For many optometric students and practitioners, binocular vision remains an area of trepidation and uncertainty. There is some justification for this: the binocular system is complex, with numerous interacting components to consider. However, there are in essence a limited number of underlying principles which when understood allow a common-sense approach to the binocular vision conditions that the practitioner is likely to encounter in daily practice.
The purpose of this introductory article (with a series of articles to follow) is to try to clarify these underlying principles, including some of the basic vocabulary and definitions that describe normal binocular vision, which in turn underpins the understanding of what happens when binocular vision fails. This article will only mention in passing clinical conditions or tests that help to illustrate these basic principles.
The follow up articles in this series will look at these clinically important issues in more detail, with particular reference to the commonly presenting scenarios and their optometric management. We shall start with a short consideration of what we mean by the term ‘binocular vision’ and will then consider the issues of sensory and motor fusion in some detail. Virtually all BV problems relate to fusion in some form, hence a proper understanding of this area is essential in trying to understand the patients’ signs, symptoms and needs.
What is Binocular Vision?
There are many potential definitions of the term ‘binocular vision’, but for the purpose of these articles, I will adopt the widely accepted clinical understanding of binocular vision as the condition where, with regards to the monocular visual fields, there is a large area of binocular overlap which is used for the coding of depth.1 The term ‘coding of depth’ can be roughly equated to ‘stereopsis’, the ultimate aim of binocular vision. In this definition, natural viewing conditions are assumed, ie that there are no impediments to either eye. In this state, the eyes are allowed to be associated, as opposed to dissociated, where there is an impediment that abolishes any possibility of binocular vision. For example, occlusion of one eye in the cover test dissociates.
Two fundamental requirements for the extraction of stereoscopic information while in the associated state are the presence of:
- Motor fusion – involves the control of the extra-ocular muscles to adjust eye position to maintain association.
- Sensory fusion – a more abstract concept whereby the brain processes both retinal images in order to extract stereoscopic information.
Compromise of one or both of these two requirements generates the vast majority of binocular vision issues. Although these two distinctly different aspects of binocular vision can be described independently on a theoretical basis, and both have fundamentally different clinical investigations associated with them, we will see that these two components are inextricably linked in normal binocular vision. As one aspect becomes more compromised, so will the other. Indeed, neither aspect can function in the complete absence of the other. Although this interaction may seem like an unwanted complication, it has the hidden benefit that knowledge about one aspect may allow us to infer something about the other, without direct evidence. Perhaps the most important example of this is the fact that observation of motor fusion proves that sensory fusion must be occurring. This gives objective evidence of an otherwise invisible function of the brain.
The importance of understanding motor and sensory fusion and their interactions cannot be underestimated. Understanding these two functions is fundamental to understanding normal binocular vision, and then the signs, symptoms and investigation of compromised binocular vision. These themes underpin and recur throughout this series of articles, and hence will be dealt with in more detail at this early stage.
Sensory Fusion
Confusingly, this term has two meanings. In the broader context, it relates to how the brain deals with the input from two distinct (and often subtly different) retinal images, one from each eye. For clarity, I shall restrict the use of the term ‘sensory fusion’ to this broad meaning. This broad concept can be broken down into a three-stage hierarchy: simultaneous perception, followed by sensory fusion (the second, more specific use of the term: for clarity I shall use the alternative term of flat fusion to mean this specific level in the hierarch of sensory fusion), followed by stereopsis (figure 1). This all occurs invisibly in the cerebral cortex. Typically we rely on our interpretation of the patient’s responses for investigation, ie investigations are subjective. However, demonstration of motor fusion is valid evidence of flat fusion.
