Are you sitting and seeing comfortably? Then let’s begin.
Pause for a moment to think about the answer to that question. Are you sitting comfortably? How does your body feel right now? Where would you place yourself on a scale moving from absolute comfort to total discomfort, or even pain? Comfort is complex and multifactorial. This is no less true when it comes to the eyes, specifically the comfort experience of the contact lens (CL) wearer. This article explores the influences on CL comfort, examining how both physical and visual elements contribute to the overall comfort experience.
Defining comfort and discomfort
Defining comfort and discomfort is not straightforward. Neither is it a binary concept, where the absence of discomfort implies comfort and vice versa. Research in the field of ergonomics defines comfort as ‘a pleasant state or relaxed feeling of a human being in reaction to its environment’ and discomfort as ‘an unpleasant state of the human body in reaction to its physical environment’.1 Interestingly, the absence of discomfort does not automatically result in comfort, rather that without discomfort, nothing is experienced.2 To report comfort, more must be experienced, and for studies of ergonomics, that extra is related to luxury, relaxation or feeling refreshed.1
Contact lens experience
In terms of CLs, overall comfort is influenced by both the physical and visual experience (figure 1).
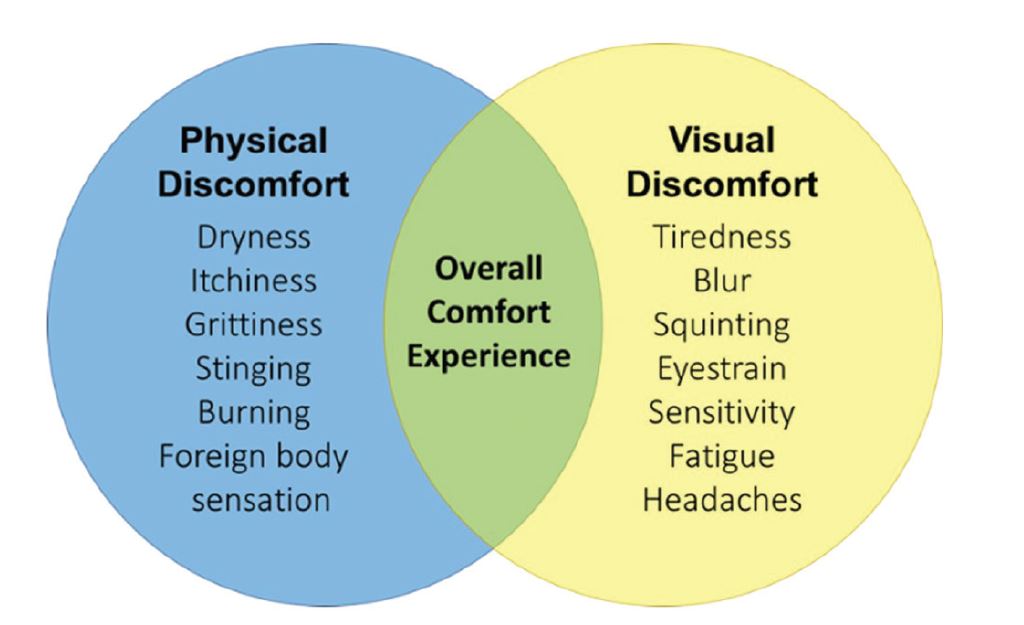
Figure 1: Contributors to the overall comfort experience of contact lens wear
Physical contact lens discomfort
With regard to the physical experience of CLs, discomfort is most often evident in the end of day sensations and reduced wear times patients may describe. For some it may simply be reported as an inability to wear lenses as long as desired. For others, the sensations experienced may be described in words. ‘Dryness’ and ‘discomfort’ remain the most commonly cited reasons for drop out,3,4 especially for established wearers, and the practitioner should be alert to these words, or alternatives such as ‘stinging’, ‘gritty’, ‘scratchy’, or ‘irritated’. It is worth noting that new wearers experience issues with handling and vision, both of which can contribute to drop out among this group in addition to problems with comfort.5
The Tear Film and Ocular Surface Society’s (TFOS) 2013 workshop reviewed the evidence available about contact lens discomfort (CLD) in relation to its etiology, investigation and management.6 CLD is common, with on average around half of CL wearers affected.7 Unsurprisingly, the etiology of CLD is complex, with many possible causes contributing to the overall level of comfort experienced by the wearer. The report suggested how contributors to CLD can be classified into CL and environmental factors. CL factors cover material properties, design, fit and lens care. It remains challenging to study the contribution of these factors in isolation from each other: changing one material property to examine its effect on comfort invariably changes other elements within the CL.
