Thanks to media advertising, consumers are generally aware of laser vision correction, but they may not be so familiar with alternatives, such as refractive lens exchange (RLE) and phakic intraocular lens implantation (pIOL). Which begs the question – what is the best way to counsel a patient about these lens-based procedures, particularly one who has his or her mind made up about laser vision correction?
Several factors should come into play in this discussion, such as the patient’s age, axial length, type and magnitude of refractive error, anterior segment consideration, endothelial cell counts, as well as what the patient wants.1
It is always paramount to evaluate the needs and wants of the patient. Understanding the outcomes, potential complications and having realistic expectations will help the patient during all phases of the procedure. Patients need to understand their expected visual outcomes – they will often have a very high expectation, unrealistic even, of how their sight will be post-procedure. The best candidates for refractive surgery will enter pre-op consultations with an open mind and a clear understanding of the procedures and outcomes.
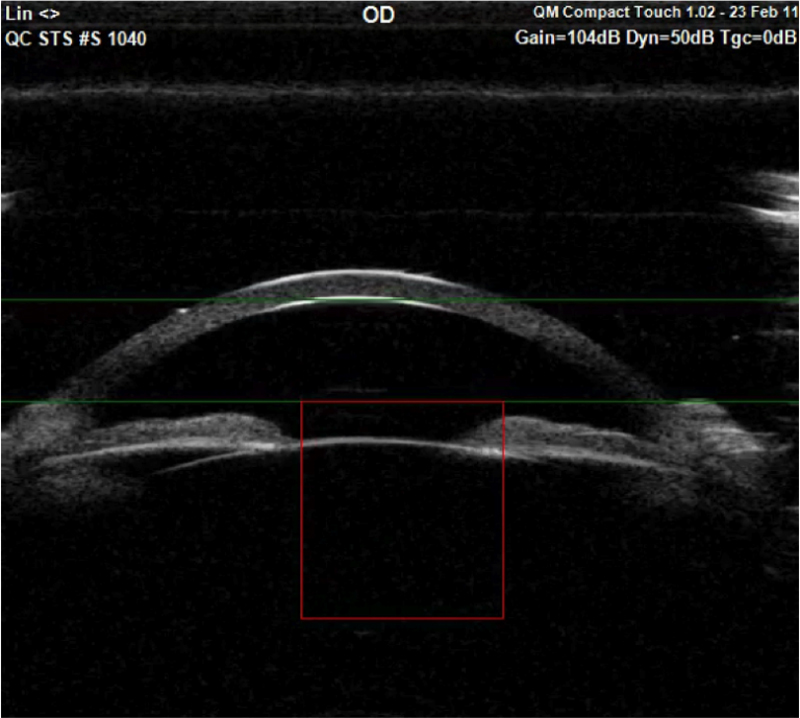
Figure 1 An implantable lens in situ as viewed with wide-field anterior OCT
 The patient needs to be able to give informed consent and this requires the doctor to give valid and true information, answer questions honestly and to detail the risks and benefits – then an informed choice can be made by the patient.
The patient needs to be able to give informed consent and this requires the doctor to give valid and true information, answer questions honestly and to detail the risks and benefits – then an informed choice can be made by the patient.
‘A clear vision or understanding pre-operatively, might well lead to clear vision post operatively.’
Let us now consider refractive lens exchange (RLE), then phakic IOLs in more detail.
Refractive Lens Exchange
RLE is an effective, safe treatment for the correction of presbyopia, myopia and hyperopia, as well as astigmatism. An alternative to laser surgery, RLE results in excellent visual outcomes and may be a better option for hyperopic eyes than pIOLs.
The procedure
The procedure begins with pupil dilation. A clear gel is injected to protect delicate structures intra-operatively. An opening is created in the capsule with a hand-held tool or laser. Ultra-sonic energy and gentle suction breaks up and removes the eye’s natural crystalline lens and an IOL is inserted.2 The procedure takes approximately 15 minutes and each eye is done separately.
