This series of articles aims to provide an overview of the most commonly presenting cases of red eyes in primary care and will serve as a useful reference guide for the consulting room. It is hoped this will help support practices involved in MECS schemes.
Overview
When dealing with these type of eye conditions it is important to work within your competence and recognise what you can and canonot manage. We will discuss some common presentations, management options and look at some pit falls to avoid. It is not an exhaustive list and some of the less common presentations are not included in this article.
When a patient presents with an acute problem it can sometimes be difficult to decide how urgently they should be seen. The optometrist is not always the first person the patient will speak to. With this in mind there are several very good triage forms available for support staff to use and then pass on to the optometrist who can then decide on an appropriate timescale. One may be downloaded from: https://pecsouthern.org.uk/wp-content/uploads/sites/132/2017/09/170925-PEC-Triage-Sheet.pdf.
From a practitioner point of view however, it is always important to think about why you are asking the patient the questions you are. Is it just a checklist to work through or are you trying to gain valuable information which will help you with a diagnosis?
The first thing to do is to work out how serious the condition is and how quickly you need to see the patient. In the case of a red eye there are five key questions to ask:
- When did this happen?
- How is the vision?
- Is it painful?
- Is there any photophobia?
- Is there any discharge?
Once this has been established good follow up questions include:
- Is one or are both eyes affected?
- Is it constant or intermittent?
- Has the patient had anything like this before and, if so, what is the frequency of recurrence?
- Are they a contact lens wearer?
- Are there any associated symptoms or systemic conditions?
- Is there anything which appears to exacerbate or relieve the condition?
From an examination point of view the following would be recommended:
- Always check vision/visual acuity
- Look at pupils and assess pupil reactions
- Look at the pattern or distribution of the redness
- Carefully examine the conjunctiva, including lid eversion to view palpebral conjunctiva
- Undertake a thorough corneal slit lamp examination
- Assess the anterior chamber (A/C) examination with appropriate illumination and magnification
Careful questioning and examination will help to differentiate between the potential causes of red eye. Essentially, we need to know the underlying cause so we can treat it. The main underlying causes of red eye to be identified are:
- Infection
- Inflammation
- Trauma
- Degeneration
By the time this approach is completed we will hopefully have an idea of what is going on and be able to formulate a management plan. The various common presentations of red eye discussed in this series have been split into painless red eye (see Optician 12.10.18) and painful red eye. Each condition is listed in alphabetical order and described in terms of:
Presentation
Signs
Symptoms
Investigation
Management and advice
Ingrowing eyelashes
Patients with misdirection of the eyelashes often consult their optometrist with ocular irritation.
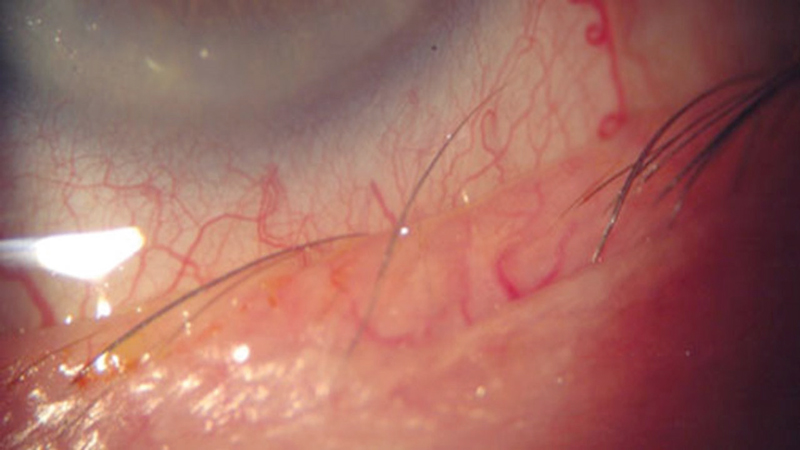
Figure 1 Ingrowing lash
Presentation
- Some patients are asymptomatic
- Gradual onset of redness and ocular discomfort more common
Signs
- Redness
- The lashes can be seen touching the ocular surface on slit lamp examination (figure 1)
- Corneal epithelial abrasion
- If the condition is longstanding there may also be pannus (figure 2) or corneal ulcer or infective keratitis
Figure 2 Pannus
Symptoms
- Sometimes patients are asymptomatic, but generally they complain of some or all of the following affecting one or both eyes:
- Discomfort
- Irritation
- Foreign body sensation
- Lacrimation
Investigation
- History to check if this is a recurrent problem
- Slit lamp examination of lids and lashes
- It can be secondary to several different conditions
- Misdirected lashes – lashes originate from the normal follicle, but are re-directed posteriorly. This can be due to scaring of the lid margin or lash follicle
- •Metaplastic lashes (congenital) or distichiasis, an extra row of lashes growing from meibomian gland orifices. This is an uncommon genetic abnormality
- •Metaplastic lashes (acquired), where lashes originate from an abnormal position. This is usually secondary to entropion or injury eg Stevens Johnson syndrome (figure 3), ocular cicatricial pemphigoid or chemical burn.