Table 1 contains a short summary of how these CL factors may contribute to CLD.
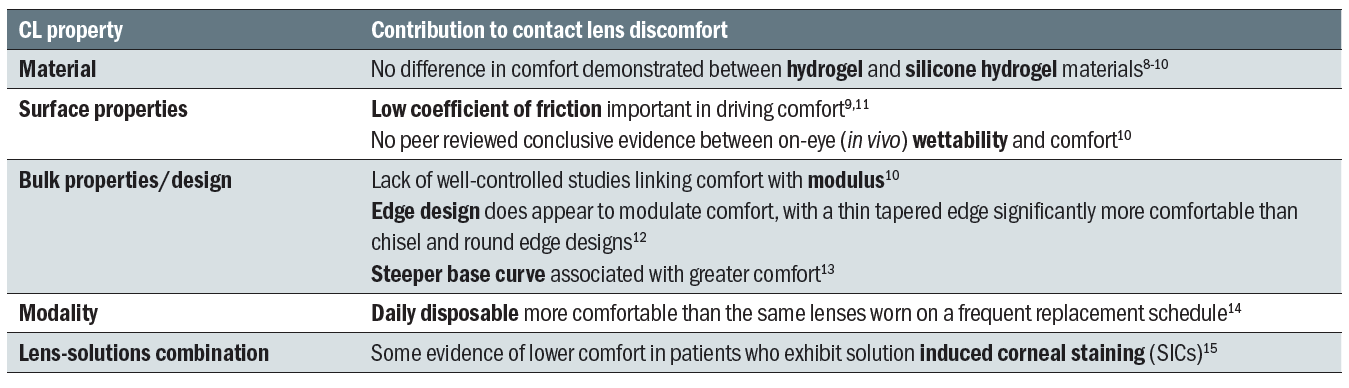
Table 1: Factors associated with contact lens discomfort
Addressing contact lens discomfort
To effectively manage this multifactorial problem, there are two important considerations. The first step is to question the patient thoroughly about their comfort experience. The amount of time CLs can be comfortably worn for should always be established. If a gap of two hours or more exists between the total and comfortable wearing time, it can be an indication of ‘less than successful wear’16 and the practitioner should be prompted to investigate and manage the situation. Use of a validated questionnaire is recommend to quantify and track change in symptoms over time. The CL dry eye questionnaire (CLDEQ-8) asks specific questions about the frequency and intensity of dryness and discomfort symptoms.17
The second important consideration in addressing CLD is to have a methodical approach. The TFOS CLD report suggests a management strategy which involves addressing co-existing factors prior to changing the CL or other ocular or environmental factors.18 For instance, presence of blepharitis would indicate this is managed first, followed by further recommendations that may include increasing replacement frequency by changing to a daily disposable and use of lubricating drops. The actions taken once any other co-existing factors have been addressed are summarized in table 2.
