When WC Fields made his famous quote ‘Never work with animals or children’ he was referring to fellow actors in the film industry but the adage is used in other walks of life too. However, those who follow its precepts miss out on a lot. I cannot speak much about testing the eyes of animals but examining and caring for children’s eyes can be both rewarding and amusing.
This article aims to provide suggestions and ideas for examining the eyes of young children from nursery age upward, and to make the experience more useful and enjoyable for both the child and the practitioner. It does not go into detail about all the different components that make up a complete sight test.
Children need to be reviewed more frequently than adults so there is the chance to build up a good rapport with them and their families and to watch how our input into their visual development adds to their capability and self-assurance. A young child who has been struggling to see the board in class can be amazed at the instant improvement a pair of myopic spectacles affords. After a few years, the same child may not want to have to wear glasses and fitting them with contact lenses can markedly improve their self-confidence.
The definition of a ‘child’ varies depending on the context but when examining children, it is up to the practitioner to gauge the intellect of their patient and treat them accordingly.
Before the appointment
In order to help children feel more familiar with what happens when they attend for their appointment, have a children’s section on the practice website. It can contain eye-related facts, colouring games or downloadable sheets. Include some videos or links to information videos on other sites such as ABDO’s Professor Hallux’s i-guide www.funkidslive.com/learn/hallux/i-guide, the College of Optometrists’ infographic of a child having a sight test, or the eye movie on the Kidshealth website kidshealth.org. There are also several YouTube videos of children’s eye tests including Peppa Pig’s ‘The eye test’.
Arriving at the practice
Try to consider the whole experience from the child’s point of view. Coming to have a ‘test’ or an ‘examination’ can be nerve-racking, so if space allows, have a small table in the waiting area with a few books, some easily cleanable toys, and washable crayons with frequently replenished paper or colouring sheets. Put up child-friendly posters: cartoon characters, children and animals wearing glasses (figure 1), and show some videos of eye-related topics but check in case you need a license for any of them.

Figure 1: Even dogs wear glasses
Welcoming your patient
Decide beforehand what you want children to call you; you may or may not think it appropriate that a four-year-old child calls you by your first name. Remember, you are a professional, not the patient’s friend, and it can help to maintain the professional relationship to introduce yourself as Mr/Ms Name. That is the main reason that children usually do not call their teachers by their first name.
When you call in your patient, smile and greet them by name, greet the parent and introduce yourself. This may seem obvious but it is very easy to walk ahead of them looking at the record card, and it can be quite daunting for a child to have to follow a strange person into a room filled with implements of torture (think what a slit lamp or a phoroptor head might look like if you have never seen one before).
In the consulting room, try to put both child and parent at ease. Ask if the child would prefer to sit on someone’s lap or on the chair on their own, or if they arrive in a pushchair, let them stay sitting in it if they are content. Begin with some inconsequential conversation.
Topics can include:
- What they are wearing eg a football team t-shirt, cool shoes or pretty colours of clothes.
- School holidays or birthdays depending on the time of year.
- The name of a toy if they have brought one with them and whether it would like to have its eyes tested as well.
Communication
Be sure to check the name(s) of the accompanying adult(s) and note it on the record card (see Legal aspects below). This can avoid problems in the future, for example where the parents do not communicate with each other. (For simplicity, I have used ‘parent’ rather than ‘accompanying adult’ for this article).
Try to make the questions and discussion age specific and look at both child and parent as you speak. Start by asking their age, even though you probably already know it. This is an easy question that they will know the answer to. Further topics can lead into talking about their eyes:
- Which school or nursery they go to?
- What subjects they like?
- Where they sit in the classroom?
- Can they see what the teacher writes on the board? If the answer is no, is it because they cannot see well enough or because the teacher has poor handwriting?
- Have they had their vision checked at school?
Be aware of your terminology and what it might mean to the child. If you use a word that you think they might not understand, ask if they know its meaning. They are unlikely to have come across words like ‘focus’ and ‘lens’ and they may assume that ‘testing your eyes’ means that they are about to have a reading test. Explain or use different words if you think they do not understand:
- ‘Fuzzy’ instead of ‘blurry’
- ‘A little window’ rather than ‘a lens’
- ‘Is it easy to see/ read?’ rather than ‘Is it clear?’
