Essential Contact lens practice series
- Insights into contact lens wear
- History and symptoms
- Initial examination 1 – refraction and corneal assessment
- Initial examination 2 – slit lamp
- The tear film in contact lens wear
- Contact lens selection
- Soft contact lens fitting
- Soft toric contact lens fitting
- Managing the presbyope
- Rigid contact lens fitting
- Instruction and compliance
- The aftercare
- The future for contact lenses
The contact lens market is full of potential. We arguably have the widest range of soft lens materials, modalities and parameters available than ever before. With this vast soft lens availability to support the smaller rigid gas permeable market, more patients than ever can find a contact lens which best meets their individual needs. Alongside this, high profile marketing campaigns and public relations activity have served to increase public awareness. Yet, despite these advances, penetration within the UK remains at approximately 16%, a figure which is just under two thirds that of the US.1 The availability of better contact lens products brought about by advances in technology is most certainly creating an impact, but, the UK contact lens market grows only slowly year on year indicating that there is still significant opportunity for growth.
Research suggests there are somewhere in the region of 20 million spectacle wearers in the UK, of which about 4.1 million are also contact lens wearers. More interestingly, there are around 15 million patients who would be open to trying contact lenses.1 It is staggering to think there are more people considering being contact lens wearers than there are actual wearers. The market figures would appear to indicate that we are not identifying these millions of potential contact lens wearers in our midst, suggesting we must pay closer attention to our patients’ visual correction needs.
Equally, while marketing campaigns strive to recruit new wearers, the contact lens market is a known ‘leaky bucket’ and research suggests that for every new wearer we recruit, just as many drop out of contact lens wear.1 The key to a healthy contact lens market must lie in the successful identification of all potential considerers, but also in the early detection and appropriate management of the patients at risk of leaving contact lens wear behind.
Identifying Patient Needs
In 2016 the General Optical Council launched its Standards of Practice replacing the previous Code of Conduct defining the levels of expected behaviour and performance for registrants. The 19 listed standards begin with two key elements which can seek to address some of these contact lens patient concerns:
- Listen to patients and ensure they are at the heart of the decisions made about their care.
- Communicate effectively with your patients.
Eye care professionals are encouraged to fully listen to patients and to take account of their individual views, preferences and concerns, with an emphasis on allowing sufficient time to deal properly with patient needs. Great communication lies at the heart of any consultation and these standards reiterate the importance of clear and honest discussions, ensuring the patient is always welcome to ask questions where appropriate.
Now, more than ever, the expectation of the profession is to provide support, expertise and a chance to ensure that any patients’ unmet needs are identified and addressed.
Communication is so much more than words, and while an eye care practitioner may not intentionally set out to do a ‘bad job’, research repeatedly indicates that we are not doing as well as we might suspect, particularly where the field of contact lenses is considered. In fact, 66% of patients do not feel well informed about contact lenses and over half of our contact lens ‘considerers’ wish their eye care professional would talk to them more on the topic.2 Listening to the patient and putting them at the heart of the decisions made about their care can only seek to rectify the disparity within these statistics. Sufficient time should be spent with each patient to create the rapport needed to successfully ascertain their specific visual correction requirements.
Understanding what drives someone to consider contact lenses requires identification of their specific patient needs. Keeping a patient as a successful contact lens wearer requires an understanding of changing needs or identification of situations whereby those needs are no longer being met.
Benefits of Contact Lens Wear
Contact lenses are fundamentally a form of vision correction, so the simple benefit of clear vision cannot be overlooked. However, vision is most often defined by what can be resolved on an acuity chart assessment, but in reality, ‘good vision’ is so much more than that. For example, there is an improvement in field of view with contact lenses over spectacles in many cases. Patients with high powered spectacle prescriptions are often recommended smaller frames to achieve a good cosmetic outcome – but this can impede peripheral vision. It is also worthwhile remembering that spectacle minification occurs in high minus powers, often rendering a patient with ‘better’ vision in contact lenses. Contact lenses are a recognised excellent alternative for anisometropic patients who could struggle with the differential image sizes that their prescription creates. Research has also shown that contact lenses may reduce amplitude and frequency of nystagmus in some patients 3 and it has been suggested that a contact lens may be the preferred corrective option here as a contact lens will move with the eye 4 potentially creating visual stability.
Alongside the visual benefits, there are many reasons why a contact lens recommendation may be appropriate, and there are many recognisable ‘flags’ which may prompt a discussion. A desire or need to wear contact lenses for sports or hobbies can provide important motivation and create an obvious and clear benefit, giving an easy way to begin a contact lens conversation. Certain occupations may generate discussion about contact lens suitability, as will many other lifestyle requirements. Most practitioners would feel that these recognisable lifestyle and recreational activities should generate, at the very least, a suggestion of a contact lens option.