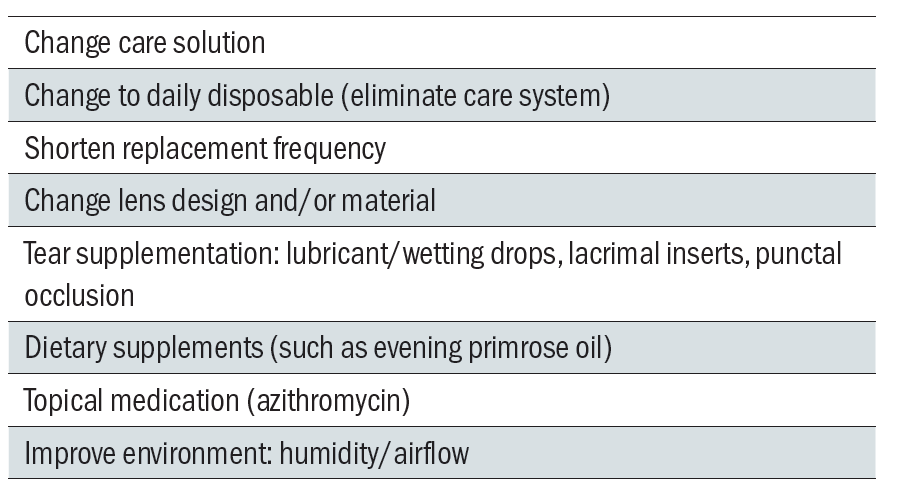
Table 2: Options to manage contact lens discomfort, adapted from TFOS International Workshop on Contact Lens Discomfort: Report of the Management and Therapy Subcommittee 18
Finally, with reference to physical comfort, it must be acknowledged that studies suggest decline in comfort throughout the day may be more related to a fatigue-like response in the ocular tissues and changes in the ocular environment than to the contact lens itself.19,20
Visual discomfort
The physical sensation of discomfort alone does not fully describe the CL wearing experience. To build a complete picture, the perceptual elements of visual comfort must also be considered. Visual comfort is of course relevant to all patients, irrespective of CL wear. The CL wearer however, presents a challenge to the practitioner, because both elements of physical and visual comfort must be considered to be able to fully understand and manage the patient.
Although no single definition of visual comfort exists, there are similarities between descriptions. Here, visual comfort is defined as ‘the feeling of ease, well-being, or satisfaction with the visual environment.’ It has also been defined as ‘the subjective impression of comfort caused by visual stimuli’.21 A good example of the impact of visual discomfort is the fact that in the US it is listed as a condition with applicable signs and symptoms for diagnosis in the international classification of disease (ICD-10) codes used for medical insurance billing purposes.22
The sensations experienced by the patient when visual discomfort or eyestrain occurs range from feeling pain, to ache or tiredness around the eyes. Blurred or diplopic vision, headache and ocular fatigue may also be experienced. Blurred vision has long been associated with visual discomfort,23 and uncorrected astigmatism has been found to be a major cause of eyestrain, headache and tired eyes.24-26 Accommodative and vergence anomalies are also sources of eyestrain.27-30 Oculomotor imbalances resulting from poorly compensated phorias also contribute to eyestrain.
Squinting is possible in response to blurred vision or extraneous light sources, and involves constriction of the orbicularis oculi muscle (figure 2). Significant correlation between discomfort and blood flow to this muscle has been shown, and suggests that pain around the eye may result from over activation of the orbicularis while squinting.24 Prolonged constriction of the corrugator supercilli muscle near the eyebrows has also been associated with migraine headaches, likely due to compression of the supraorbital and supratrochlear nerves that run through it.31

Figure 2: A reaction to bright light
The contrast of the target,32 text size,33 and cognitive demand 34 of the task also contribute to visual comfort. Blink rates have been shown to reduce with near tasks35,36 and incomplete blinks have been correlated with discomfort.37 The evidence for pupil constriction being a source of pain remains equivocal, with a number of studies reporting that pupil constriction does not directly cause discomfort,38-40 and a recent study suggesting a more causal relationship.41 Irrespective of a direct link, pupil constriction is of course related to accommodation and convergence, and sustained near tasks place strain on this triad of close focusing systems.
