This series of articles aims to provide an overview of the most commonly presenting cases of red eyes in primary care and will serve as a useful reference guide for the consulting room. It is hoped this will help support practices involved in MECS schemes.
Overview
When dealing with these type of eye conditions it is important to work within your competence and recognise what you can and cannot manage. We will discuss some common presentations, management options and look at some pit falls to avoid. It is not an exhaustive list and some of the less common presentations are not included in this article.
When a patient presents with an acute problem it can sometimes be difficult to decide how urgently they should be seen. The optometrist is not always the first person the patient will speak to. With this in mind there are several very good triage forms available for support staff to use and then pass on to the optometrist who can then decide on an appropriate timescale. One is may be downloaded from here: https://pecsouthern.org.uk/wp-content/uploads/sites/132/2017/09/170925-PEC-Triage-Sheet.pdf.
From a practitioner point of view however, it is always important to think about why you are asking the patient the questions you are. Is it a checklist to work through or are you trying to gain valuable information which will help you come to a diagnosis?
The first thing to do is to work out how serious the condition is and how quickly you need to see the patient. In the case of a red eye there are five key questions to ask:
- When did this happen?
- How is the vision?
- Is it painful?
- Is there any photophobia?
- Is there any discharge?
Once this has been established good follow up questions include:
- Is one or are both eyes affected?
- Is it constant or intermittent?
- Has the patient had anything like this before and, if so, what is the frequency of recurrence?
- Are they a contact lens wearer?
- Are there any associated symptoms or systemic conditions?
- Is there anything which appears to exacerbate or relieve the condition?
From an examination point of view the following would be recommended:
- Always check vision/visual acuity
- Look at pupils and assess pupil reactions
- Look at the pattern or distribution of the redness
- Carefully examine the conjunctiva, including lid eversion to view palpebral conjunctiva
- Undertake a thorough corneal slit lamp examination
- Assess the anterior chamber (A/C) examination with appropriate illumination and magnification
Careful questioning and examination will help to differentiate between the potential causes of red eye. Essentially, we need to know the underlying cause so we can treat it. The main underlying causes of red eye to be identified are:
- Infection
- Inflammation
- Trauma
- Degeneration
By the time this approach is completed we will hopefully have an idea of what is going on and be able to formulate a management plan. The various common presentations of red eye discussed in this series have been split into painless red eye (see Optician 12.10.18) and painful red eye. Each condition is listed in alphabetical order and described in terms of:

