PLEASE NOTE: THIS VERSION OF THE EXERCISE IS ONLY APPROVED FOR CONTACT LENS OPTICIANS. IF YOU ARE AN AN OPTOMETRIST, DISPENSING OPTICIAN OR THERAPEUTIC OPTOMETRIST, PLEASE TAKE EXERCISE C61401)
This series of articles aims to provide an overview of the most commonly presenting cases of red eyes in primary care and will serve as a useful reference guide for the consulting room.
Over the last couple of years there has been an increase in the number of optometrists dealing with red eye diagnosis and management. There are several reasons for this. Firstly, with an independent prescribing qualification, optometrists are now able to treat a wider range of conditions. This has led to enhanced roles both in community practice and in hospital. Secondly there has been a rapid growth in MECs/PEARs type schemes being set up to enable optometrists, and now contact lens opticians, to manage more acute conditions in the community.
When dealing with these type of eye conditions it is important to work within your competence and recognise what you can and cannot manage. We will discuss some common presentations, management options and look at some pit falls to avoid. It is not an exhaustive list and some of the less common presentations are not included in this article.
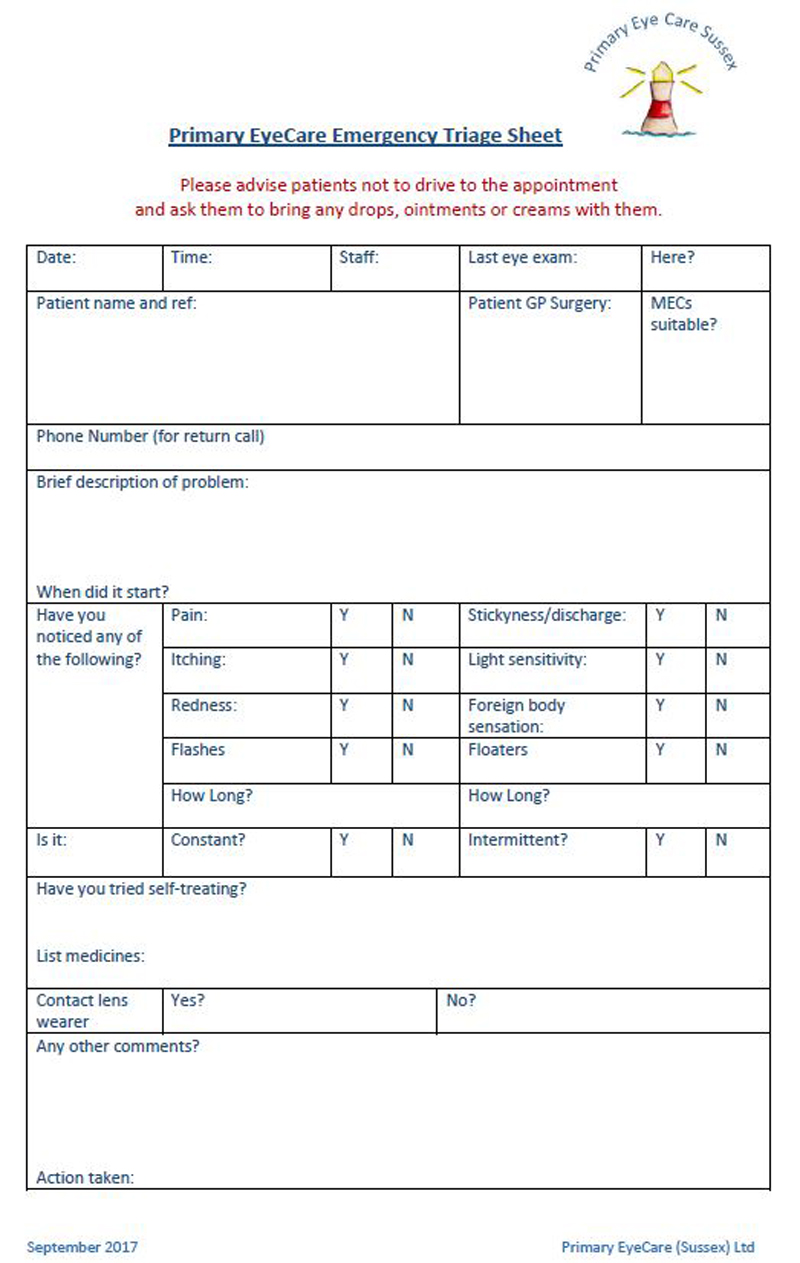
When a patient presents with an acute problem it can sometimes be difficult to decide how urgently they should be seen. The optometrist is not always the first person the patient will speak to. With this in mind there are several very good triage forms available for support staff to use and then pass on to the optometrist who can then decide on an appropriate timescale. One is shown in figure 1 and can be downloaded from https://pecsouthern.org.uk/wp-content/uploads/sites/132/2017/09/170925-PEC-Triage-Sheet.pdf.