Digital devices
Many of the additional factors associated with visual discomfort arise from the type of near task performed. While reports of visual discomfort can be found in literature dating back many hundreds of years, most relevant in today’s modern society are those tasks completed on digital devices. It has been found that the magnitude of ocular symptoms are significantly higher when viewing digital displays compared to printed materials.42 Vision-related symptoms arising from the use of digital devices include eyestrain, blurred vision, dry eye, headache and discomfort.42
The use of digital devices is widespread: a 2017 survey of US adults showed just over three-quarters of Americans own a smartphone, with even higher penetration among the 18 to 29-year-old age group of 92%.43 The term ‘computer vision syndrome’ (CVS) characterises a group of ocular and non-ocular symptoms, and when this complete range of symptoms are taken in account, a prevalence of CVS of 90% has been reported.44 The use of CVS to describe symptoms is gradually reducing in favor of the newer descriptor ‘digital eyestrain’.45 A survey of New York office workers found 40% reported ‘tired eyes’ at least half the time, with nearly a third (31%) reporting ‘eye discomfort’ at the same frequency.46
The type of device used varies, from desktop VDU screens, through to laptops, and handheld devices. Each of these are used at different viewing distances and gaze angles, at different times of day, under different ambient illumination and in varied environments. This presents a complex range of demands to the visual system (figure 3).

Figure 3: Modern digital devices pose a definite challenge to the visual system
Photophobia
Visual discomfort can also be attributed to several ocular and systemic diseases, and medications. Photophobia is a cause of visual discomfort and is defined as ‘a sensory state in which light causes discomfort in the eye or head; it may also cause an avoidance reaction without overt pain’.47 Photophobia is associated with dry eye, migraine, depression, blepharospasm, progressive supranuclear palsy and the use of medications such as barbiturates and benzodiazepines.47 Photophobia is linked to pain sensation, with functional magnetic resonance imaging (fMRI) recordings showing a pattern of activation which suggests photophobia is perceived as a true pain stimulus.48
Glare
We are all susceptible to being troubled by excessive light levels: just think of how we shield the eyes from the sun on a bright day, or how uncomfortable we find oncoming headlights when driving at night (figure 4). Viewing bright lights can cause the eye to respond with squinting and pupil constriction, which may lead to visual fatigue and discomfort. It is also common to deal with uncomfortable light levels by averting the eyes.

Figure 4: An example of a compensating behaviour when eyes are challenged by light
The American National Standard Practice for Office Lighting (ANSI) states that ‘glare occurs when luminances, or luminance ratios are excessively high in relation to the state of adaptation’ (ANSI/IES RP 1-12). Luminous ratio is the luminance of the glare source divided by the luminance of the target. The ANSI standard states that the luminance ratio should not exceed 10:1 for remote light or more than 3:1 between the target and immediate visual surroundings. Use of sunglasses does not change the luminous ratio, however viewing through sunglasses feels more comfortable because overall retinal illumination has been reduced. This moves the exposure below the borderline luminance between visual comfort and discomfort (binary-code decimal or BCD value). The BCD value is commonly used by lighting engineers and architects when determining the optimum, comfortable levels of illumination for a room.
Glare reduces both contrast sensitivity,49 and high and low contrast acuity.50-52 It is generally categorised into two types. Disability glare is ‘a temporary impairment of vision due to light’ and is caused by loss of retinal image contrast resulting from intraocular light scatter.53 Discomfort glare is ‘a transitory irritation caused by light’ and may be a response to the saturation of visual neurons.53 In addition to the luminous ratio, and the size and distance to the light source, a number of other factors contribute to discomfort glare. Awareness of these factors, summarised in table 3, enables better advice to be offered to the patient troubled by glare-induced visual discomfort.