Other more subtle clues may also highlight a patient as a considerer, whereby contact lens wear could provide a real benefit. A patient who openly admits that they do not like spectacles, or ‘only uses them when they absolutely have to’ may also be sending out a signal for an alternative option. An increase in reliance on the spectacles or a change in wearing habit may also elicit a contact lens need.
Contact Lens Considerers
It would be so much easier if each person considering contact lenses simply asked for them, but we know that this has never been, and is unlikely to ever be the case. There is often so much information to discuss at the end of an eye examination that contact lens recommendation may not be top of mind. Sadly, the situation will often arise whereby the professional assumes that if the patient wanted contact lenses – they would ask about them. Conversely, the patient assumes that if they were a suitable option, the professional would have mentioned them. It is, however, a vicious cycle, as the eye care professional not mentioning contact lenses is cited as one of the main reasons consumers give for not taking any steps towards getting them.5 The vast majority of considerers would simply appear to be waiting for us to recommend contact lenses as an option.
With the significant improvements in contact lens parameters and materials, considerers will lie at both ends of the population demographic and practitioners may find the need to rethink ‘who’ they really listen for these clues from. Improvements in parameters and materials also re-opens the door to previous contact lens wearers who now may be satisfied with new products. This highlights the need for eye care practitioners to keep up to date with new additions to the contact lens market.
There is often a difference in how a practitioner feels about fitting contact lenses, and the actual contact lens wearing population. For example, in the UK, ECPs feel the minimum age they would be happy to fit contact lenses for is nine years old, yet only 3% of current contact lens wearers tell us they started under 15 years of age.6,7 These numbers would suggest that while a practitioner may be happy to fit a nine-year-old with contact lenses, they may not be actively recommending to this age group. The key to converting these considerers, and any others, may simply lie in an open conversation.
The benefit of contact lenses in children expands to include a social benefit. The Adolescent and Child Health Initiative to Encourage Vision Empowerment (ACHIEVE) study considered the quality of life improvements associated with contact lens wear in children. In a study of eight to 11 years old myopic children, physical appearance, athletic competence and social acceptance self-perceptions were shown to improve with contact lens wear.8
At the opposite end of the potential wearer demographic, we should also mention the onset of presbyopia at this point. Over a third of contact lens considerers are presbyopic, even though this may not appear to fit the mould of a new contact lens wearer.1 Statistics demonstrate that whilst the percentage of spectacle wearers in the 45+ age group steadily rises with age, the contact lens wearing percentage reflects a corresponding decline (figure 1).7 Yet, in a study where presbyopic patients were given the choice between contact lenses and spectacles, 78% of patients said they would prefer a combination of the two.9
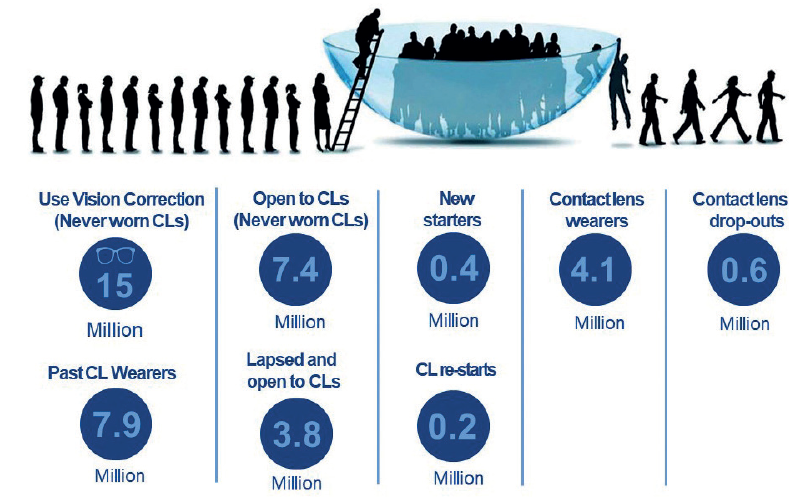
Figure 1: The UK contact lens market in 20171
Identifying the contact lens considerers does, however, go above and beyond the simple identification of an appropriate hobby or lifestyle requirement. While just 16% of the UK vision correction users wear contact lenses,1 research indicates that there is more to contact lens wear than simple vision correction.10 Motivation comes in many forms and whilst rational benefits such as clear vision and convenience may be the presenting need, these elements can be considered ‘surface drivers’ or rational drivers, and only represent a relatively small proportion of the motivation. A more significant proportion (two thirds), of the motivational drivers have been shown to be emotional in origin, promoting self-confidence and a sense of belonging.10 This is where great communication skills become invaluable as a patient is less likely to share these deeper emotional elements with a practitioner if there is not a comfortable rapport.