Figure 1 Example of triage documentation for community optometry
From a practitioner point of view, however, it is always important to think about why you are asking the patient the questions you are. Is it just a checklist to work through or are you trying to gain valuable information that will help you come to a diagnosis.
The first thing to do is to work out how serious the condition is and how quickly you need to see the patient.
In the case of a red eye there are five vital questions to ask:
- When did this happen?
- How is the vision?
- Is it painful?
- Is there any photophobia?
- Is there any discharge?
Once this has been established good follow up questions are:
- Is one or both eyes affected?
- Is it constant or intermittent?
- If the patient has had anything like this before and, if so, what is the frequency of recurrence?
- Are they a contact lens wearer?
- Are there any associated symptoms or systemic conditions?
- Is there anything which appears to exacerbate or relieve the condition?
From an examination point of view the following would be recommended:
- Always check vision/VA
- Look at pupils and assess pupil reactions
- Look at the pattern of redness
- Carefully examine the conjunctiva, including lid eversion
- Thorough corneal slit lamp examination
- Anterior chamber (A/C) examination with appropriate illumination and magnification.
Our careful questioning and examination will help to differentiate between the various causes of red eye. Essentially, we need to know the underlying cause so we can treat it.
The main ones associated with red eye include:
- Infection
- Inflammation
- Trauma
- Degeneration
By the time this is complete, hopefully we will have an idea of what is going on and be able to formulate a management plan.
The various common presentations of red eye have been split into painless red eye and painful red eye. The rest of this article will deal with painless red eye. Each condition is listed in alphabetical order and described in terms of:
- Presentation
- Signs
- Symptoms
- Investigation
- Management and advice
Allergic conjunctivitis
This is usually seasonal but there many different possible causes (the College of Optometrists produces an excellent factsheet on this).
Some patients can be sensitive to more than one of these and as a result may suffer with symptoms throughout the year. They may also find it worse at particular times of the year.
It is a type 1 hypersensitivity reaction.
Presentation
- Red itchy eye
- May be associated with sneezing and runny nose.
Signs
- The eye is red
- Watery discharge
- Conjunctival chemosis of the bulbar conjunctiva
- Lid eversion may show papillae on the tarsal conjunctival
- Lids can also be swollen
- No corneal involvement
- It is usually bilateral but can be unilateral if the patient has come into contact with an allergen and then rubbed one eye
Symptoms
- The main symptom the patient complains of is itching and watery eyes
- Vision is usually unaffected
Investigation
- History of allergy/atopy, eg hay fever, asthma, eczema or any pet, food or drug allergies
- Consider family history of allergic disease
- Very commonly it is associated with sneezing and rhinitis
- Vision is usually unaffected
- Look for lid oedema
- Conjunctival chemosis
- Diffuse redness
- No corneal involvement
- May be papillae on lid eversion
Management and advice
There is a wide range of treatment approaches to allergic conjunctivitis, depending on the severity and whether you are IP qualified or not.
Simple remedies
- Cold compresses, instructions to try and stop rubbing eyes.