Children are much more literal than adults so ‘Can you see the top line on the chart?’ may simply elicit an affirmative answer. It is better to ask ‘Can you read the top line to me?’
Children who arrive at the end of the day wearing their school uniform are likely to have come straight from school and be tired. Although this can be a disadvantage, it can prove useful in revealing decompensating phorias and headaches caused by uncorrected ametropia.
At the end of every consultation ask parent and child if they have any questions.
Most discussion goes on in front of the child but occasionally, you may feel it is more appropriate to speak to the parent without the child being present. If this is not possible in the practice, try to call the parent later.
History and symptoms
Go through the standard questions:
- General health
- Family history –
- Whether any child in the family wears glasses.
- If any adults wore glasses as a child.
- History of squint, lazy eye or patching.
- Other eye problems or hospital treatment for eyes.
- Ask the parent why they booked the appointment.
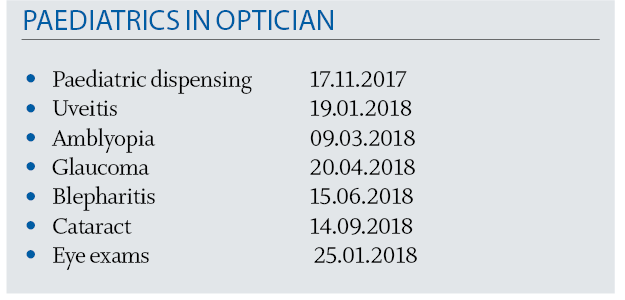
- Ask the child about any specific problems but be aware that the answers may be inaccurate. Table 1 shows some possible alternative meanings to what is being said.
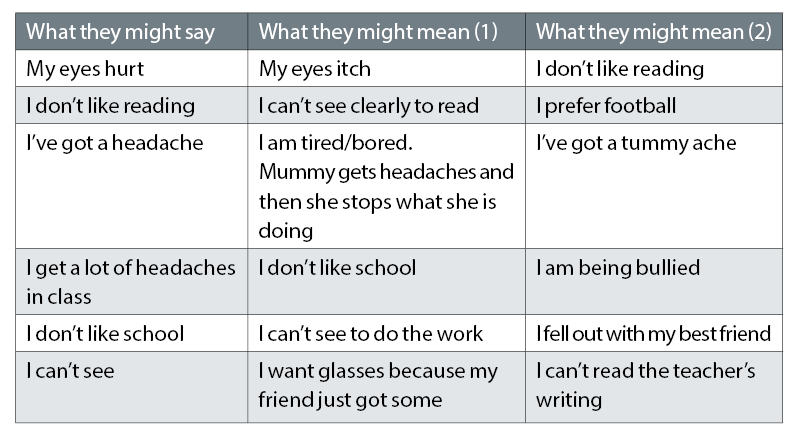
Table 1: Possible interpretations of what a child might say
Children will not usually complain that they cannot see, they just assume everyone sees the same as they do so rather than asking if they can see clearly, questions that elicit more useful answers might be:
- Can your friends/family see things that you can’t see?
- Can you see what the teacher is writing or holding up if you are at the back of the class?
Do they enjoy reading? If not, try to find out why. Is it because:
- They cannot see it (uncorrected refractive error)?
- They do not like the story that they are reading this week?
- The words seem to dance around or have different patterns making it hard for them (possible dyslexia)?
- They are simply not able to read as well as their peers?
- Uncorrected refractive error.
- Not as intelligent as their peers. Some high-flying parents are loathe to accept that their child is not bright and will take them to many professionals to find an alternative that they are willing to accept.
What are their hobbies?
- Can they see the goal when they are playing football?
- Do they get headaches or eye aches playing their video games?
Fabricated symptoms
Occasionally children will fabricate symptoms. This may be because they want glasses like their friend but it can be attention seeking and be aware that it might relate to bigger concerns such as bullying, family problems, abuse or psychological issues.
Headaches
If they are complaining about headaches, ask where on the head it hurts. They may not give a precise answer especially if it was not really a headache.
Are the headaches:
- Recent onset?
- Changes at school, home, family relationships?
- Only on school days?
- Eyesight problem?
- Stuffy classroom?
- Insufficient water?
- Do they dislike going to school? If so, why?
- After certain lessons?
- Concentrated close work or IT?
- At the end of the day?