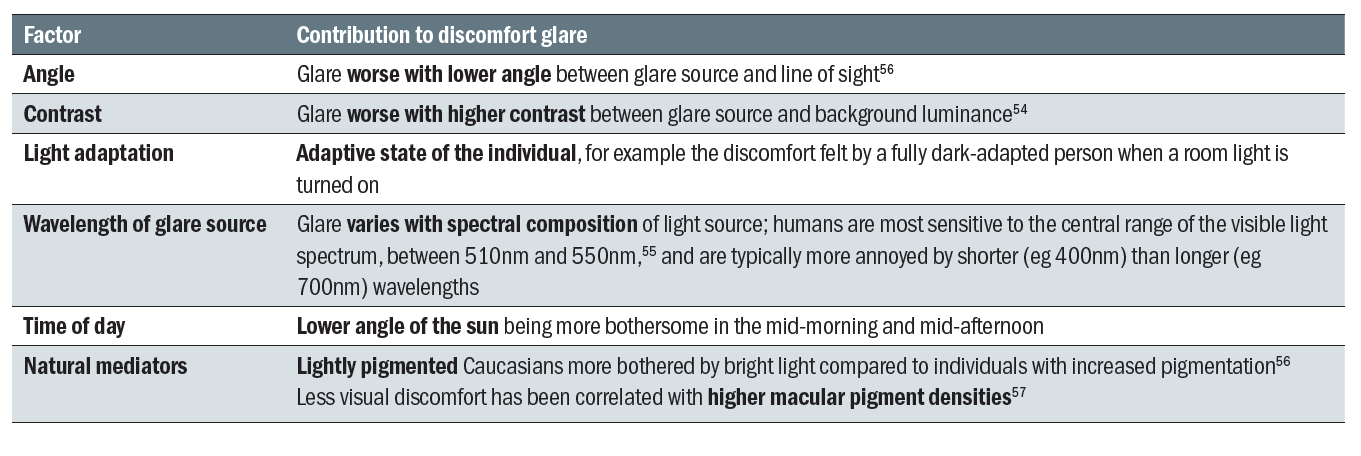
Table 3: Factors that contribute to discomfort glare
Compensating behaviors
A number of compensating behaviors are employed to help mediate visual discomfort. Squinting occurs in relation to uncorrected refractive error, binocular vision imbalances, and glare. Excess light is often blocked by a hand shielding the eyes or use of sunglasses (figure 4). The compensating behavior particularly associated with glare is avoidance. Examples of this include looking away from car headlights at night, or flipping down the visor when driving towards low setting sun.
Overlap between physical and visual discomfort
Figure 1 listed the physical and visual factors that contribute to overall comfort when wearing CLs. In reality of course, these factors may overlap. In a survey of habitual reusable CL wearers 59% reported a decline in comfort, overall lens satisfaction and vision quality over the course of the day.58 Of this ‘declining’ group, the most commonly described symptoms were ‘tired eyes’ and ‘dry eyes’. The former refers to a visual factor, the latter to a physical sensation. Changes to the tear film could provide part of the explanation for these overlapping sensations of discomfort: CL wear promotes a more unstable tear film which can lead to both discomfort, dryness and fluctuations in vision.59
Overlap between comfort and vision was investigated in a study which looked at the influence of vision on ocular comfort ratings.60 Under some circumstances comfort was reduced with induced visual blur, and the authors suggested complex psychological influences and higher-order sensory integration of vision and pain processes may be involved.
Conclusion
In terms of what is best for our patients, it is important to be aware that discomfort can manifest as both physical and visual sensations. Recognising the total comfort experience consists of both elements allows us to elicit better information from our patients, and from that, to make more useful recommendations to manage their discomfort. While we may regularly ask our CL wearers ‘how comfortable their lenses feel’, we have an opportunity to also enquire about ‘how comfortably they can see’.
Comfort and discomfort in CL wear is driven by multiple factors, which can overlap and influence each other. It is important to take a methodical approach to management. Follow best practice guidelines for addressing physical CL discomfort, and provide appropriate visual correction and advice on near focusing and light management to help optimise visual comfort. In so doing, the practitioner will help improve the patients’ overall CL experience, satisfaction, potentially reduce drop out and increase recommendation.
Future CL technology may be developed to aid some of these issues. For example, in addition to providing UV-blocking, it may be possible for a CL to selectively filter light to enhance visual performance. Remembering that in the field of ergonomics, comfort is only achieved when something additional is experienced, perhaps we can hope for future CL technology to not only avoid feelings of ‘discomfort’, but actually to deliver enhanced visual and physical comfort for the wearer.
John Buch, OD, MS, FAAO is Principal Research Optometrist, Greg Hofmann is Principal Engineer New Products and David Ruston BSc FCOptom DipCL, FAAO is Director Global Professional Education and Development at Johnson & Johnson Vision.