- Pseudotrichiasis due to marginal entropion normal lashes are directed posteriorly
Figure 3 Stevens Johnson syndrome
Management and advice
- Epilation can be performed, although the lashes tend to grow back and cause renewed symptoms in six to eight weeks (figure 4)
- Micropore tape can be used in cases of entropion
- Ocular lubricants help provide relief
- A bandage contact lens may also be useful to offer symptomatic relief
- In cases where the lash constantly regrows and causes symptoms the can be referred for possible
- Electrolysis
- Cryotherapy
- Argon laser
- Surgery for any underlying conditions, eg entropion
Figure 4 Tweezers used for epilation

Iritis
This is the most common form of uveitis and is thought to account for 75% of ocular inflammation. Optometrists who have an IP qualification may be more involved in managing this condition.
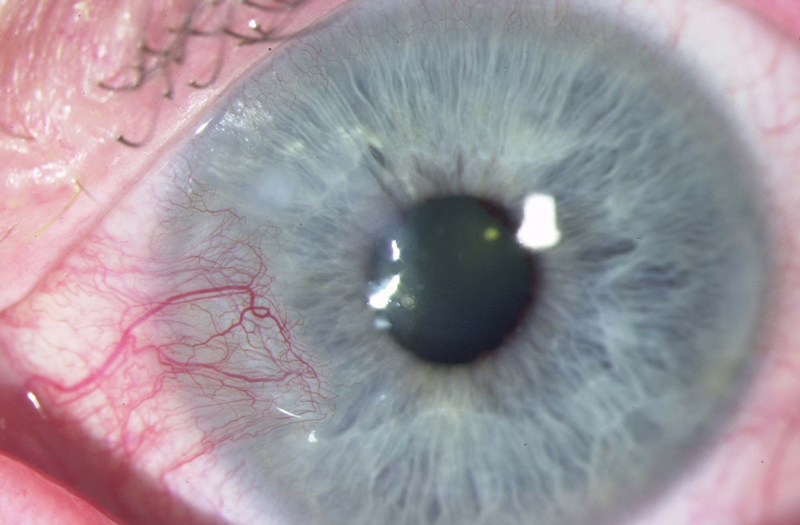
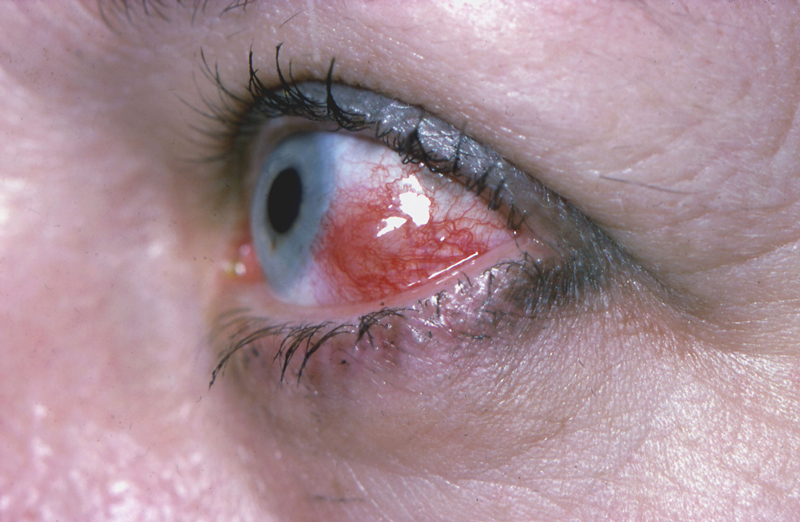
Figure 5 Injection with iritis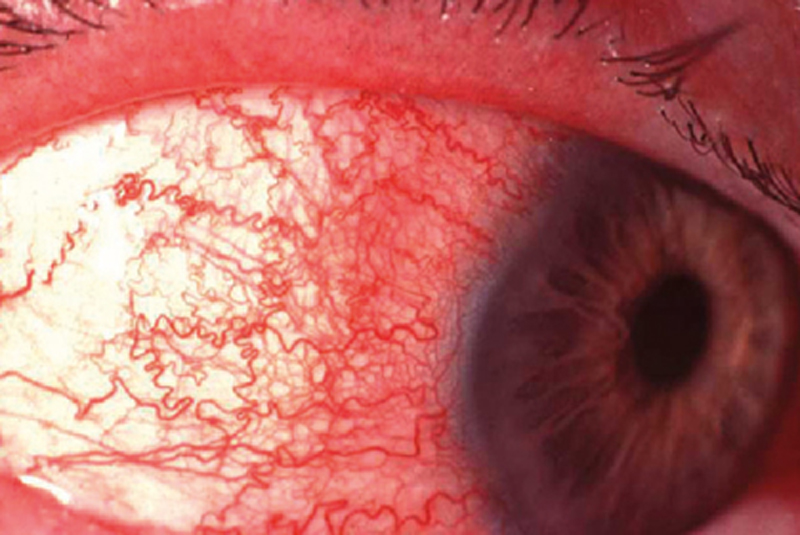
Presentation
- Sudden onset painful eye
- Usually unilateral, but may be bilateral
Signs
- Circumcorneal injection (figure 5)
- Anterior chamber cells and flare (figure 6)
- Keratic precipitates may be fine or large (mutton fat – figure 7)
- Other variable signs include:
- Fibrin
- Hypopyon
- Iris abnormalities
- Raised or low IOP
- Some anterior vitreous cells (spill over)
- Cystoid macular oedema
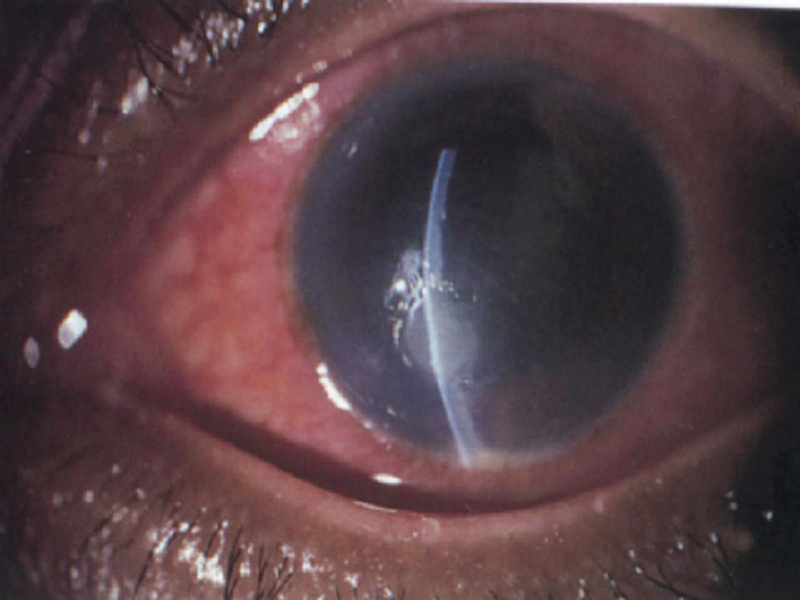