- Uncorrected refractive error or decompensating phoria?
- Overtired?
- Insufficient water?
- In a particular room
- Stuffy classroom
- How much time do they spend on a ‘rectangular device’ (phone, tablet, computer)?
- How close do they hold their tablet when playing games?
- How close do they hold a book to read?
- Does a member of the family get a lot of headaches and the child simply copies them?
The eye examination
At the first appointment, everything is unfamiliar and a bit frightening both for the child and possibly also the parent. Some children misbehave when they are nervous, others become very shy. Having stickers on pieces of equipment can make them look less scary (figure 2).

Figure 2: A sticker on a retinoscope. This can also act as a target for dynamic retinoscopy
The first hurdle to overcome is to get your patient to sit still long enough to test their eyes.
A few general points:
- Explain what you are doing as you go along and what the equipment is.
- Always say when you are turning the lights off or on. Do not stick to a strict routine so if the child wants to play with the trial lenses, start with retinoscopy and leave history and symptoms until later.
- Let the child ‘help’ by perhaps holding up a trial lens or attempting to hold down an eyelid.
- When examining patients on the slit lamp, tell them if you need to touch their lids, and warn them if your hands are cold.
- Be flexible in your approach: if a child will only calm down when sitting on the floor, then carry out some of the sight test there.
- Let them eat or drink while you are testing if it helps keep them still.
- Learn a lot of silly jokes – “What do cows do in their spare time? Go to the moovies!”
- For little ones, get to know some popular children’s characters so that you can bring them into the conversation and be prepared to sing nursery rhymes – ‘The Wheels on the Bus’ usually goes down well.
- If necessary, bring the child back on another day to complete the eye examination.
- When the child does behave well, praise and thank them even if they were naughty for most of the consultation. They will usually respond to encouragement and will try harder and next time, they are likely to be less nervous and so easier to examine.
- Have a large variety of stickers to give as rewards. It is better not to give edible rewards in case of allergies or religious convictions.
- Do not forget to praise and thank siblings who behave and give them stickers as well.
Fixation targets
- Have a supply of small toys, disco balls and finger puppets (figures 3a and b) to use as distractions and near fixation targets.
- Before using a specific fixation target, check that they are not frightened by it; some children are scared of clowns or flashing lights.
- Ask the parent to act as a fixation target by standing behind you and making funny faces or holding their phone, possibly showing a video the child likes.

Figure 3a: Fixation targets. Small toys and finger puppets

Figure 3b: A disco ball is one of the best fixation targets
Testing visual acuity
Table 2 shows the distance and near acuity tests used at different ages. Tumbling E and Landolt’s C tests are rarely used nowadays. Until a child can name pictures or letters, it is not possible to accurately measure near vision.
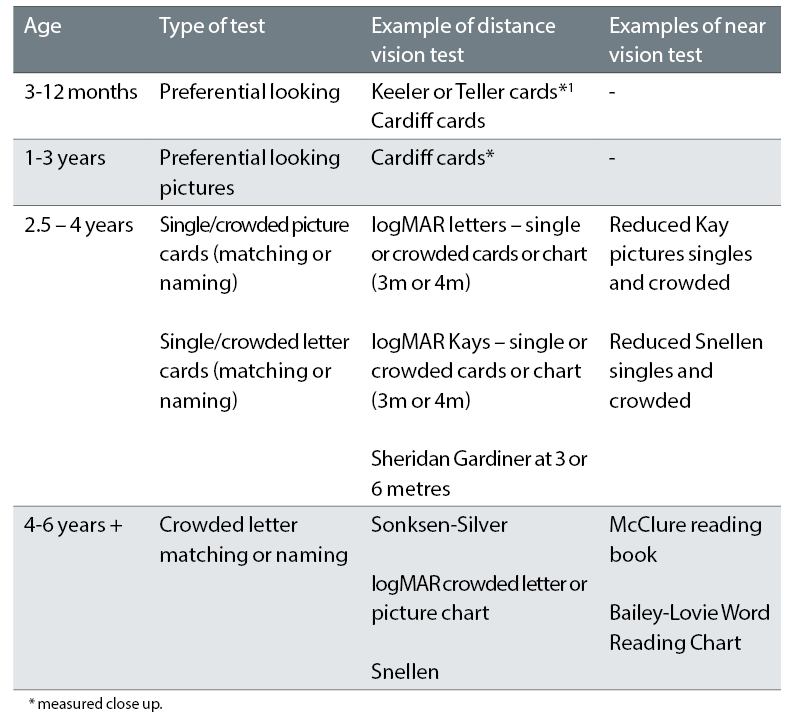
Table 2: Acuity tests used for children. Tests in bold are the preferred option
Infants and young children are not able to say what they see but if shown two images, where one provides more visual stimulation than the other, they will look towards the more visually stimulating image. This response is utilised in forced choice preferential looking cards such as Keeler or Teller cards for infants or Cardiff picture cards for older, pre-school children (figure 4).