In part 1 of this series we introduced red eye investigation and management, discussing the use of triage forms and ideal questions to incorporate into our history and symptoms. We then covered the presentation, investigation and management of some of the more common presentations of painless red eye. Part 2 will cover the first part of painful red eye presentations. As before these are presented in alphabetical order.
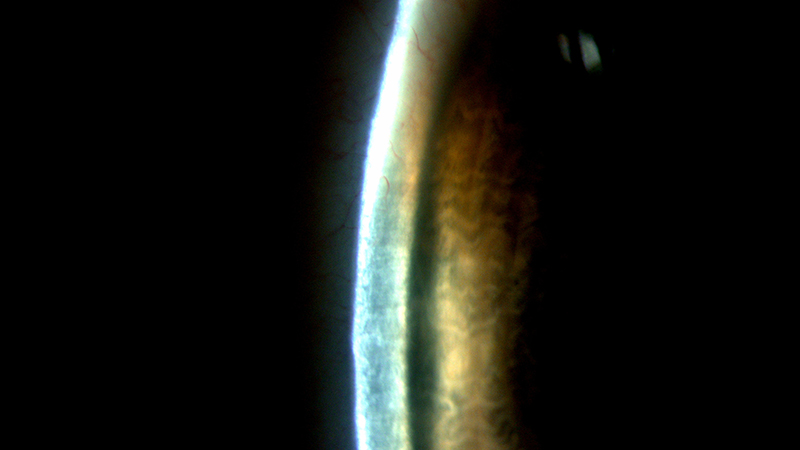
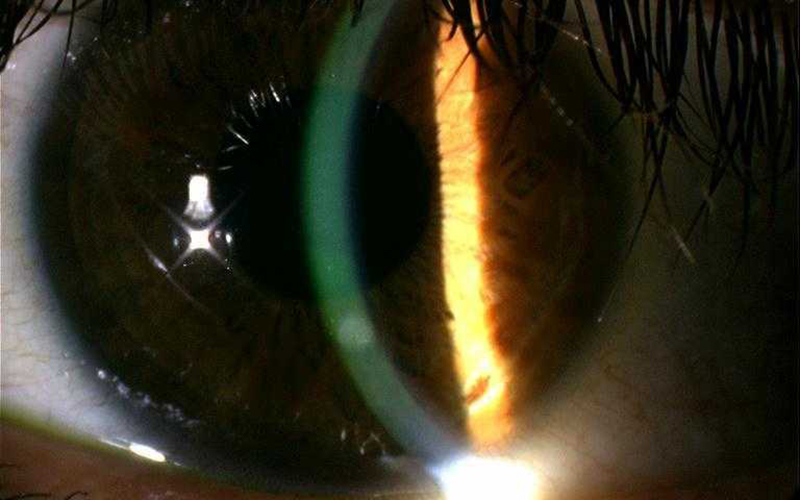
Figure 1: A narrow van Herrick graded angle
Angle Closure Glaucoma
Primary angle closure occurs when the anterior chamber angle closes. This obstructs aqueous outflow, causing IOP to rise rapidly. The main mechanisms causing it are as follows:
Anatomical
- Shallow anterior chamber (figures 1 and 2) which is more common in females
- Large crystalline lens (with increasing age or developing cataract)
- Short axial length (hypermetropia)
- Small corneal diameter
- Ethnicity
- Family history
- Plateau iris syndrome
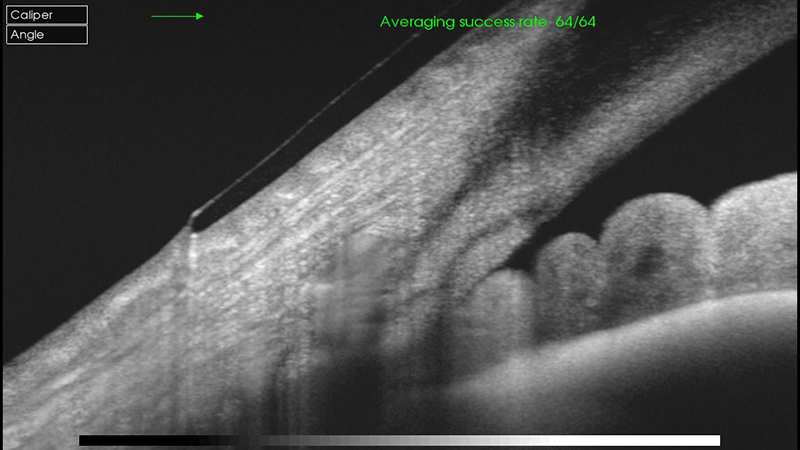
Figure 2: Anterior OCT of a narrow angle despite appearing sufficiently wide on van Herrick
Iatrogenic
- Drug-induced which can be both topical and systemic
- Adrenergic agents
- Anticholinergic effects of drugs tricyclic antidepressants
- Drugs causing ciliary body oedema such as sulphonamides
- Surgery-induced, such as after vitreoretinal surgery when intraocular gas has been introduced
- Sudden onset very painful red eye
- Usually unilateral

- Circumcorneal redness
- Hazy cornea
- Shallow anterior chamber
- Fixed mid dilated pupil
- High intraocular pressure (often in the range of 40 to 80mmHg)
- Anterior chamber cells and flare
- Grey white anterior subcapsular lens opacities
- Oedematous optic disc

- Sudden drop in vision
- Ocular pain which may be severe
- Redness of the eye
- Nausea and vomiting
- Note — angle closure may be asymptomatic in Asians

- Careful questioning as family history is common
- Anterior segment examination to exclude other causes
- Gonioscopy if competent and confident