Figure 6 Cells and flare in the anterior chamber seen as a continuous beam of light through the cornea, aqueous and lens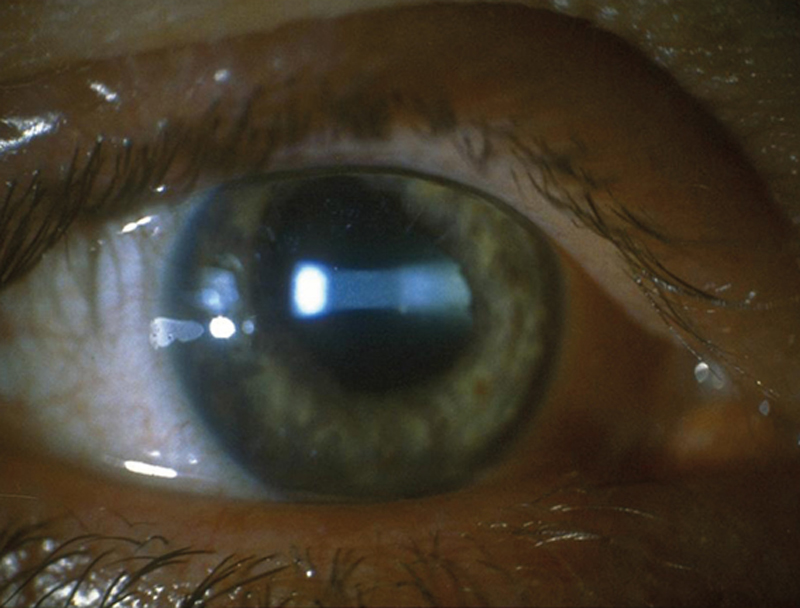 Symptoms
Symptoms
- Pain
- Photophobia
- Redness
- Blurred vision
Figure 7 Large, mutton fat keratic precipitates Investigation
Investigation
- Thorough history to ascertain any systemic links
- Full anterior segment examination
- Dilated examination to exclude posterior involvement
Management and advice
Non-IP optometrists:
- Give advice and refer to ophthalmology via local protocols
If underlying systemic disease and posterior involvement has been ruled out:
- IP optometrists may treat this condition
- Frequent steroid and mydriatic on a reducing dose over six weeks
- Review within 48hrs to ensure drops are working
- Referral to ophthalmology if no improvement in one week
Marginal keratitis
This condition is a response to exotoxins from bacteria. It is thought to be either a toxic or hypersensitivity reaction, usually to staphylococcal bacteria. It is associated with bacterial blepharitis and tends to be recurrent.
Presentation
- Painful red eye with associated foreign body symptoms
- May be linked to atopy, rosacea (figure 8), or chronic blepharitis
Figure 8 Acne rosacea

Signs
- Redness, which may be sectoral or adjacent to the lid margins (two, four, eight and 10 o’clock position where the lid margin crosses the limbus)
- The conjunctiva may also be swollen