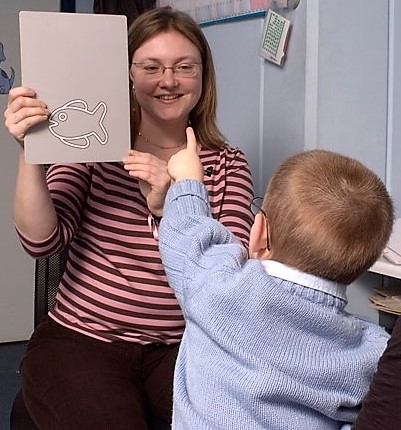
Figure 4: Testing acuity with Cardiff cards (courtesy of Bronwen Walters)
The logMAR chart is standardised and allows different tests be compared easily2 so, for example, the logMAR Kay picture test is comparable to the standard logMAR (letter) tests.3 Table 3 shows distance acuity norms for infants and children.
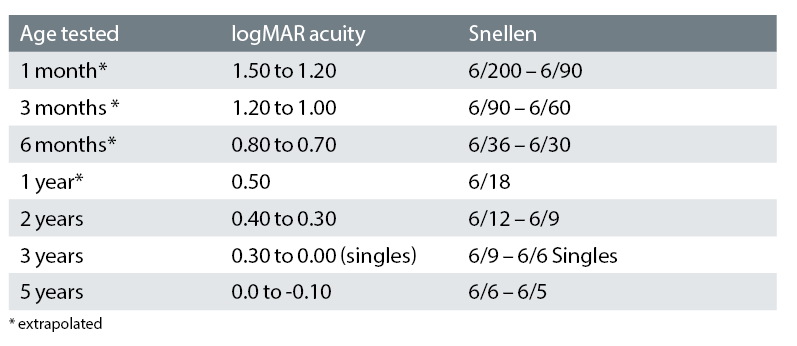
Table 3: Distance acuity norms for infants and children (adapted4)
Always test reading as well as distance vision and watch the child rather than just the chart. Do they screw up their eyes or look over their glasses; do they hold the reading matter very close? These might indicate difficulties.
LogMAR reading acuity measured at 25cm should be the same as logMAR distance acuity, so if a child sees 0.30 logMAR in the distance, they should be able to see 0.30 on a Reduced logMAR card at 25cm (figure 5).5
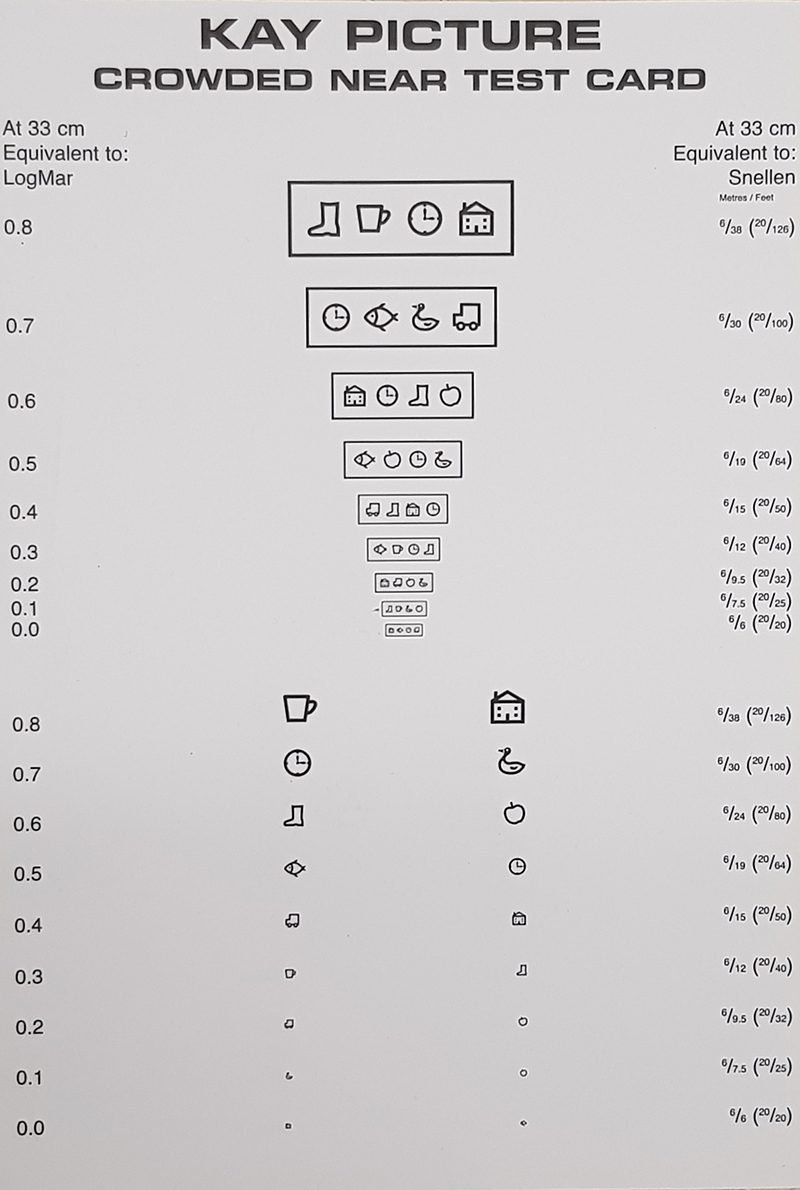
Figure 5: Reduced Kay picture test