Advantages of RLE
- RLE provides greater depth of focus through the utilisation of multifocal and accommodative lenses1
- RLE can correct almost any degree of hyperopia
- Visual acuity is often better than LASIK and PRK outcomes in moderate to high hyperopia3
- RLE is a quick procedure taking only 15 minutes approximately per eye
Microincision cataract surgery introduction aids the safety profile of RLE. RLE causes loss of accommodation and therefore the procedure should be avoided in patients where their natural lens is functioning.3
The relative contraindications for RLE are:
- Patients younger than 50 years
- Axial length of more than 25mm
- No evidence of posterior vitreous detachment (PVD); presence of multiple peripheral vitreoretinal degenerative changes
- History of retinal detachment in the same or other eye
- Presence of myopic choroidal neovascularization/lacquer cracks
- Patients with unrealistic expectations of the outcome, who are unwilling to attend regular follow-up or to accept the inherent risks of surgery4
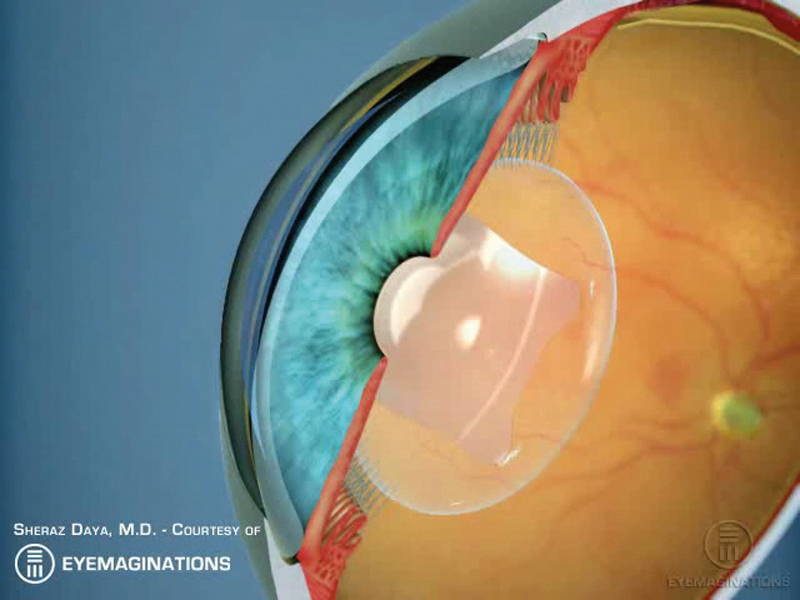
Figure 2 Phakic intraocular lens (courtesy of Eyemaginations)
Potential complications – the risks
Several studies indicate that RLE surgery considerably increases the risk of retinal detachment in myopes.5 The risk is higher in younger myopic eyes, (<50 years old). The incidence of retinal detachment after RLE ranges from 0% to 8 %.6 In hyperopic patients, retinal detachment is rarer.
The risk of late retinal detachment in high myopes has been widely documented.7 Whereas, with phakic lenses retinal detachment is less of an issue, for example, in a European multicentre study of the Artisan phakic IOL, retinal detachments occurred in just two eyes over an eight-year period.6
RLE can be a more invasive procedure than other laser type surgeries. There is a possible risk of:
- Raised intraocular pressure (IOL)
- Dislocated IOL
- Glare or halos from multifocal lens
- Potential intraocular infection (endophthalmitis)
- Glaucoma, cataract and posterior capsular opacification (PCO), are associated with RLE – PCO is a common post-operative complication for RLE
Phakic IOLs
Phakic IOLs include the following:
- Visian Implantable Collamer Lens (ICL; STAAR Surgical)
- The iris- fixated Artisan/Verisyse and Artiflex/Veriflex (Ophtec BV /Abbott Medical Optics Inc)
- The AcrySof Cachet (Alcon Laboratories Inc)
- The Visian ICL, the V4c with its 360-µm central hole, removes the need for iridotomies
The Visian ICL is a newly introduced posterior chamber phakic IOL, meaning it is positioned behind the iris and in front of the natural lens (figure 1). It received FDA approval in 2005 for correcting myopia ranging from -3.00 to -20.00 D. Made of a soft, biocompatible collagen copolymer and due to its flexibility, the lens can be folded during implantation, requiring only a small surgical incision.2
The Verisyse is an anterior chamber phakic IOL, meaning it is positioned in front of the iris. In 2004, the Verisyse phakic IOL received FDA approval for correcting moderate to severe near-sightedness within the range of -5.00 to -20.00 dioptres (D).2
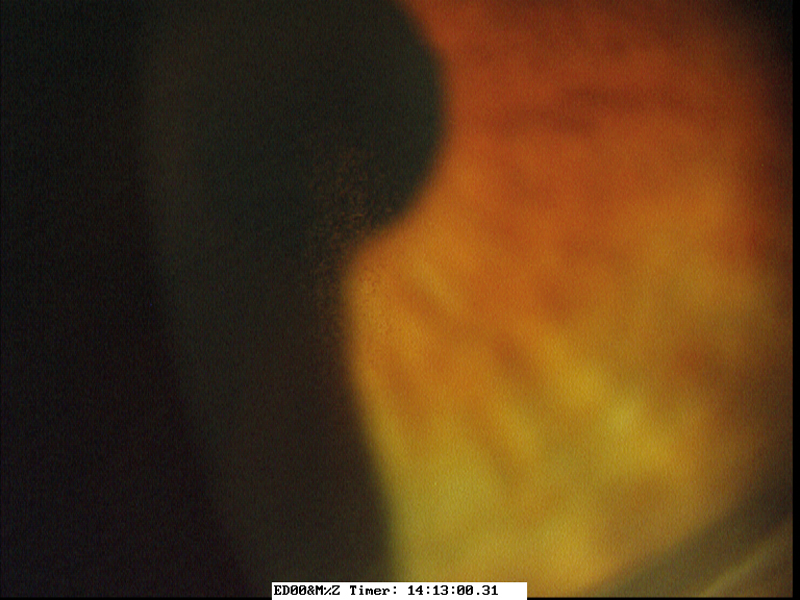
Figure 3 Pigment dispersion