- This is an ocular emergency and patients should be referred straight to ophthalmology
- IP optometrists may consider giving oral acetazolamide (Diamox 500mg) if there are no contraindications and the patient is not vomiting
- Once the patient is at hospital this will be treated with
- Topical miotics (pilocarpine 2 or 4%)
- Systemic medication (acetazolomide, orally or intravenously)
- Topical antihypertensives (timolol, dorzolomide, brimonidine)
Chemical trauma
Treat first and ask questions later
It is estimated 10% of emergencies treated in hospital are chemical injuries. Note – alkalis penetrate the eye easily by liquefactive necrosis while, by contrast, acids cause coagulative necrosis which slows down penetration.
- Sudden onset painful red eye
- May be one or both eyes
- History of contact with one of the following
- Alkalis such as household cleaners, cement, plaster
- Acid such as car battery acid, wart treatments, limescale removal fluids
- Detergents
- Solvents
- Fixatives
- Contact lens solutions
- Pepper spray
- Superglue

- Redness
- Possible burns to lids and face
- Particulate matter under the eyelids
- Conjunctival chemosis and hyperaemia
- Blanching of limbal blood vessels (number of clock hours of limbal involvement predicts the prognosis)
- Corneal defects
- Corneal oedema
- Corneal opacification

- Pain
- Lacrimation
- Reduced vision

- Ascertain the cause of the trauma
- Treat first and ask questions later
- Measure IOP as it may be raised
- Irrigate the eyes, preferably with saline (figure 3), but tap water if not available for up to 30 minutes
- If possible check pH and stop irrigation when returns to normal, Then re check pH 30 minutes after completion of irrigation.
- Remove any particulate matter
- Measure VA
- If it is severe refer immediately
Figure 3: Single use preservative-free saline for irrigation purposes
Contact Lens Peripheral Ulcer (CLPU) Or Contact Lens Associated Infiltrative Keratitis
This is an inflammatory condition and is thought to be a response to the presence of bacterial antigens. Although it is related to bacteria, there is not any progression to infection.
- Mild discomfort, red watery eye
- Associated with contact lens wear

- Usually unilateral
- Mild epiphora
- No lid oedema
- Mild conjunctival hyperaemia
- Small peripheral anterior stromal infiltrate (figure 4)
- Usually less than 1mm
- May be single or multiple
- Anterior chamber quiet (although there may be mild inflammation present)

- The eye is slightly watery
- Moderate redness
- Mild foreign body sensation
- Mild photophobia
- However, some patients may be asymptomatic

- Full anterior segment examination to exclude other causes
- Meticulous follow up is required – remember big ulcers start as small ulcers
- Ask patient to temporarily discontinue contact lens wear
- It is important to monitor over the first 24 hrs
- If concerned about the possibility of microbial keratitis, ask patient to return later the same day or early next day (always give SOS advice)
- If there is any doubt about the diagnosis refer to ophthalmology as an emergency
- Most signs and symptoms will resolve over 48 hours, although the infiltrate may take several weeks
- Ocular lubricants are useful to ease discomfort. No other treatment is required unless there is associated blepharitis
Figure 4: Small peripheral anterior stromal infiltrate
Corneal Abrasion
This is simply a superficial corneal wound. It can be due to:
- Sub tarsal foreign body (always remember to evert the eyelid)
- Trauma (commonly from a finger nail – figure 5)
- Contact lens related trauma
- Trichiasis (look for entropion with which it is commonly associated)
Despite being superficial this can be very painful. Several key factors to look out for are:
- Epithelial basement membrane dystrophies. The epithelium is more prone to damage.
- A history of diabetes
- Neurotrophic keratitis
- Sudden onset painful red eye
- Usually unilateral

- Lid swelling and redness
- Conjunctival redness
- Epithelial defect in the cornea
- Underlying corneal oedema
- Visual loss
- Possible anterior uveitis secondary to the injury

- Pain – can vary greatly
- Blepharospasm
- Photophobia
- Lacrimation
- Redness
- Often history of trauma