When considering these emotional drivers, it can be useful to consider how life simply ‘changes’ over time. People change and so do the things that they want or need. An awareness of designer high fashion sunglasses may suddenly appear overnight and become the only thing a patient wants to be seen in. Their faithful prescription sunglasses may simply no longer suffice. A change in personal circumstance may promote the desire for a ‘new look’, or an increased reliance on spectacles may provide frustrations in certain circumstances. It would be a happy coincidence if any change to a patient’s life happened at the exact same time as their next routine appointment was due, but we know that this is not going to be the case. Ironically, it may also be emotional reasons holding the patient back from starting the conversation. There are deeper emotional elements here too – some patients may fear being judged as vain or shallow for initiating a conversation around simply changing their look. They may present stating one need, such as a desire to use them for sport, to avoid the conversation around a deeper more emotional need.
Initial patient interactions during history and symptoms are essential to a successful examination but will often identify only the ‘top line’ needs. The real skill in identifying a potential contact lens wearer comes from really understanding what would motivate an individual to wear them and this goes above and beyond the instantly obvious ‘practical’ reasons which are so easy to identify from basic questioning. Building a relationship which encourages open and honest discussion about contact lens possibilities both currently and beyond into the future, is what will help ensure that we really understand our patient’s needs.

Figure 2: Contact lens penetration compared to the percentage of the population who require vision correction versus age
Keeping the contact lens wearer happy
Much of the promotion of contact lenses in the practice environment targets the potential new wearer and while we must strive to build this further by identifying the millions of considerers, the issue of contact lens drop-out must also be addressed. As much as a life changing event may trigger an interest in contact lenses, the same can be said for the reverse. When the contact lens ceases to meet the patient needs, motivation to continue wear reduces. The identification of changing wants and needs not only applies to chasing the new wearer but maintaining our existing contact lens wearers too. Life is not static in its demands, and a contact lens wearer may need several adaptations to their lens to address their changing requirements. In the same way that a patient may assume that if they were suitable for contact lenses, the practitioner would mention them, an existing contact lens wearer may assume there are no alternative options available if these are not discussed.
Patients can initially be very accepting of subtle inconsistencies in their needs being met, maybe assuming that end of day discomfort is part and parcel of contact lens wear – or that it is normal to need to blink hard to see clearly. While these issues might initially be infrequent and not too bothersome, they may build and impact the patient more often. Wearing hours may reduce, followed by fewer days in contact lenses, ultimately the cessation of contact lens wear altogether may occur. The Tear Film and Ocular Surface (TFOS) International Workshop on Contact Lens Discomfort 11 proposed a progression for the stages of discomfort, starting with ‘strugglers’ experiencing early symptoms and concluding ultimately with permanent dropout (figure 3).

Figure 3: Progression of contact lens discomfort. Adapted from TFOS.12
These vanishing contact lens wearers can slip under the radar as those that cease contact lens wear will rarely make an appointment just to share this news with you; they simply disappear.
So, what leads to the discontinuation of contact lens wear? Put bluntly, for a myriad of potential reasons, the contact lens may no longer meet the needs of the patient. When the perceived benefit of the contact lens reduces – maybe due to increasing comfort issues, or the ‘hassle’ of the care regime, or if the wearer’s motivation alters and changes – it does not matter if the wearer is new to contact lenses, or an established wearer – the end point is the same. When the benefit of the contact lenses are no longer obvious to the wearer, they will reduce lens wear and could ultimately drop out of lens wear altogether.
With this in mind, it is, however, useful to consider why patients at different stages in their contact lens journey may cease to find the benefits of contact lens wear, or lose sight of the motivation that drew them to contact lenses initially. Studies looking at retention of the new contact lens wearer provide some interesting insight.12,13 When patients in their first year of contact lens wear are considered, 26% ceased lens wear within this period (figure 4). More significantly, of those that do drop out, nearly half did so in the first two months. It is often assumed that handling problems contribute to new wearer drop out, and this was cited as the most common reason for spherical lens wearers. However, poor vision was cited as the most common reason for early drop out among toric and multifocal new lens wearers. Within these studies,12,13 only a small amount (29%) of patients had an additional trial fitting with a changed power or lens type prior to dropping out of contact lens wear altogether. It would seem that a better understanding as to what to expect in the early stages of contact lens wear could do much to address these issues.

Figure 4: Proportion of new wearers who discontinued lens wear by number of days since dispensing (n=510, for 14 patients time discontinued unknown)13
It is possible today to purchase pretty much anything, at any time of day, with a simple click of a button from wherever you happen to be. The path to successful contact lens wear is more complex than clicking a button and it somewhat lacks the quick fix of so many of life’s commodities. It is essential that a patient understands why this is so and appreciates that this is a product recommended specifically for them and their individual needs, and not something that is simply picked off a shelf. The early stages of the contact lens journey are key to successful contact lens wear and support provided during these initial stages is vital to success.