- Peripheral ulcer which stains with fluorescein
- The shape of the ulcer can vary from round to arcuate
- There may be single or multiple ulcers
- They are adjacent to the limbus but separated by an area of clear cornea
Symptoms
- Patient sensation can vary from discomfort to pain
- Red eye
- Epiphora
- Photophobia
Investigation
- History of any associated factors such as atopy and rosacea
- Careful anterior segment examination to exclude other causes
Management and advice
Optometrist management:
- Discount other differential diagnosis such as microbial keratitis
- Marginal keratitis is usually self-limiting
- Sunglasses for photophobia may help
- Lubricants can give symptomatic relief
- Systemic pain killers such as aspirin, paracetamol or ibuprofen
- Advice on regular lid hygiene for associated blepharitis
- Meticulous follow-up
IP optometrist management:
- As already stated, marginal keratitis is usually self-limiting, but any topical treatment can consist of antibiotic (chloramphenicol) to help reduce bacteria and steroid (prednisolone or Maxidex) to reduce inflammation. Some eye departments use a combination of Maxidex and neomycin (Maxitrol) as an ointment. Although some patients may be sensitive to neomycin
- Again, meticulous follow-up is essential
Microbial keratitis
This an eye emergency which can be sight threatening but is treatable. However, prompt action is required as well as meticulous follow up.