Key points
- Overall contact lens experience is influenced by both physical and visual comfort
- Ask not only ‘how do your lenses feel?’ but also ‘how comfortably can you see?’
- To improve physical comfort, apply a methodical approach to addressing issues
- Visual comfort is often related to specific tasks or environmental conditions
- To maximise visual comfort, advise on proper viewing techniques for near tasks and digital devices, correct any binocular imbalance and pay attention to glare sources in the patient’s environment
- In the future, it may be possible to deliver enhanced visual and physical comfort for the CL wearer
This publication is similar to the article ‘Getting into your comfort zone’ that appeared in the July 2018 issue of Contact Lens Spectrum and is used with permission given by PentaVision LLC.
References
- Vink P, Hallbeck S. Editorial: comfort and discomfort studies demonstrate the need for a new model. Applied ergonomics. Mar 2012;43(2):271-276.
- Helander MG, Zhang L. Field studies of comfort and discomfort in sitting. Ergonomics. Sep 1997;40(9):895-915.
- Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye & contact lens. Jan 2013;39(1):93-99.
- Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. Feb 2007;26(2):168-174.
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Contact lens & anterior eye: the journal of the British Contact Lens Association. Feb 2017;40(1):15-24.
- Nichols KK, Redfern RL, Jacob JT, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Definition and Classification Subcommittee. Investigative ophthalmology & visual science. 2013;54(11):TFOS14-19.
- Dumbleton K, Caffery B, Dogru M, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Subcommittee on Epidemiology. Investigative ophthalmology & visual science. 2013;54(11):TFOS20-36.
- Guillon M. Are silicone hydrogel contact lenses more comfortable than hydrogel contact lenses? Eye & contact lens. Jan 2013;39(1):86-92.
- Jones L, Brennan NA, Gonzalez-Meijome J, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design, and care subcommittee. Investigative ophthalmology & visual science. Oct 2013;54(11):TFOS37-70.
- Stapleton F, Tan J. Impact of Contact Lens Material, Design, and Fitting on Discomfort. Eye & contact lens. Jan 2017;43(1):32-39.
- Coles MC, Brennan NA. Coefficient of friction and soft contact lens comfort. Optometry and vision science: official publication of the American Academy of Optometry. 2012;89:e-abstract # 125603.
- Maissa C, Guillon M, Garofalo RJ. Contact lens-induced circumlimbal staining in silicone hydrogel contact lenses worn on a daily wear basis. Eye & contact lens. Jan 2012;38(1):16-26.
- González-Cavada J, Corral O, Niño A, Estrella M, Fuentes J, Madrid-Costa D. Base curve influence on the fitting and comfort of the senofilcon A contact lens. Journal of optometry. 2009;2:90 - 93.
- Lazon de la Jara P, Papas E, Diec J, Naduvilath T, Willcox MD, Holden BA. Effect of lens care systems on the clinical performance of a contact lens. Optometry and vision science: official publication of the American Academy of Optometry. Apr 2013;90(4):344-350.
- Diec J, Evans VE, Tilia D, Naduvilath T, Holden BA, Lazon de la Jara P. Comparison of ocular comfort, vision, and SICS during silicone hydrogel contact lens daily wear. Eye & contact lens. Jan 2012;38(1):2-6.
- Riley C, Young G, Chalmers R. Prevalence of ocular surface symptoms, signs, and uncomfortable hours of wear in contact lens wearers: the effect of refitting with daily-wear silicone hydrogel lenses (senofilcon a). Eye & contact lens. Dec 2006;32(6):281-286.
- Chalmers RL, Begley CG, Moody K, Hickson-Curran SB. Contact Lens Dry Eye Questionnaire-8 (CLDEQ-8) and opinion of contact lens performance. Optometry and vision science: official publication of the American Academy of Optometry. Oct 2012;89(10):1435-1442.
- Papas EB, Ciolino JB, Jacobs D, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the management and therapy subcommittee. Investigative ophthalmology & visual science. Oct 2013;54(11):TFOS183-203.