Children seem to be programmed from an early age not to guess when they are asked a question, so unless they are certain of something, they will usually not respond as they do not want to get it wrong. Where letters or pictures are similar, an older child or adult will plump for one of them but just because a younger child says nothing, it does not mean that they cannot see. Encourage them to have a go and if mistakes are made, simply encourage them to continue. If the Kay pictures are not familiar, give them a sample sheet of pictures (figure 6) to take home to learn so when you see them again, it will be easier to measure acuity.
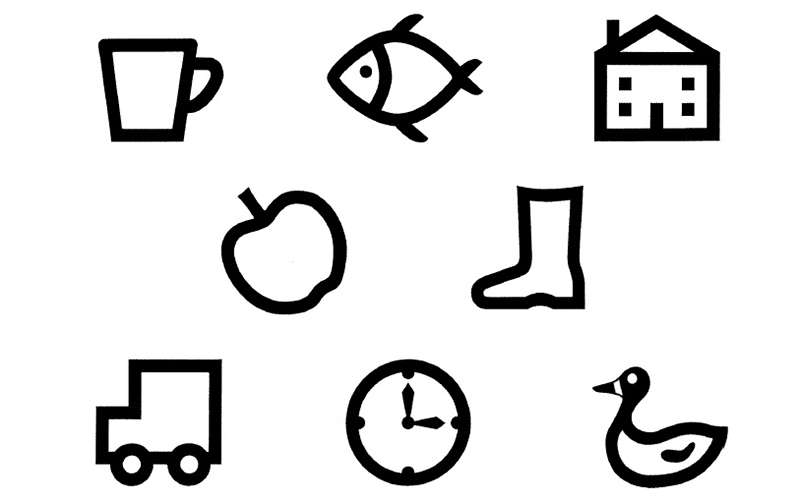
Figure 6: Kay picture matching card (Courtesy of Kay pictures)
Do not underestimate a child’s memory or intelligence. They can quickly learn the letters or pictures on a test chart. A digital chart, with randomised letters and symbols such as COMPlog, or a variable chart such as the Thomson Test Chart, is better than a static one.
Refraction
Why bother with retinoscopy?