Risk factors include:
- Trauma
- Contact lens wear
- Ocular surface disease
- Lid disease
- Systemic immunosuppression
- It can be due to bacteria, virus, fungus (figure 9) and acanthamoeba
Figure 9 Microbial keratitis of fungal origin
Presentation
- Sudden onset painful red eye with rapid progression
Signs
- Lid swelling
- Epiphora
- Discharge
- Conjunctival redness
- Corneal lesion (note the position and depth)
- Anterior chamber activity
Symptoms
- Pain which can vary from moderate to severe
- Redness
- Photophobia
- Discharge
- Blurred vision
- Usually unilateral
Investigation
- Full anterior segment examination to look at lids, conjunctiva and cornea of both eyes to exclude other causes
- Check for size and depth of any corneal lesion
- Test corneal sensitivity (can indicate neurotrophic conditions such as herpetic disease)
- Anterior chamber examination to check for cells and flare
Management and advice
- This is an emergency and immediate referral to ophthalmology is required
- Most hospital units perform a corneal scrape to guide therapy
- If the patient wears contact lenses send lenses, case and any solutions for culture
- Treatment will be intense (hourly) topical broad-spectrum antibiotic (fluoroquinolone such as levofloxacin or moxifloxacin) plus mydriatic for photophobia or severe pain
- Sometimes patients are admitted if the lesion is severe and overnight treatment is required
- Polymerase chain reaction (PCR) technique is used to identify fungal organisms
- Acanthamoeba keratitis is rare but 90% of cases of are associated with contact lens wear. Pseudodentrites may be seen in the early stages and early treatment is essential. This includes a combination of a biguanide (polyhexamethylene biguanide, or PHMB) and diamine (propamidine such as Brolene). Steroids may be introduced later to manage inflammation
Recurrent corneal erosion
This is one of those conditions where a provisional diagnosis is sometimes made on symptoms, as the signs may not be present when the patient is examined.
Figure 10 Recurrent corneal erosion
- It occurs when the corneal epithelium does not adhere properly to the basement membrane (figure 10)
- It can be caused by trauma or there may be an underlying corneal dystrophy
- There are several different types of epithelial basement membrane dystrophies (Including Map Dot and Fingerprint dystrophies)