- Papas EB, Tilia D, Tomlinson D, et al. Consequences of wear interruption for discomfort with contact lenses. Optometry and vision science: official publication of the American Academy of Optometry. Jan 2014;91(1):24-31.
- Navascues-Cornago M, Morgan PB, Maldonado-Codina C. Effect of Three Interventions on Contact Lens Comfort in Symptomatic Wearers: A Randomized Clinical Trial. PloS one. 2015;10(8):e0135323.
- Sagawa K. Visual comfort to colored images evaluated by saturation distribution. Color Res. Appl. 1999;24:313–321.
- International Classification of Diseases (ICD-10). 2017; http://www.icd10data.com/ICD10CM/Codes/H00-H59/H53-H54/H53-/H53.14 Accessed 13dec2017.
- Facts about refractive error. 2010; https://nei.nih.gov/health/errors/errors. Accessed 26nov2017.
- Thorud HM, Helland M, Aaras A, Kvikstad TM, Lindberg LG, Horgen G. Eye-related pain induced by visually demanding computer work. Optometry and vision science: official publication of the American Academy of Optometry. Apr 2012;89(4):E452-464.
- Wiggins NP, Daum KM. Visual discomfort and astigmatic refractive errors in VDT use. Journal of the American Optometric Association. Sep 1991;62(9):680-684.
- Wiggins NP, Daum KM, Snyder CA. Effects of residual astigmatism in contact lens wear on visual discomfort in VDT use. Journal of the American Optometric Association. Mar 1992;63(3):177-181.
- Wee SW, Moon NJ, Lee WK, Jeon S. Ophthalmological factors influencing visual asthenopia as a result of viewing 3D displays. The British journal of ophthalmology. Nov 2012;96(11):1391-1394.
- Sheedy JE, Parsons SD. The Video Display Terminal Eye Clinic: clinical report. Optometry and vision science: official publication of the American Academy of Optometry. Aug 1990;67(8):622-626.
- Jaschinski W. The proximity-fixation-disparity curve and the preferred viewing distance at a visual display as an indicator of near vision fatigue. Optometry and vision science: official publication of the American Academy of Optometry. Mar 2002;79(3):158-169.
- Karania R, Evans BJ. The Mallett Fixation Disparity Test: influence of test instructions and relationship with symptoms. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians. Sep 2006;26(5):507-522.
- Dirnberger F, Becker K. Surgical treatment of migraine headaches by corrugator muscle resection. Plastic and reconstructive surgery. Sep 1 2004;114(3):652-657; discussion 658-659.
- Gowrisankaran S, Sheedy JE, Hayes JR. Eyelid squint response to asthenopia-inducing conditions. Optometry and vision science: official publication of the American Academy of Optometry. Jul 2007;84(7):611-619.
- Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians. Sep 2011;31(5):502-515.
- Himebaugh NL, Begley CG, Bradley A, Wilkinson JA. Blinking and tear break-up during four visual tasks. Optometry and vision science: official publication of the American Academy of Optometry. Feb 2009;86(2):E106-114.
- Portello JK, Rosenfield M, Chu CA. Blink rate, incomplete blinks and computer vision syndrome. Optometry and vision science: official publication of the American Academy of Optometry. May 2013;90(5):482-487.
- Patel S, Henderson R, Bradley L, Galloway B, Hunter L. Effect of visual display unit use on blink rate and tear stability. Optometry and vision science: official publication of the American Academy of Optometry. Nov 1991;68(11):888-892.
- Jansen ME, Begley CG, Himebaugh NH, Port NL. Effect of contact lens wear and a near task on tear film break-up. Optometry and vision science: official publication of the American Academy of Optometry. May 2010;87(5):350-357.
- Gray LS, Gilmartin B, Winn B. Accommodation microfluctuations and pupil size during sustained viewing of visual display terminals. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians. Jan 2000;20(1):5-10.
- Hopkinson RG. Glare Discomfort and Pupil Diameter. J. Opt. Soc. Am. 1956/08/01 1956;46(8):649-656.