Retinoscopy is not carried out as often as it used to be since autorefractors have taken over in many practices but an accurate retinoscopy is particularly useful when examining children because as well as measuring refraction and accommodation, it can reveal opacities of the lens and ocular media, corneal irregularities and some retinal anomalies such as staphyloma. If reading acuity and accommodation are abnormal, dynamic retinoscopy (see figure 2) is a useful process.6
Whether sitting behind a phoropter head or wearing a trial frame, a small child is unlikely to be comfortable so it is usually more practical to hand-hold trial lenses while doing retinoscopy. Hold the lens in front of your own eye, teddy’s eyes (figure 7) or the parents’ eye to demonstrate. With an uncooperative patient, hold the neutralising lenses as in Figure 7 and move the retinoscope light quickly across both eyes. This can give an idea of whether there is a refractive error.

Figure 7: Testing a patient’s eyes using hand-held lenses for retinoscopy
Subjective examination
- A small trial frame is necessary for subjective testing such as Miraflex Chidren’s Trial Frame by Dibble Optical.
- Young children cannot discern small changes. Demonstrate a +/-1.00 sphere or cylinder change to show the difference and then reduce to +/-0.50.
- Do not rely on the response that something is better/clearer; instead ask what they can see using a different set of letters or pictures.
- A child of less than seven years is unlikely to comprehend the concept of cross cylinder so physically move the cylinder axis by 10 or 20 degrees to demonstrate an axis change.
- Red/green test results are also somewhat unreliable at a young age.
Dilating drops
Dilating drops are almost always necessary if the vision is not normal or there are any problems or symptoms. It may be preferable to book a second appointment for dilation so that the child doesn’t always associate the optometrist with stinging drops. However, sooner or later, you will need to explain to both parent and child that you are going to instil drops that, in all honesty, sting like soap and cause marked photophobia. There is no good way to do this but you can make the experience more or less horrible. (See Legal aspects at the end of this article).
Explain why drops are necessary and that the vision might become fuzzy. If asked, do not lie by saying the drops will not hurt as your patient will never believe you or any other clinician again but do not dwell on the discomfort either, for example say the drops might be uncomfortable.
Being able to make a choice helps the child feel more in control so they could choose:
- Which eye the drop will go into first?
- Who will instil the drops – you or the parent?
- Where they want to sit, on the chair on their own or on their parent’s knee?
Once the drop is in, explain that the discomfort only lasts about 20 seconds and if they count slowly to 20, it will feel better. Try to instil the drop into the second eye as soon as possible after the first so both eyes can settle together.
Some practitioners advocate the use of a local anaesthetic first7 but the author finds this to be a hindrance. It prolongs the agony by making the child go through an extra set of drops and some people find local anaesthetics also hurt.
Fundoscopy
Fundoscopy is usually carried out once the refraction has been completed. A bio head set allows easier viewing of the optic discs than direct ophthalmoscopy. Even in young children, photographs of reasonable quality can be acquired using a digital camera or SLO system.
Whether to prescribe glasses
Refractive errors can change a lot as the eyes of infants and children emmetropise8,9 so except with high prescriptions, it is advisable to recheck a prescription three to four months later before prescribing glasses. There are different opinions on when and what to prescribe,10-13 but generally, if there are no symptoms and the vision is good, spectacles should not be necessary. A symptomless low hyperope, say +3.00DS, with normal VA and accommodation and no heterophoria, does not need spectacles, but one who has difficulty with reading or is complaining of headaches after close work is likely to benefit from wearing their full or a partial correction.
Consider the acuity test being used, so for example, the Cardiff card test is carried out at 50cm or 1m so can be seen well by myopes, and achieving 6/6 with a Sheridan Gardiner single letter matching test is much easier with an uncorrected refractive error than 0.0 on a Keeler logMAR crowded test.
The active accommodation of young patients can make them appear myopic without cycloplegia. Most will admit to improved vision on the letter chart when minus is added, so it is necessary to carry out a cycloplegic refraction before ordering glasses. If a myopic correction is found, the full prescription should be given for school-age children.12 At subsequent appointments, if myopia is found to be increasing, the type of correction to prescribe and whether to consider myopia control in the form of multifocal spectacles or contact lenses should be discussed with the parents.14,15
Just because there is a high refractive error does not mean the child will want to wear the correction. Giving a lower prescription can help them (and their parents) get used to the glasses, for example, a young -6.00DS myope may find the corrected vision too sharp so ordering -4.00DS can ease them into spectacle wear. In addition, it will affect their reading distance less and the reduced image size will be less of a problem (this is especially important in children with poor acuity). The same applies to astigmatic errors. Always explain that the prescription will probably increase at the next appointment, otherwise they will assume that the vision has got worse.