- Other risk factors include diabetes dry eye and ocular rosacea
Presentation
- Sudden onset painful red eye
- May be recurrent
Signs
- Examination may show nothing, or some of the following signs
- Corneal epithelial defect
- Intraepithelial microcysts
- Mild corneal oedema
- If there is a suspicion of corneal dystrophy check both eyes
Symptoms
- Usually affects one eye
- Sharp pain which typically is sudden onset on waking
- Lacrimation
- Photophobia
- Blurred vision
- May recur – this can be over weeks months or years
Investigation
- Careful history to establish if caused by trauma or if it is recurrent
- Ask about dry eye, rosacea and diabetes as these are possible risk factors
- Full anterior segment examination to exclude other possible causes
- Look for signs of epithelial basement membrane dystrophy
- Check for signs of anterior chamber activity
Management and advice
- Lubricating eyedrops during the day and ointment at night. The ointment should be used for at least three months after the last episode to ensure corneal healing
- Bandage contact lenses can also provide relief
- If the patient still has symptoms referral to a corneal ophthalmologist may be indicated for:
- Mechanical debridement of the epithelium
- Alcohol delamination of the epithelium
- Excimer laser phototherapeutic keratectomy
Scleritis
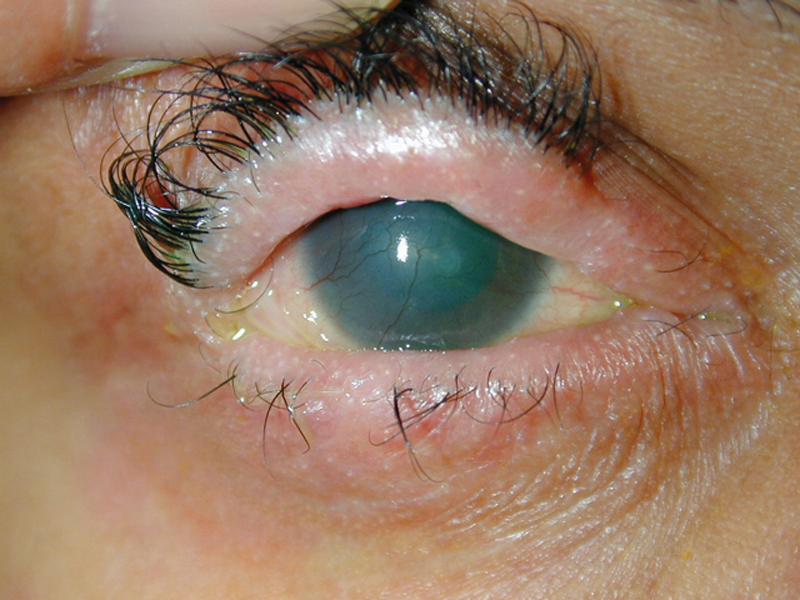
Scleritis can be anterior or posterior (figure 11), it is associated with systemic conditions (such as rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, sarcoid and tuberculosis) in about 50% of cases and can be sight threatening. We will deal with anterior scleritis only here. This is normally classified as non-necrotising (diffuse making up 60% of cases and nodular making up 40% of cases – figure 12) and necrotising (less frequent but more severe – figure 13)
Figure 11 Posterior scleritis
Presentation
- Sub-acute onset of severe pain
- Often worse at night
Figure 12 Non-necrotising scleritis
Signs
- Usually unilateral
- Hyperaemia of both superficial and deep episcleral vessels
- Possible anterior uveitis also present
- Necrotising can show uveal tissue visible beneath thinned sclera
Symptoms
- Moderate to severe pain
- Gradual onset
- Can disturb sleep
- Globe tenderness
- Photophobia
- Epiphora
- Reduced vision
- History of previous attacks
Investigation