- Careful history to establish any possible cause of the abrasion. Also ask about diabetes as the injury may be slower to heal
- Exclude chemical injury or penetrating foreign body (Seidel’s test is useful for this – the dilution of instilled fluorescein by the leakage of aqueous humour through a full thickness penetrating wound)
- Look for signs of recurrent erosion syndrome or epithelial basement membrane dystrophy
- There may be a risk of bacterial invasion
- Check for secondary anterior chamber activity
- It may be necessary to instil topical anaesthetic to aid examination
- Aspirin, paracetamol or ibuprofen tablets can help ease pain in the first 24 hours
- Lubricating drops to ease discomfort
- If there is a risk of infection, topical antibiotic can be used such as chloramphenicol
- Mydriatic drops can help to ease discomfort by stopping pupil spasm
- IP optometrists can prescribe a topical non-steroidal anti-inflammatory drug (NSAID) for both its anti-inflammatory and analgesic properties
Corneal Foreign Body
The common causes of superficial foreign bodies are:
- Wind-blown dust or grit
- Do-it-yourself tasks
- Gardening
- High velocity projectiles from hammering and grinding are very dangerous as they can penetrate or perforate the globe.
They rarely cause infection. Microbial keratitis is more common with organic stone or ceramic foreign bodies. Vegetative foreign bodies carry a risk of fungal keratitis.
- Sudden onset painful red eye

- Normally unilateral
- Injection
- Rust ring forms within 48 hours
- Possible anterior uveitis

- Photophobia
- Pain
- Lacrimation
- Blurred vision
- History of foreign body

- Measure VA before and after removal
- Assess pupil responses
- Examine anterior chamber for signs of activity
- If a penetrating injury is suspected from the history carry out a dilated fundus examination
- Always check for multiple foreign bodies
- Saline rinse may dislodge if superficial
- If not instil anaesthetic:
- Conjunctival foreign bodies may be removed with a sterile cotton bud
- Corneal foreign bodies may also be removed with a cotton bud
- Some may need removal with a hypodermic needle (such as a 26 gauge)
- Always approach from the side
- An Alger brush can be used to remove a rust ring
- Topical antibiotic (such as chloramphenicol ointment) four times a day for five days
- Short term cycloplegia for comfort
- IP optometrists may prescribe topical NSAIDs for analgesia and anti-inflammatory properties such as diclofenac 0.1%
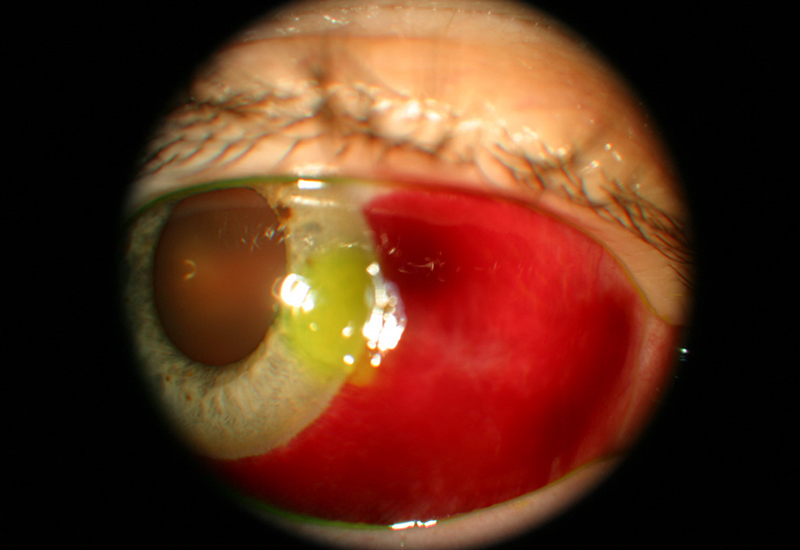
Figure 5: Corneal abrasion due to a fingernail. Note the presence of a subconjunctival haemorrhage too
Herpes Simplex Keratitis
This is a common virus, with up to 90% of the population in the UK being seropositive for it, though the virus is usually latent. The primary infection occurs in childhood (usually accompanied by a brief period of general malaise) and the virus lies dormant in the trigeminal ganglion. Reactivation of the virus can cause ocular infection. This may result in recurrent keratitis which may be:
- Epithelial
- Stromal
- Endothelial
- Neurotrophic
There may also be intraocular involvement which might include anterior uveitis and retinitis. The most common form is epithelial keratitis which will be discussed here.
- This may be variable but usually an acute onset unilateral red eye with pain and reduced vision

