lens is then likely to adhere to the epithelium and eventually mechanical damage to this vital layer will occur.
- The oxygen normally carried by the circulating tears will be lost to the cornea under the lens. This is not too important provided the lens is able to transmit sufficient oxygen through its own substance, but for a lens of low transmission tear exchange may be an important source of oxygen delivery. Central corneal hypoxia will compromise epithelial integrity further.
Clearly, then, we must have enough peripheral clearance to allow adequate tear exchange. The other reason for peripheral clearance is that a certain amount of edge clearance is needed to allow the eyelids to dislodge the lens.
Modern system lenses have peripheries that are designed to give a smooth progression and, where spherical curves are used, the transitions between them are polished to blend the curves into one continuous surface. They are calculated to work on the majority of patients, but if a patient has an unusual corneal shape, too much or too little edge clearance will result. This can be detected once the lens is observed on the eye with fluorescein, and laboratories can increase or decrease the edge lift of the lens produced while keeping the optic zone the same. For a lens ordered empirically, a system lens is usually the best bet, unless you are aware of unusual corneal characteristics.
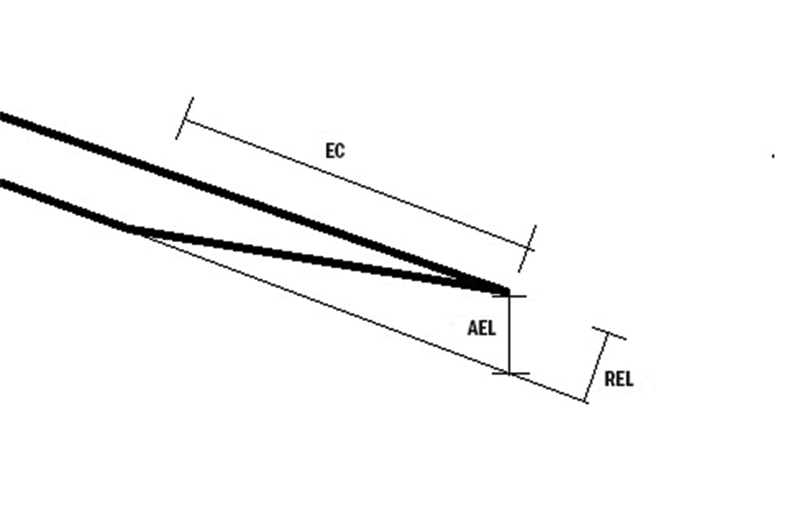
The terms ‘edge clearance’ and ‘edge lift’ are not interchangeable. Edge clearance refers to the gap between the front surface of the cornea and the back surface of the peripheral curves, and it is edge clearance that is observable with fluorescein. Edge lift is a geometrical characteristic of the lens itself, and is definable in either axial or radial forms. The difference between them is shown in figure 5.
Figure 5 Schematic representation of edge clearance (EC), radial edge lift (REL) and axial edge lift (AEL)
Edge profile
The shape of the edge is an important determinant of lens comfort, especially in the early stages. Laboratories tend to have their standard designs, but if you find that the lenses coming through are not as comfortable as they should be, you could ask for a different form. Generally, for the alignment fit with partial lid attachment it is interaction between the lens edge and the eyelids (rather than the cornea) that seems to determine comfort. Rounding of the anterior rather than the posterior edge seems to be the important factor.
Centre thickness
Modern lenses, because of their material properties and thin design, tend to flex, especially in low minus-powered lenses. In general, flexure increases with Dk and with the degree of toricity of the cornea the lens is sitting on. In general, system lenses take care of this for you. Once corneal astigmatism gets to about 2.00D a further 0.02mm is needed, so if you are fitting an astigmatic cornea with a spherical lens you might need to order something a bit thicker. This will, of course, compromise the oxygen transmission a little.
Back Vertex Power
The power of the contact lens required would normally be calculated from the spectacle prescription corrected for vertex distance but must take the power of the tear lens between the contact lens and cornea into consideration. If the lens is in perfect alignment with the central cornea, it follows that the tear lens will have zero dioptric power, and over-refraction is rather a good way to measure the degree of alignment. A lens which is steeper than the cornea will give rise to a tear lens of positive power, and a flat lens will create a negative tear lens. The power of the tear lens can be calculated precisely, but for lenses fitted fairly close to alignment this is unnecessary. A simple rule of thumb exists:
- For every 0.05mm that the BOZR is steeper than K, the tear lens power increases by +0.25D.
Therefore, you must counter this by adding –0.25D to the power of the contact lens. Obviously, if the contact lens is flat by 0.05mm, an extra –0.25 is added to the power of the tear lens, and the power of the lens ordered must be increased by +0.25D.