With high prescriptions, visual development and the amblyogenic period are of prime concern. If reluctant to wear the glasses at all, encourage building up the wearing time from as little as five minutes initially. Getting the parents to remove the glasses while the child is looking at something can help them notice the difference. Consider that if a high hypermetrope wears their glasses consistently for close tasks, they are unlikely to have any major problems as they will still be having a reasonable amount of focused visual stimulation.
Dispensing and wearing glasses
(See Optician 17.11.17 of the current series)
When a child is told they need glasses, they may be really pleased or they may burst into tears. The same goes for their parents. The hardest situation to deal with is when a parent insists that their child will look awful in glasses and will not wear them. It can take a lot of gentle persuasion to overcome the parent’s prejudice.
Have a good selection of children’s frames with different bridge types and frame colours. If possible, let the child choose their own frames and see themselves in a selfie on their parent’s phone. They are more likely to wear the glasses if they have been allowed to have the colour and style they want, but make sure the frame fits well and is comfortable and that the sides are not too long. If necessary, shorten the sides rather than simply bending very long sides.
Children with disabilities
Disabled children are more likely to have eye problems and visual impairment than the general population16 but many young disabled children have never had a sight test. Down syndrome is a known risk for eye problems and Woodhouse et al17 found 91% of their group of 136 children had a reduced amplitude of accommodation.
It is beyond the scope of this article to go into detail about testing the eyes of children with disabilities or autism but the basic tenets used to put your patient at ease are the same for all.18 There are numerous web links available including National Autistic Society,19 College of Optometrists,20 SeeAbility.21
Letter writing
If there are visual problems, explain them in a letter to the school (or preferably to the parents to give to the school). State what the distance and near acuities are and advise on how best to help the child by enlarging print and sitting at the front of the class. Sometimes a pushy parent will try to persuade the practitioner to write a letter for a child who is not doing well in school. If you don’t think the child’s vision warrants extra help, don’t be persuaded.
Schools frequently discourage spectacle wear for sports so explain why a myope will have problems if they cannot wear their glasses. Ensure their glasses are safe to wear and if necessary, recommend sports goggles. A sports band will secure a pair of glasses for swimming.
Legal aspects
- DBVS (Disclosure and Barring Service) - If you are likely to see children regularly, you will need to have an enhanced DBS check.
- Safeguarding – Sadly many children are either neglected or abused so safeguarding training is essential.
- Prevent – training to help recognise if children and young people are being radicalised.
- Competence – is a child able to comprehend and consent to what is being done to them? For young people aged 16 years or older, their ability to consent for treatment needs to be assessed in accordance with the Mental Capacity Act 2005.22
- Data – as with adults, data must be protected23 (Data Protection Act, 2018).
- Records – For children and young people, records must be kept for 10 years after they were last seen or until the patient’s 25th birthday.20
- Parental responsibility – Note who accompanies the child. Parents do not automatically have parental responsibility and so may not be entitled to know about the child’s medical information.24
Conclusion
Testing the eyes of young children is challenging but you are never likely to be bored and the benefits that good, comfortable vision can provide for a child in all walks of life cannot be overestimated.
Lynne Speedwell is Head of Optometry, Great Ormond Street Hospital for Children NHS Foundation Trust and Principal Optometrist, Moorfields Eye Hospital.
Further Useful Sources of Information
College of Optometrists20
- Examining younger children
- Examining patients with learning disabilities
- Communicating with younger children
- Safeguarding children and vulnerable adults
- Children and young people with the capacity to consent
- Guidance for professional practice
- Patient resources
- Stickers, colouring sheets and information for children
- A child’s eye examination video
- Parents short guide to children’s eyes.
DOCET – Examining Children.25
Optical Confederation26 – Safeguarding Guidance on Safeguarding, Mental Capacity and the Prevent Strategy Gov.uk27
- Child abuse concerns
- Safeguarding children
- Parental rights and responsibilities
Great Ormond Street Hospital is the country’s leading centre for treating sick children with the most complex conditions, and has the widest range of specialists under one roof.