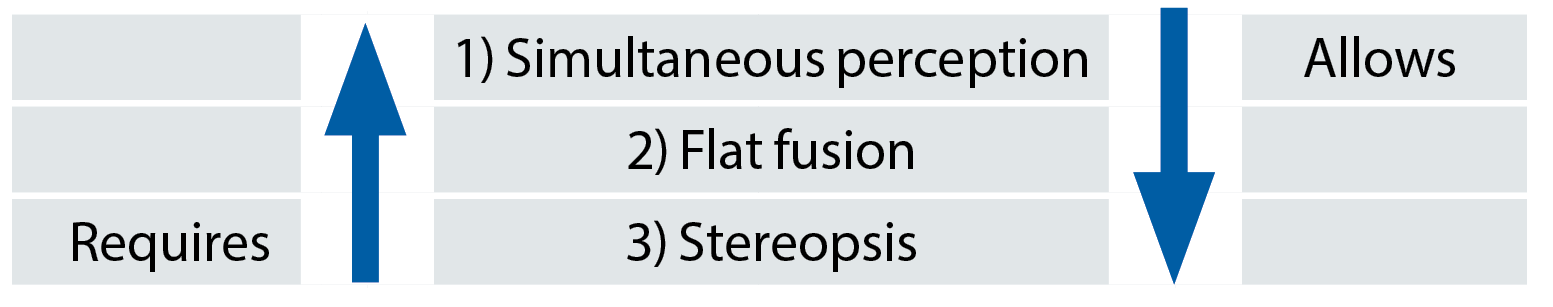
Figure 1: The Sensory fusion hierarchy: 1 allows 2 which allows 3. Demonstrating the absence of 1 obviates testing for 2 or 3. In the opposite direction, 3 requires 2 which requires 1. Demonstrating 3 obviates testing for 2 or 1
By the term simultaneous perception we mean that both retinal images are available to, and used by, the brain at the same time. Simultaneous perception may be abolished by occlusion of one eye, thereby creating a situation where there is only one meaningful retinal image. Alternatively, it may be abolished by suppression, a ‘psychic’ act carried out by the brain, where it selectively processes one retinal image and ignores the other. This typically occurs to eliminate diplopia.
Suppression may be global, ie the whole of one retinal image is suppressed, or local where only part of the retinal image, typically the area around the fovea, is suppressed. While suppressing, the input from one eye totally dominates the other, either in a constant unilateral manner (when the brain perceives through the dominant eye and suppresses the non-dominant eye) or on an alternating basis (where both eyes are similar in dominance, and the brain alternates attention and suppression between the two retinal images).
In the clinical environment, simultaneous perception is most convincingly demonstrated by presenting dichoptic (or nonius) stimuli to the patient. By this we mean that the majority of the visual scene is accessible to both eyes, therefore allowing binocular vision to occur, but selected components of the scene are presented exclusively to the right eye, and other selected components are presented exclusively to the left eye. This is also termed partial dissociation, as the binocular components maintain overall association, but there is a partial impediment to binocularity involving the dichoptic components of the visual scene, ie dissociation on a local basis.
If the patient can see both sets of dichoptic components at the same time, they must have simultaneous perception. If they have adequate vision in each eye to see the targets monocularly, but can only see one set at a time under binocular viewing conditions, they have suppression. Probably the most familiar example of this is the Mallett unit, where the bars are presented dichoptically via the polarised filters, and the rest of the unit and surrounding visual scene is seen binocularly. If all bars are seen, we have simultaneous perception. If only one set is seen, the patient has suppression and if we establish which eye sees which set, we can easily work out which eye is being processed and which is being suppressed. If suppression is alternating, the bars will alternate (figure 2).