- Allergy avoidance (simple advice for patients who suffer with hay fever would include keeping windows closed during the hay fever season, not hanging washed bedding to dry outside, have a shower and wash hair before going to bed).
Eye drops
- Simple lubricating drops may have some effect by washing away allergens.
- Optometrists could also recommend the use of P medicine anti-allergy drops. These can be sold over the counter to patients in our practices and include:
- Topical mast cell stabilisers such as sodium cromoglycate (Opticrom) or lodoxamide (Alomide). These usually take about five days to take effect and the patient should be made aware of this.
- All optometrists can also sell or supply topical antihistamine drops such as Otrivine-antistin which will have more of an immediate effect.
IP optometrists have a greater range of eyedrops available to prescribe:
- Topical antihistamine, eg azelastine, emedastine or epinastine
- Topical antihistamine and mast cell stabiliser e.g. olopatadine or ketotifen
- Topical non-steroidal anti-inflammatory drugs (NSAIDs) such as diclofenac sodium
All the drops target different part of the inflammatory pathway, and this goes beyond the scope of this article
Bacterial conjunctivitis
This is one of the commonest eye conditions presenting to clinicians. There are various types of bacteria which can cause this, and some age groups, eg children and elderly more prone to this condition.
The eye normally has a good protective mechanism to remove bacteria. The eyelids form a physical barrier, the tears as well as have a flushing effect contain protective elements such as lysozyme and IgG and IgA and the conjunctiva contains specialised lymph tissue.
Presentation
- Sudden onset sticky gritty red eye
- One eye affected first then both
Signs
- Crusted eyelids
- Purulent or muco-purulent discharge
- Conjunctival hyperaemia
- Sometimes there may a mild chemosis and papillae of the palpebral conjunctiva
Symptoms
- Sudden onset red eye
- Grittiness
- Stickiness
- Usually bilateral, but may affect one eye first
- Vision usually unaffected, but may be slightly affected by discharge
Investigation
- Careful history to ascertain if the patient has been in contact with anyone else with this condition
- Detailed anterior segment examination including lid eversion to exclude any other possible causes
Management and advice
- Often this is self-limiting, resolving in about a week
- Lid hygiene helps to remove the lid crusting
- Topical antibiotic may help resolution
Eye drops which are available to all optometrists
There are several alternatives:
- Chloramphenicol eye drops or ointment
- Azithromycin eye drops
- Fusidic acid gel
Blepharitis
Blepharitis is frequently used to describe lid margin disease or inflammation of the lid margin. This is intended as a summary as blepharitis has been covered in detail in previous articles. It is included here for completeness.
It is usually divided into:
Anterior blepharitis
- Bacterial
- Seborrhoeic
Posterior blepharitis
- Meibomian gland dysfunction (MGD) – a chronic abnormality of the meibomian glands
Both of these types can coexist together. Demodex infestation has also been found to be associated with blepharitis
Presentation
- May be asymptomatic
- Varying degrees of ocular discomfort and or itching are reported
Signs
Bacterial anterior blepharitis
- Lash crusting (at base of lashes)
- Lid margin redness
- Recurrent styes (external hordeola)
- Corneal punctate erosions inferiorly
Seborrhoeic anterior blepharitis
- Oily or greasy deposits on lid margins
Demodex blepharitis
- Crusting of lashes with a clear sleeve around the base of the lash extending upwards on the lash.