References
1 Teller D, McDonald MA, Preston K, Sebris SL, Dobson V. (1986) Assessment of visual acuity in infants and children; the acuity card procedure. Dev. Medicine and Child Neurology 779-789
2 Bailey I, Lovie J. (1976) New design principles for visual acuity letter charts. Am J Optom Physiol Opt 53:740–745.
3 Elliott MC and Firth AY (2009) The logMAR Kay picture test and the logMAR acuity test: a comparative study. Eye 2009 23(1):85-8. Epub 2007 Sep 28
4 Fulton AB, Hansen RM, Moskowitz A, Mayer DL (2005) Normal and abnormal visual development. Hoyt and Taylor, Pediatric Ophthalmology and Strabismus 4th edition, Chapter 4, published by Elsevier.
5 Johnston AW. (2016) ACLM Yearbook and https://www.researchgate.net/publication/302954722
6 Hunter DG (2001) 2001 Dynamic retinoscopy: the missing data. Surv. Ophthal. 46(3):269-74.
7 AAPOS American Association for Pediatric Ophthalmology and Strabismus. https://www.aapos.org/terms/conditions/43
8 Gwiazda J, Thorn F, Bauer J, Held R. (1993) Emmetropization and the progression of manifest refraction in children followed from infancy to puberty. Clin Vis Sci, 8 (1993), pp. 337-344
9 Mayer DL, Hansen RM, Moore BD, Kim S, Fulton AB. (2001) Cycloplegic refractions in healthy children aged 1 through 48 months. Arch Ophthalmol, 119: 1625-1628
10 Miller JM, Harvey EM. (1998) Spectacle prescribing recommendations of AAPOS members. J Ped Ophth and Strab. 35 (51-52)
11 Lyons, S, Jones, LA, Bartolone AG, Carlson NB et al (2004) A survey of clinical prescribing philosophies for hyperopia. Optom Vis Sci. 81(4):233-7
12 Leat SJ (2011) To prescribe or not to prescribe? Guidelines for spectacle prescribing in infants and children. Clin Exp Optom 94: 6: 514–52
13 Woodhouse M. (2016) Spectacle prescribing for young children Optometry Today No. 50551, May 2016
14 Gifford, K. 2016. Putting myopia control into practice. Optometry Today, C-52154.
15 Logan, NS, Gilmartin, B, Cho P. (2019) Contact Lens Correction and Myopia Progression. Phillips & Speedwell, Contact Lenses 6th edition, Chapter 28 published by Elsevier
16 Salt A, Sargent J. (2013) Common visual problems in children with disability. BMJ 99(12). http://dx.doi.org/10.1136/archdischild-2013-305267
17 Woodhouse JM, Pakeman VH, Saunders KJ, Parker, M, Fraser, WI, Lobo, S, Sastry, P. (1996) Visual acuity and accommodation in infants and young children with Down's syndrome. J Intellectual Disability Research 40(1): 49-55
18 Gowen E, Porter C, Baimbridge P, Hanratty K, Pelham J, Dickinson C. (2017) Optometric and orthoptic findings in autism: a review and guidelines for working effectively with autistic adult patients during an optometric examination. Optom in Practice 18 (3): 145-154
19 National Autistic Society website https://www.autism.org.uk/
20 College of Optometrists. Guidance https://guidance.college-optometrists.org/guidance-contents
21 SeeAbility https://www.seeability.org/eye-tests-explained
22 Great Ormond Street Hospital for Children – Consent for treatment https://www.gosh.nhs.uk/parents-and-visitors/advice-when-you-stay/preparing-treatment/consent-giving-permission-your-child-have-treatment
23 Data Protection Act 2018 http://www.legislation.gov.uk/ukpga/2018/12/contents/enacted
24 gov.uk – https://www.gov.uk/parental-rights-responsibilities/who-has-parental-responsibility
25 Adler P, Weddell L. Examining children DOCET https://docet.info/pluginfile.php/49038/mod_resource/content/1/examining_children_booklet.pdf
26 Optical Confederation – Safeguarding Guidance on Safeguarding, Mental Capacity and the Prevent Strategy http://www.opticalconfederation.org.uk/downloads/oc-safeguarding-guidance-updated-june-2017.pdf
27 gov.uk - https://www.gov.uk/topic/schools-colleges-childrens-services/safeguarding-children