- Fry GA, King VM. The Pupillary Response and Discomfort Glare. Journal of the Illuminating Engineering Society. 1975/07/01 1975;4(4):307-324.
- Lin Y, Fotios S, Wei M, Liu Y, Guo W, Sun Y. Eye Movement and Pupil Size Constriction Under Discomfort Glare. Investigative ophthalmology & visual science. 2015;56(3):1649-1656.
- Chu C, Rosenfield M, Portello JK, Benzoni JA, Collier JD. A comparison of symptoms after viewing text on a computer screen and hardcopy. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians. Jan 2011;31(1):29-32.
- Smith. A. Record shares of Americans now own smartphones, have home broadband. 2017; Pew Research Center. Available at: http://www.pewresearch.org/fact-tank/2017/01/12/evolution-of-technology/. Accessed 25th Jan, 2018.
- Thomson WD. Eye problems and visual display terminals--the facts and the fallacies. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians. Mar 1998;18(2):111-119.
- Hall L, Brennan-Coles C. More screen time = more digital eye strain. Contact Lens Spectrum. June 2015;30:38-40.
- Portello JK, Rosenfield M, Bababekova Y, Estrada JM, Leon A. Computer-related visual symptoms in office workers. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians. Sep 2012;32(5):375-382.
- Digre KB, Brennan KC. Shedding light on photophobia. Journal of neuro-ophthalmology: the official journal of the North American Neuro-Ophthalmology Society. Mar 2012;32(1):68-81.
- Moulton EA, Becerra L, Borsook D. An fMRI case report of photophobia: activation of the trigeminal nociceptive pathway. Pain. Oct 2009;145(3):358-363.
- Harrison JM, Applegate RA, Yates JT, Ballentine C. Contrast sensitivity and disability glare in the middle years. Journal of the Optical Society of America. A, Optics, image science, and vision. Aug 1993;10(8):1849-1855.
- Bailey IL, Bullimore MA. A new test for the evaluation of disability glare. Optometry and vision science: official publication of the American Academy of Optometry. Dec 1991;68(12):911-917.
- Regan D, Giaschi DE, Fresco BB. Measurement of glare sensitivity in cataract patients using low-contrast letter charts. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians. Apr 1993;13(2):115-123.
- Haegerstrom-Portnoy G, Schneck ME, Brabyn JA. Seeing into old age: vision function beyond acuity. Optometry and vision science: official publication of the American Academy of Optometry. Mar 1999;76(3):141-158.
- Mainster MA, Turner PL. Glare’s causes, consequences, and clinical challenges after a century of ophthalmic study. American journal of ophthalmology. Apr 2012;153(4):587-593.
- Applegate RA, Wolf M. Disability glare increased by hydrogel lens wear. American journal of optometry and physiological optics. May 1987;64(5):309-312.
- Fekete J, Sik-Lanyi C, Schanda J. Spectral discomfort glare sensitivity investigations. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians. Mar 2010;30(2):182-187.
- JK IJ, de Waard PW, van den Berg TJ, de Jong PT. The intraocular straylight function in 129 healthy volunteers; dependence on angle, age and pigmentation. Vision research. 1990;30(5):699-707.
- Stringham JM, Garcia PV, Smith PA, McLin LN, Foutch BK. Macular pigment and visual performance in glare: benefits for photostress recovery, disability glare, and visual discomfort. Investigative ophthalmology & visual science. Sep 22 2011;52(10):7406-7415.
- Mathews K DB, Alford et al. Exploring variability in soft contact lens performance. Optician. 2015;251(6543):32-34.
- Craig JP, Willcox M, ArgÜeso P, Maissa C, Stahl U, Tomlinson A, Wang J, Yokoi N, Stapleton F. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens interactions with the tear film subcommittee. Invest Ophthalmol Vis Sci 2013;54:TFOS123-56
- Rao SB, Simpson TL. Influence of Vision on Ocular Comfort Ratings. Optometry and vision science: official publication of the American Academy of Optometry. Aug 2016;93(8):793-800.