An established contact lens wearer conversely, is more likely to leave contact lens wear because of comfort concerns. Maintaining comfort is key to long term successful contact lens wear.14 Introducing the notion that a specific type of contact lens may not be a lifelong partner could prove valuable in prompting patient discussion when the world around them changes. A patient needs to feel secure, not only in the knowledge that there will be alternatives should their needs evolve or change, but that their chosen professional can provide the knowledge and support to make these adjustments if they become necessary.
Recommendations
While the need to maintain clinical skills and knowledge clearly forms an essential element of the practitioner-patient interaction, insights tell us that our recommendations are more valuable than we realise. There is a certain expectation from a patient that the clinician will be technically competent to perform the required clinical examinations or have access to the scientific background data supporting the products we choose to use. When considering what drives a patient to make a vision correction purchase, more patients will prioritise ECP expertise over everything else.15 But alongside this is an expectation that the recommendation will be tailored to their individual needs and requirements.
In the world of contact lens fitting, this personalised recommendation is a sum of several parts. The practitioner must firstly strive to fully understand the benefits contact lens wear can bring to the patient and really understand their motivations. This should combine with the clinical skills to evaluate an eye and understand how its individual physiology will impact contact lens wear. A firm understanding of material properties, optical design and how these can influence the potential drop out risk factors of handling, vision and comfort, complements the preliminary investigations and ensures that each recommendation made, is a recommendation truly tailored to the individual patient’s needs. But this approach should not be reserved for the new wearer. The motivation for an established wearer will change over time and if this is not identified and addressed, we risk losing this patient from contact lens wear.
While the default recommendation at the conclusion of an eye examination would seem to be discussion around spectacle correction, it could be argued that full communication of the visual correction options for a large number of patients should also include a contact lens suggestion too.
Increasing the number of contact lens wearers will simply – yet importantly – mean that we are meeting the currently unidentified needs of more of our patients. Creating a successful contact lens wearer is not simply about removing barriers to wear but understanding potential motivations and the specific benefits that contact lens wear will bring.
Top Tips for Introducing Contact Lenses to Your Patients
- Offer contact lenses to patients as an aid to spectacle dispensing.
- Present contact lenses and spectacles as complementary correction options.
- Link contact lens recommendations to patient hobbies so they can immediately see when they would offer benefits over spectacles.
- Increase the visibility of contact lenses in your practice to engage with prospective wearers.
- Educate and motivate the whole team on the benefits of contact lenses, ensuring everyone is kept up to date with the latest developments.
- Use positive and encouraging language such as ‘You’re an excellent candidate for contact lenses’.
Clair Bulpin is an optometrist, assessor and examiner for the College of Optometrists and a paid consultant faculty member for the Johnson & Johnson Institute, UK. Dr Rachel Hiscox is a Professional Education & Development Manager, UK & Ireland, Johnson & Johnson Vision Care. This article is the first in a revised and updated ‘Essential Contact Lens Practice’ series originally authored by Jane Veys, John Meyler and Ian Davies. This article was produced without further input or review from the original authors.
References
- JJV Data on File 2017. Independent Market Research, Global Incidence & Growth Leavers. Penetration defined as percentage of the population who require vision correction who are wearing contact lenses.
- JJV Data on File 2017. Independent Market Research, UK Shopper
- Allen ED , Davies PD . Role of contact lenses in the management of congenital nystagmus. Br J Ophthalmol 1983; 67: 834–836.
- Miller J. Refractions and reflections. Surv Ophthalmol 2004; 49: 436.
- JJV Data on File 2018. Independent Market Research, UK Path to Purchase
- JJV Data on File 2013. Independent Market Research, ECP Claims Study
- JJV Data on File 2017. Independent Market Research, EMA Incidence
- Walline JJ et al; The adolescent and child health initiative to encourage vision empowerment (ACHIEVE) study: design and baseline data. Optom Vis Sci 2006; 83(1):37-45
- Neadle S, Ivanova V and Hickson-Curran S. Do presbyopes prefer progressive spectacles or multifocal contact lenses? Cont Lens Ant Eye, 2010;33:262-263
- JJV Data on File 2017. Independent Market Research, Motivations and Barriers Towards Contact Lenses
- Nichols KK, Redfern RL, Jacob JT et al. The TFOS International Workshop on CL Discomfort: Report of the Definition and Classification Subcommittee. Invest Ophthalmol Vis Sci 2013;54: TFOS14-19
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye. 2017;40(1):15-24.
- Sulley A, Young G, Hunt C. Prospective evaluation of new contact lens wearer retention rates. Contact Lens & Anterior Eye, 2018; 41(S1):S4
- Morgan PB. Optimising contact lens wear for a lifetime of use. Optician 2013;245;6400:32-37
- Aslam A. What drives vision correction purchases? Optician (2014) 247; 6458: 16-20.