Posterior blepharitis (MGD)
- Conjunctival hyperaemia
- Blocked meibomian glands foam along lower tear meniscus
- Irregular lower lid margins
- Lid notches
- Unstable tear film
- Inferior corneal stain
Symptoms
- Patients may be asymptomatic
- Discomfort
- Soreness
- Burning
- Itching
- Dry eye symptoms
Investigations
- Full anterior segment examination to exclude any other potential lid pathology
- Consider appearance of lid crusting
- Meibomian gland assessment (some practitioners find it useful to express the glands to gauge the quality and quantity of the secretions)
Management and advice
Whatever the cause for the anterior blepharitis lid hygiene is the main treatment regime
- Lid warming
- Lid massage
- Lid wipes
- There are various products available for this and practitioners can make their own choices
For more persistent or difficult to treat cases consider
- Topical antibiotic rubbed into the lid margin
- Longer term dietary advice, eg omega 3 intake vs omega 6
- IP optometrists may consider prescribing systemic antibiotics (for their anti-inflammatory effect) eg tetracyclines
Dry eye
Many patients present with symptoms of dry eyes. Although this has been included in painless red eye patients’ symptoms vary and can range from asymptomatic to painful.
Many of these will have tear film instability related to MGD and/or blepharitis. (See above for management).
However, it is important identify patients who may be suffering from true aqueous deficient dry eye due to an underlying systemic disease as this can be severe, painful and sight threatening.
In particular be suspicious of:
- Auto immune conditions such as Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus
- Lacrimal gland deficiency (could also be associated with sarcoidosis and lymphoma)
- Lacrimal gland obstruction (due to trachoma)
- Reflex hyposecretion (as a result of neurotrophic keratitis)
- Systemic drugs (there are many that may affect aqueous production including antihistamines, but these may be non-modifiable)
If you suspect a patient has any of these conditions they should be referred to an appropriate specialist, such as a rheumatologist for auto immune conditions as they may need systemic treatment for this.
Presentation
This is variable from chronic to acute onset.
Ocular discomfort which can vary greatly and can be described in many different ways by patients, but include terms such as:
- Burning
- Stinging
- Watering
- Grittiness
- Burry vision
Signs
- Blepharitis and MGD are often present
- Superficial conjunctival and corneal staining
- Reduced or variable tear prism height (also look for lid position anomalies)
- Tear break up time reduced with fluorescein
Symptoms
- Ocular irritation
- Foreign body sensation
- Grittiness
- Burning sensation
- Watery eye
- Variable vision
- Usually bilateral
Investigation
- Careful history to ask about possible underlying systemic causes
- Careful anterior segment investigation to rule out any other potential causes and to look for lid margin disease and lid malposition
- Assess tear quantity and quality (including tear prism height and tear break up time)
Management and advice
- Treat any blepharitis or MGD present (see above)
- Lubricating eye drops. If advising more frequent use (four to six times per day) consider preservative free (or soft vanishing preservatives)
- If there is suspected underlying systemic disease a referral to ophthalmology/rheumatology is indicated
- Note also check for lid position abnormalities which can disrupt the normal tear film, eg lower lid laxity and refer as appropriate
Episcleritis
This is another common condition. Usually it is self-limiting, but it can be recurrent.
It is most common in young women and, although it is not normally associated with systemic disease, it is thought that up to one third may be associated with one of the following:
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Inflammatory bowel disease
Presentation
- Sudden onset
- Red eye with mild discomfort
- Usually unilateral
- May have slight epiphora/watering
Signs
- Redness can be sectoral or diffuse (simple episcleritis, which accounts for 80% of cases)
- Can also be seen as slightly raised with injection (nodular episcleritis which accounts for 20% of cases). This type will have a greater foreign body sensation
- The anterior chamber is usually quiet
- There is no effect on the cornea
Symptoms
- Sudden onset of mild discomfort
- Occasionally tearing
- The vision is unaffected
Investigation
- Careful history to ask about possible systemic involvement
- Detailed anterior segment examination to exclude other possible causes
- The hyperaemia is superficial and blanches with a topical vasoconstrictor (phenylephrine 10%)
Management and advice
- Normally just reassurance that this is self-limiting
- Cold compresses can help give symptomatic relief
- Lubricating drops can also be recommended for discomfort
- IP optometrists can treat more severe cases with a mild topical steroid, eg fluorometholone. Evidence for using a topical NSAID is inconsistent
Subconjunctival haemorrhage
This is perhaps one of the common presentations of a red eye in primary care. Patients are usually concerned about its sudden onset, though they are usually unaware it has happened – it has been pointed out to them by a family member or friend. For the most part it is innocuous, but there are several things to consider when dealing with this.