The Verisyse lens is made of a rigid, medical-grade plastic polymethylmethacrylate, or PMMA. In Europe, it is approved and marketed under the trade name Artisan. There are foldable versions of the myopic lens which can be inserted through smaller incisions and known as Veriflex or Artiflex.2
Phakic IOLs are surgically placed between the cornea and the iris or just behind the iris, without removing the natural lens of the eye (figure 2).2
Advantages of pIOLs
- Rapid visual recovery
- A greater range of treatable ametropia including astigmatism to 6.00 DC
- Reversibility
- High predictability rates
- Stability
- Preservation of accommodation4
Potential risks
The main possible complications associated with phakic IOLs are:
- Pigment dispersion (figure 3)
- Cataract formation, glaucoma and inflammation
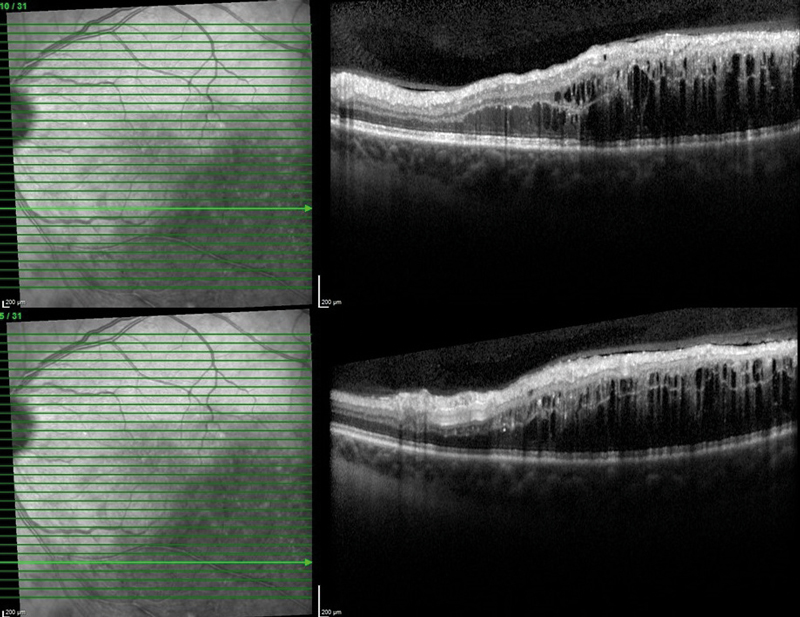
- Cystoid macular oedema (CMO) – CMO is a more common following RLE (figure 4)
- Endothelial cell loss – in phakic IOLs located in the anterior chamber
Selection Criteria in RLE and Phakic IOL implantation
Selection
This will depend on the patient’s needs and vision assessment, along with factors such as age. The author will not consider RLE in individuals under 50 years old, exceptions are made for patients who have high hyperopia (+4.00 DS and greater) and where the anterior chamber depth is shallow.1
Preoperative workup
This is extensive to ensure the correct choice for implantation. Preoperative assessment includes manifest and cycloplegic refraction, Snellen uncorrected and corrected distance, intermediate and near visual acuity, pupillometry, applanation tonometry, fundus evaluation, corneal topography, pachymetry and lens biometry preferably with partial coherence interferometry devices. A fundus evaluation is required to ensure an intact peripheral retina and to document the status of the macular and vitreous.1 Increasingly macular and retinal nerve fibre layer ocular coherence tomography is performed to objectively document the status of both macula and nerve and also the presence or not of a posterior vitreous detachment. If a phakic lens is going to be used, then specular microscopy to measure endothelial cell count, anterior chamber depth, and white-to-white measurements are also required.
Figure 4 Cystoid macular oedema viewed on OCT
Different types of lenses for implantation
The refractive models used in RLE to achieve multifocality through the use of diffractive, zonal refractive or extended depth of focus (EDOF) lenses usually provide proper far and intermediate vision; however, sometimes, near vision is not enough depending on the type of lens used. They are dependent on pupil dynamics and may create a reduction in contrast sensitivity, and cause halos or glare.8
The trifocal diffractive models are composed by diffractive concentric microstructures and reliably provide correction at distance, intermediate and near and depend on cortical adaptation which in a small sub-group of patients can take time. Contrast sensitivity may be a greater issue with diffractive models,8 however, on a practical level based on experience and patient feedback, this is not usually clinically significant.