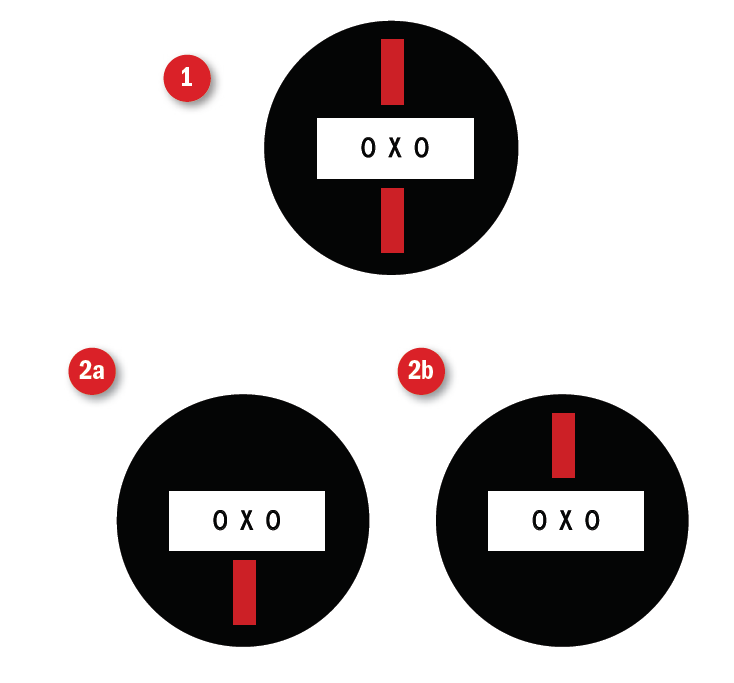
Figure 2: The Mallett Unit illustrating 1) bifoveal vision: 2a and b) suppression of one or other eye. Alternating suppression would alternate between 2a and 2b
There are a number of techniques for generating dichoptic presentations, but clinically they are most commonly created by the following filters:
- Cross-polarised filters – both over the targets and in front of each eye.
- Red and green filters – with the target containing red-only features and green-only features, eg the TNO stereotest.
Indeed, any tests using red/green or polarised filters are probably doing so specifically to generate dichoptic stimuli.
Simultaneous perception can also be confirmed by the appreciation of diplopia, which can be easily demonstrated by introducing significant base-up or base-down prism (for example 10Δ, as used in the von Graefe technique). The vertical shift in one retinal image generates retinal disparity on a global level, ie a difference in position across the whole of the two retinal images (figure 3). If the patient now perceives diplopia, they must have simultaneous perception. If on removal of the prism the diplopia goes away again, then the inference is that the patient has the next level of the hierarchy, flat fusion.

Figure 3: Vertical retinal disparity can be induced by adding vertical prism to one eye via a prism bar or a phoropter head, as here. If the retinal disparity is too great, fusion is broken and diplopia results, demonstrating simultaneous perception and implying flat fusion prior to the diplopia
Flat fusion is where the brain takes the two retinal images and processes them into a single percept. This cannot be confirmed directly: we cannot peer into the brain to see what it is doing, there is nothing we can see or measure to determine whether the single percept the patient is experiencing is due to flat fusion of two images, or suppression of one of the two images. However, there are a number of ways that we can infer that flat fusion is occurring.
One approach is to assess what happens when we attempt to disrupt the presumed flat fusion. When we add vertical prism to demonstrate simultaneous perception, we interrupt flat fusion in order to demonstrate the perception of two retinal images without fusion, ie diplopia. The return to single vision on removal of the prism assumes the restoration of flat fusion. Stronger evidence is given by the demonstration of motor fusion, which we will return to later. Another strong source of evidence is the demonstration of the third layer in the sensory fusion hierarchy, stereopsis.
Stereopsis can be defined as the ‘relative ordering of visual objects in depth’.2 Note that this definition does not exclude depth perception due to monocular cues. These give us information about depth even in the absence of binocular vision. Examples include ‘size of known objects’, where an increase or decrease in retinal image size is interpreted as the object being closer or further away, respectively, rather than larger or smaller, or ‘overlapping contours’ where partial obscuring of one object by a second object suggests that the partially obscured object must be the more remote of the two. Binocular stereopsis is the precise term for depth perception achieved via the processing of the local retinal disparity that occurs between the two slightly different retinal images when different parts of the visual scene are at different distances (figure 4). In the clinical environment, it is this binocular stereopsis that we assess, although we refer to it simply as stereopsis.