Example 1. A patient has a spectacle prescription of –5.00DS at a back vertex distance of 10mm. His K readings are 7.80mm in all meridians, but we have elected to fit him with a lens with a BOZD of 7.75mm. The first step is to adjust the spectacle lens power to account for the fact that the contact lens is sitting on the eye. This can be calculated using the formula;
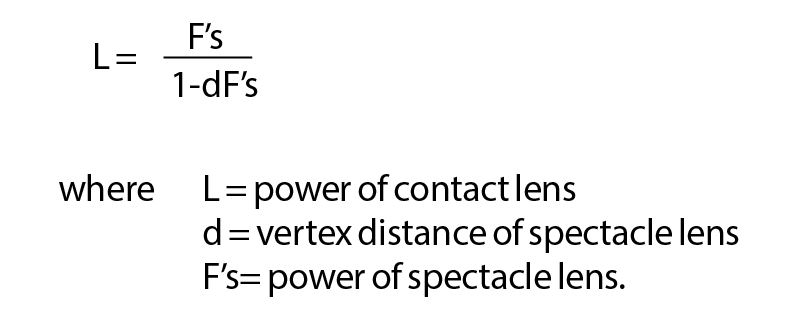
A spectacle lens at 10mm BVD has an effective power in the corneal plane of –4.75D, so this is the power we need for the contact lens. The lens is 0.05mm steeper than K, so the liquid lens will have a power of +0.25D. To counter this, we need to add –0.25D to the contact lens power, which takes us back to –5.00D. This is the power we will order.
If we decide that the 7.75 base curve looks a bit steep, we might decide to order a flatter lens next time. Suppose we want to order a BOZR of 7.85 this time. This is 2 x 0.05mm flatter than the previous lens, so we will create a tear lens with an extra –0.50D. We need to modify the power of the lens we order by +0.50, so we will order –4.50D.
Binocular considerations
Myopes are likely to be exophoric, particularly at near fixation distances. If they wear their spectacles for near visual tasks, they will benefit from a certain amount of base-in prism at near, as the spectacles will be centred for distance. The loss of this base-in prism may result in decompensation of their near ocular motor balance, variable vision, asthenopic symptoms or even diplopia. In such cases, a slight over-correction of their myopia can sometimes be beneficial, as the extra accommodation stimulated will also induce accommodative convergence.
With a normal accommodative convergence/accommodation (AC/A) ratio of around 4 even –0.25D can significantly alter the oculomotor balance without overloading accommodation itself. Accommodative demand is higher for a myope in contact lenses than it is in spectacles. If the patient habitually reads without spectacles, as many low myopes do, they may initially struggle to cope with the extra accommodative demand that correction of their myopia brings. For these patients, over-correction is not appropriate. Hyperopic patients often find near vision easier with contact lenses, as their accommodative and convergence demands are less. Practitioners should also beware the hyperope with a significant latent element, as their latent element sometimes seems to become manifest shortly after contact lens fitting.
Markings
It used to be common to see lenses marked ‘R’ and ‘L’ and some lenses even had the BOZR and TD printed on them as well. This is wonderful when doing aftercare, especially if you did not fit the patient. However, engravings do tend to assist the formation of deposits and they may weaken a lens mechanically. A spate of RGP lenses splitting in line with the vertical part of the R and L led to many labs adopting a simpler method of discrimination between the two, and most lenses now have only a small dot on one lens, usually the right one. One consequence of this is that many patients, particularly those in early presbyopia, have no idea which lens is which, and may turn up for aftercare appointments with either lens in either eye, or two of the same.
Tints
Some standard lenses come with a handling tint; this is intended to assist the detection of dropped lenses. The concept works well when white bathroom suites are in fashion but less so when the height of lavatorial elegance comes in avocado or tasteful beige. In any case the handling tint is rarely an option and is generally a standard feature of a particular lens. Similarly, many lenses have a UV inhibitor incorporated in the lens polymer and occasionally this is offered as an optional extra.
Summary
To order empirically, or to select from a trial set.
For a cornea with low toricity:
- TD should be large (9.60mm) unless there are good reasons for it not to be.
- BOZD should be the same as flattest K or slightly flatter. Keratometers vary owing to their different mire separation so get to know your instrument and allow for it.
- Edge lift should be standard, unless you know the patient isn’t.
- The lens edge needs to be well rounded or to have a well-rounded front edge.
- Centre thickness should be standard, unless you are fitting a spherical lens on a cornea with significant astigmatism. In this case add 0.02 to the standard thickness. Manufacturers will usually allow for the flexibility of the lens material in setting their standard thickness.
- Power should be the spectacle correction (spherical equivalent) adjusted for vertex distance and the tear lens, unless you are trying something clever to help oculomotor balance.
Andy Franklin is an optometrist specialised in contact lens practice based in the south-west.