In a retrospective study,9 phakic IOL implantation and RLE were compared in a group of highly myopic 30 to 50-year-old patients. RLE was performed in eyes with the anterior chamber shallower than 2.8mm or at the beginning of presbyopia, whereas phakic IOL was implanted in eyes with no recent visual acuity decrease or presbyopic refraction changes. At one-year follow-up, the results were similar in both groups.
In conclusion, phakic lens implantation in myopic patients of 30 to 50-year-olds was a more adequate refractive technique with lower risk of corrected distance visual acuity (CDVA) loss, and extraction of crystalline lens can be performed as a secondary procedure.
Conclusion
Where laser vision correction is not an option, both RLE and pIOLs are excellent choices and, depending on the age of the patient, may be a better option than laser surgery. The choice of procedure needs to be based on the balance of risks and benefits. Refractive lens exchange is a good option for hyperopes over the age of 50 and myopes with posterior vitreous detachments over the age of 55. Phakic lenses, an additive procedure is an excellent option for all suitable patients, whether myopic or hyperopic, under the age of 50.
The desired visual outcome is dependent on several post-operative considerations and decisions should be made on an individual basis after extensive assessments and informed consent has been obtained.
Many similarities exist between both pIOLs and RLE procedures, such as cost, recovery lengths and both procedures take approximately 15 to 20 minutes per eye. Post-operative regimes are similar in that eye drops are used for four to six weeks dependent on the case. Visual recovery in both procedures is fast – in a few days the patient should be able to see well enough. However, pIOLs provide better distance correction visual outcomes and at this time do not provide near-vision correction that RLE can provide.1
Future technology developments will no doubt present newer IOL models with sharper and more advanced visual outcomes, however, RLE and pIOLs currently stand tall among optical treatments.
Key Points
- Consider age, axial length, type and magnitude of refractive error, anterior segment configuration, ECC, and the patient’s desires
- Phakic IOLs are additive procedures and safe option in myopic eyes
- RLE is a better option in hyperopic eyes
- Always provide valid, realistic and detailed information for patients to make informed decisions
- Do not shy away from mentioning potential complications such as retinal detachment – the patient needs to have the whole picture and realistic expectations.
Sheraz Daya is a consultant ophthalmologist and medical director, Centre for Sight, East Grinstead.
References
- Nanavaty, MA, and Daya, SM. Refractive lens exchange versus phakic intraocular lenses. Curr Opin Ophthalmol. 2012 Jan;23(1):54-61. doi: 10.1097/ICU.0b013e32834cd5d1.
- Wachler, BB, Refractive Lens Exchange (Lens Replacement Surgery) All about vision.com, 2017. Available at: https://www.allaboutvision.com/visionsurgery/refractive-lens-exchange.htm Downloaded on 11/06/2018.
- Nanavaty, MA, and Daya, SM. Decision-Making: RLE Versus Phakic IOL. Cataract and Refractive Surgery Today Europe, 2012. Available at: https://crstodayeurope.com/articles/2012-oct/decision-making-rle-versus-phakic-iols/
- Srinivasan, B et al., Modern Phacoemulsification and Intraocular Lens Implantation (Refractive Lens Exchange) Is Safe and Effective in Treating High Myopia. Asia-Pacific Journal of Ophthalmology 2016; (5); 6, November/December 2016. Available at; https://pdfs.semanticscholar.org/0137/717c39916a4df03b686a01842c1bc091f97b.pdf
- Rosen, E. Risk management for rhegmatogenous retinal detachment following refractive lens exchange and phakic IOL implantation in myopic eyes. Journal of Cataract and Refractive Surgery, 2006; 32(5): 697–701. DOI: https://doi.org/10.1016/j.jcrs.2006.03.012
- Budo, c et al., Multicenter study of the Artisan phakic intraocular lens. Journal of Cataract and Refractive Surgery, 2000; 26, (8): 1163–1171.
- Fritch CD, Risk of retinal detachment in myopic eyes after intraocular lens implantation: a 7-year study. J Cataract Refract Surg. 1998; 24: 1357-1360.
- Liberdade SC, et al., Multifocal intraocular lenses: Types, outcomes, complications and how to solve them. Taiwan Journal of Ophthalmol. 2017 Oct-Dec; 7(4): 179–184. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5747227
- Arne JL. Phakic intraocular lens implantation versus clear lens extraction in highly myopic eyes of 30- to 50-year-old patients. J Cataract Refract Surg. 2004 Oct; 30(10):2092-6.