- In the early stages, superficial punctate keratitis may be seen
- This progresses to form a dendritic ulcer which may be single or multiple and have terminal end bulbs (not seen in pseudodendrites)
- If enlargement continues, a geographic ulcer may develop

- Patient reports discomfort which can range from foreign body sensation to pain
- Blurred vison
- Epiphora
- Redness
- Usually unilateral, but may be bilateral in atopic patients

- Full anterior segment examination to exclude other causes
- Posterior chamber examination to check for herpetic retinitis
- Diagnosis is usually made on clinical features
- If it is uncertain, swab for viral or other microbial causes (Acanthamoeba keratitis may be misdiagnosed as Herpes simplex keratitis)
- Both conjunctival and corneal swabs may be taken
- Non-IP optometrists should refer as an emergency to ophthalmology
- IP optometrists may treat recurrent epithelial disease thus:
- Treatment with topical antiviral such as acyclovir or ganciclovir to be used five times daily for one week
- Meticulous follow up and appropriate SOS advice is important as this is a potentially sight threatening disease
- In recurrent attacks oral antivirals may be considered

Figure 6: An Alger brush, useful for removal of a corneal rust ring
Herpes Zoster Ophthalmicus
The primary infection of Varicella Zoster virus (VZV) results in chickenpox. Reactivation results in shingles. The ophthalmic branch of the trigeminal is involved in 15% of shingles cases resulting in Herpes Zoster Ophthalmicus (HZO).
- It mainly affects patients in their 50s and 60s, but can occur at any age and may be linked to immune compromised patients
- Unilateral painful rash often respecting a vertical midline on the face

- Skin:
- Unilateral red rash on forehead and upper eyelid. Crusting developing after two to three weeks.
- Swelling around lid and orbit which may cause the eyelids to close
- Hutchinson’s sign is involvement of the tip of the nose. This indicates nasociliary nerve involvement and often signifies ocular complications are likely
- Ocular
- Mucopurulent conjunctivitis
- Episcleritis
- Scleritis
- Keratitis
- Epithelial: consisting of superficial punctate keratitis and pseudo dendrites
- Stromal: nummular keratitis with anterior stromal deposits
- Disciform: endotheliitis with a disc of corneal oedema
- Neurotrophic: Corneal nerve damage can cause a persistent epithelial defect

- General malaise
- Fever
- Headache
- Pain
- Altered sensation on one side of forehead
- Rash appears any time between 1 day to one week later

- Careful anterior segment examination to exclude other causes
- Posterior segment examination to check for secondary complications (see below)
- If skin lesions present, refer same day to GP to commence systemic antiviral treatment
- If epithelial involvement and patient is being co-managed by the GP, then optometrists can manage to resolution with topical lubricants. Aspirin, paracetamol or non-steroidal anti-inflammatory tablets can be used for pain relief. Be careful to check for any contraindications to these
- If deeper cornea is involved, refer to ophthalmology within 1 week
- The patient may be advised to
- Rest
- Ensure they have a good diet
- Take plenty of fluids, and
- Avoid contact with those who are elderly or pregnant, babies and children who haven’t been exposed to VZV, or people who are immunodeficient
- Systemic antivirals such as acyclovir, famciclovir and valaciclovir are used, possibly as well as topical steroids
- In severe cases, tarsorrhaphy is used for neurotrophic patients
- There are other potential sight threatening complications (secondary glaucoma, anterior uveitis, retinitis, choroiditis, optic neuritis) as well as neurological complications (cranial nerve palsies, encephalitis) so a low threshold for referral is sensible
- Complications can sometime occur months or years after the acute phase
Colin Davidson is an independent prescriber optometrist based in Sussex.
Further Reading
Unless otherwise stated references for this article have been taken from: The College of Optometrists Clinical Management Guidelines found at https://www.college-optometrists.org/guidance/clinical-management-guidelines.html; Oxford Handbook of Ophthalmology 3rd Edition Alastair Denniston, Philip Murray; Moorfields Manual of Ophthalmology Timothy L Jackson; Manual of Eye Emergencies – Diagnosis and Management Lennox A Webb