Presentation
- Sudden onset painless red eye
Signs
- The redness is usually localised
- Normally inferiorly
- Usually unilateral
Symptoms
- Usually this is asymptomatic
- Sometimes some minor discomfort
- Vison is unaffected
Investigation
- History is important to help differentiate potential causes.
- High blood pressure: how well is it controlled, and when was it last checked?
- Is the patient on blood thinners? (aspirin, warfarin, rivaroxaban, clopidogrel) If the patient is taking warfarin, you could ask about their INR level and if it has been checked lately.
- Is the patient diabetic?
- Any recent trauma? Do not forget contact lens-related trauma too.
- Has the patient been straining, heavy lifting, coughing, vomiting or sneezing recently?
- Is this a recurrent problem?
Examination
- Vision is unaffected
- There is no discharge
- Look for unexplained skin bruising which may be associated with a clotting disorder
- If you have this facility in your practice, measure blood pressure
- Look for a posterior limiting border to the haemorrhage. If this is not seen then it may be due to an intracranial haemorrhage, and this is life threatening. This can happen in a skull fracture
- Also look for raised lesions as this can sometimes be confused with rare conditions such as Kaposi’s sarcoma or lymphoma with secondary haemorrhage (‘salmon patch’)
- Haemorrhagic conjunctivitis – this is a rare viral conjunctivitis which is bilateral and causes multiple small haemorrhages
Management and advice
- Normally the patient can be reassured and advised this is harmless and self-limiting
- Should resolve in five to 10 days.
- Cold compresses are sometimes useful to aid relief of any mild discomfort
- As with all of the conditions we will be considering the patient should be advised to return for more advice if the condition is not improving or resolving
- If you are concerned about systemic causes/medication in these cases, then a referral to the GP to investigate this further would be appropriate
- If you are suspicious of a skull fracture or other cause of intracranial haemorrhage, then an emergency referral is indicated
Viral conjunctivitis
This is a very common type of conjunctivitis, and it is extremely contagious.
Presentation
- Sudden onset
- Red gritty watery eye
- Possible slight reduction in vision
- One eye effected first then second eye, but to a lesser degree
Signs
- Conjunctival hyperaemia
- Lid eversion shows follicles in upper and lower fornices
- Sometimes the patient will have tender lymph nodes (pre-auricular lymph nodes just in front of the ears)
- There may be small epithelial lesions initially
- Later these may be sub epithelial
Symptoms
- Redness
- Gritty burning sensation
- Watery eye
- Eyelids sometimes stick together overnight
- Starts in one eye and progresses to the other eye
- First eye usually more affected
- If there is corneal involvement the vision will be reduced.
Investigation
- Detailed history: often contagious and contact with another affected person may be revealed or history of recent upper respiratory tract infection
- Look for swollen pre-auricular lymph nodes
- Careful anterior segment examination to look for:
- Lid swelling
- Lid eversion to look for follicles on the palpebral conjunctiva
- Conjunctiva to check pattern of redness
- Cornea to look for sub epithelial infiltrates (which do not stain with fluorescein)
Management and advice
- As this is a contagious condition take care to wash your hands before and after seeing these patients, as well as cleaning/disinfecting all instruments
- Normally self-limiting in one to two weeks
- Cold compresses help to relieve symptoms
- If patient wears contact lenses discontinue wear until completely resolved
Treatment
- Lubricating eyedrops and ointments may help with symptoms
- There are no effective antiviral agents and antibiotics are ineffective
- Normally it is just a case of reassuring patients and this should self-resolve
This concludes part 1 of the series. Parts 2 and 3 will deal with painful red eye.
Colin Davidson is an independent prescribing optometrist based in Sussex.
Clinical management guidelines can be downloaded directly or as an app from the College of Optometrists’ website
- Optician will be running a VRICS CET exercise at the end of this series.