- Full anterior segment examination to exclude other causes
Figure 13 Necrotising scleritis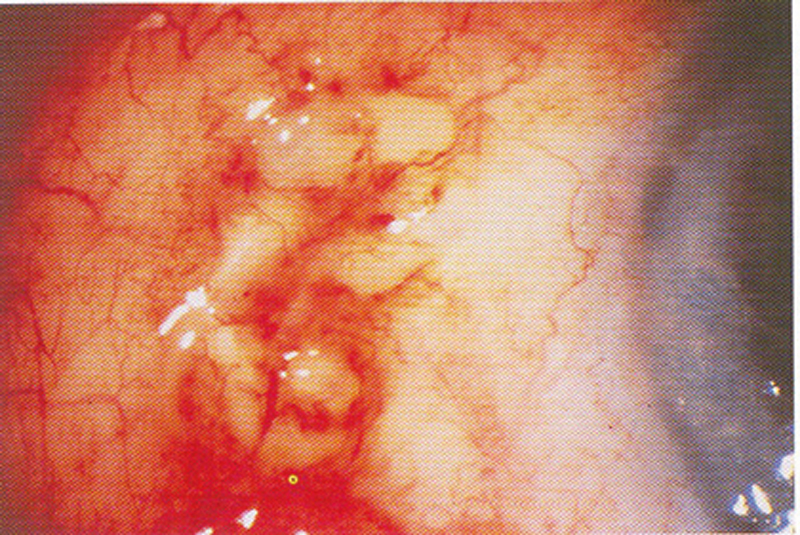 Management and advice
Management and advice
- Scleritis is sight threatening so emergency same day referral to ophthalmology is indicated
- Treatment for anterior non-necrotising scleritis is normally systemic non-steroidal anti-inflammatory tablets such Froben (flurbiprofen) 100 mg, three times daily (sometimes combined with omeprazole if there is a risk or history of gastric or duodenal ulceration)
- As there is a high incidence of systemic associations a full range of blood tests and scans may be carried out
- More severe cases may require systemic steroids or immunosuppressant drugs and newer biologic treatments
Trauma (blunt)
Trauma to the eye may be blunt, penetrating, or chemical. We will discuss blunt trauma here. Most ocular trauma is blunt (80%) compared to penetrating (20%). When dealing with blunt trauma history is important to determine:
- Mechanism of the injury
- Any associated injuries
Presentation
- Sudden onset ocular trauma
- May affect one or both eyes
Signs
- Can vary depending on the type and severity of the injury.
- Bruising
- Subconjunctival haemorrhage
- Corneal abrasion
Symptoms
- Pain
- Lacrimation
- Reduced vision
- Photophobia
Investigation
Careful history
- The cause of the injury
- When did it happen?
- What type of foreign body?
- How much pain and discomfort is there?
Examination
- Measure VA
- Ask about numbness of lower lid, cheek, nose and upper lid. Assess ocular motility for restriction of upgaze and enophthalmos – these could be a sign of a blow-out fracture.
- Assess pupil reactions to look for any RAPD
- Anterior segment examination:
- Cornea for any abrasion
- Anterior chamber for cells flare and hyphaema
- Iris for traumatic mydriasis or iridodialysis
- Lens for subluxation or cataract
- Angle recession (may occur many years later)
- Measure IOP – may be high with uveitis, or low with globe rupture
- Posterior segment examination. Look for:
- Vitreous haemorrhage
- Commotio retinae (grey white retinal opaqueness)
- Retinal detachment or dialysis
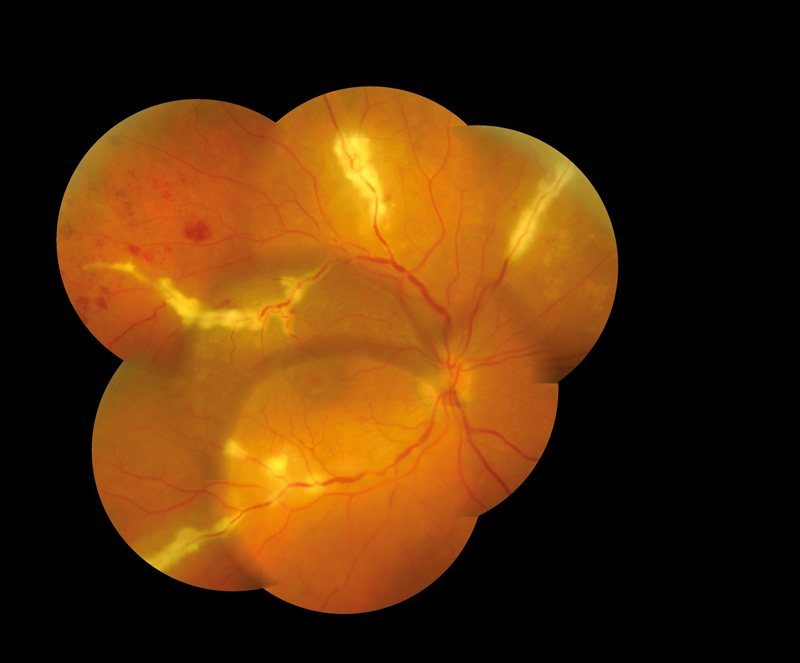
- Macular hole (may be early or late – figure 14)
Figure 14 Macular hole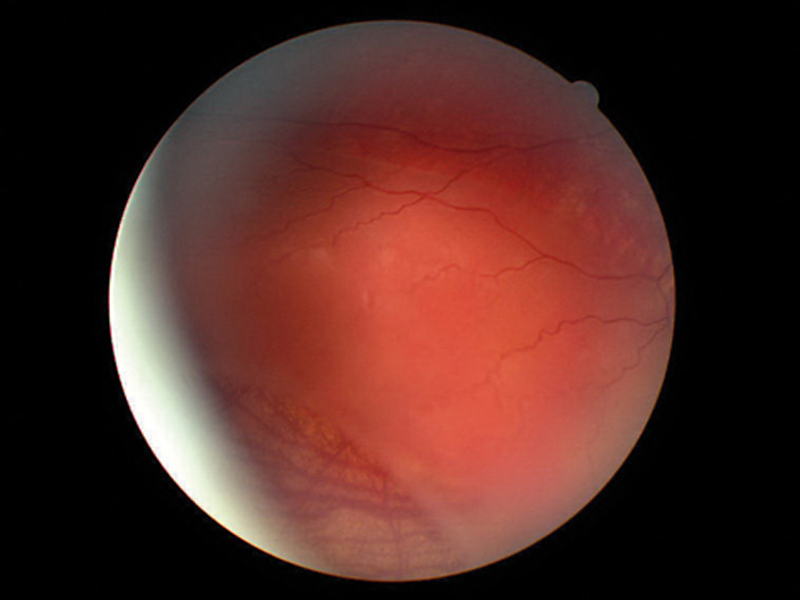
Management and advice
- Depending on severity may be managed in practice but may need hospital admission.
- Important terminology, penetrating versus perforating injury
- Penetrating = the foreign body enters the eye
- Perforating = the foreign body completely passes through the eye
- If there is a penetrating FB some form of imaging may be required (orbital x-ray or CT scan)
Summary
Red eye management is becoming an increasing part of the optometrist’s role. Confidence and competence can be built in practice by seeing these patients, but also by following up every patient to learn from them. Common pitfalls include inadequate follow up and inappropriate use of drugs (ie undertreating in the case of iritis or bacterial keratitis).
The optometrist’s formulary available on the College of Optometrists website to all College members is a great resource to the kinds of drugs that are available to optometrists, both IP and non-IP. It gives more detail about prescribing drops, recommended dosages and duration, and is a great resource for anyone interested in red eye management.
Some clinical tips to remember:
- Always compare to the patient’s other eye. This can give a good indication as to what is normal or abnormal for that patient, as well as narrowing down a diagnosis.
- Trauma is almost always unilateral.•Contagious conditions such as viral or bacterial conjunctivitis usually present bilaterally, although the response in each eye may be unequal. Bacterial infections usually take no more than 24 hours to affect both eyes.
- Viral conjunctivitis may take longer.
- Systemic and allergic conditions are usually bilateral from the outset.
Finally
When giving patients management and advice options, good communication is important.
Remember to always give appropriate SOS advice and document everything that has been said and done.
Colin Davidson is an independent prescribing optometrist who works in independent practice and hospital A&E and uveitis clinics and based in Sussex.
Further Reading
Unless otherwise stated references for this article have been taken from:
- The College of Optometrists Clinical Management Guidelines found at www.college-optometrists.org/guidance/clinical-management-guidelines.html
- Oxford Handbook of Ophthalmology 3rd Edition Alastair Denniston, Philip Murray
- Moorfields Manual of Ophthalmology, Timothy L Jackson
- Manual of Eye Emergencies – Diagnosis and Management Lennox A Webb