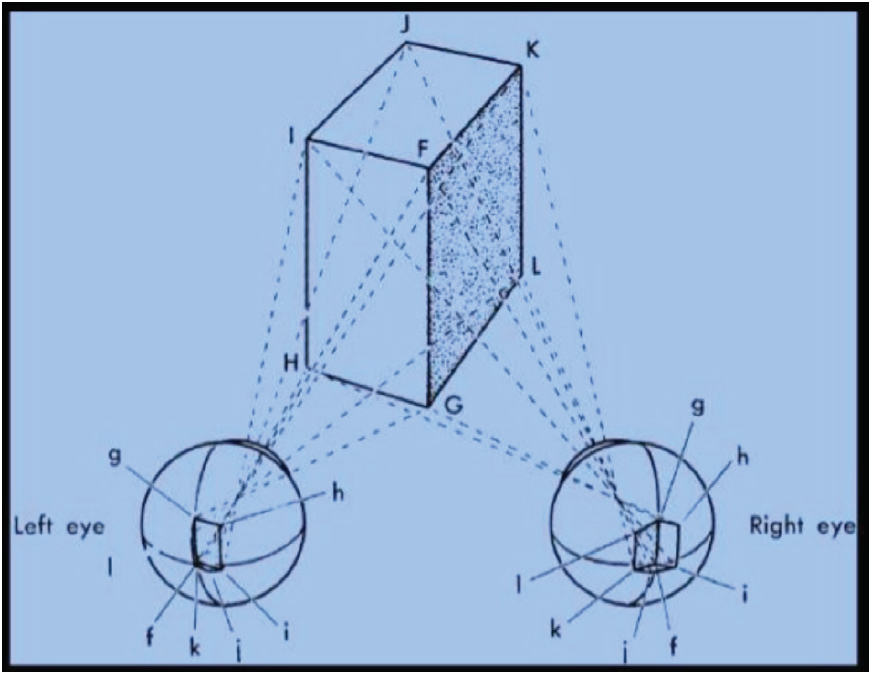
Figure 4: Local retinal disparity for a solid object: points F to I match in location in each eye, but K and L are imaged on different locations, generating retinal disparity
Crucial to our understanding of sensory fusion is the recognition of the significance of this hierarchy: simultaneous perception is a prerequisite of flat fusion which is a prerequisite of stereopsis (figure 1) Therefore, simultaneous perception can occur in isolation (as is the case in diplopia), but flat fusion cannot occur without simultaneous perception. In turn, flat fusion can occur without stereopsis, but stereoscopic information cannot be extracted in the absence of flat fusion. Logically therefore, in the clinical testing environment, if we demonstrate stereopsis we do not need to demonstrate flat fusion or simultaneous perception as they must be occurring. However, if stereopsis is absent we may then need to ascertain if flat fusion or simultaneous perception are present or absent.
Motor fusion
Motor fusion is the act of changing the relative directions of one or both visual axes in order to have both foveae pointing at an object of regard, ie to have bifoveal vision, bifoveality or to be bifoveal. Without it one fovea would not be looking at the object of regard: global retinal disparity and therefore diplopia would occur. In other words, motor fusion exists to facilitate sensory fusion and hence stereopsis. This requires control of the extra-ocular muscles. By definition, any movement of the visual axes that results in a change in their relative alignment is a vergence eye movement, as opposed to version eye movements, where the eyes move in the same direction and the relative alignment of the visual axes remains unchanged.
One example of the need for such a mechanism is the requirement of the visual axes to become more convergent (ie to move the visual axes inwards relative to each other) on a target as it approaches us, or more divergent (to move the axes outwards relative to each other) as it recedes. The maximum
amplitude of convergence (which by convention is given a positive value) is demonstrated when we measure the near point of convergence (NPC), where we encourage the patient to follow a target in towards their nose as far as they can. The maximum amount of divergence (given a negative value) can be demonstrated by gradually adding base-in prism (by prism bar or phoropter head) while looking at a remote target (ie distance negative fusional reserves). Clearly, then, there are limits to the extent of motor fusion. If we go beyond the limits double vision will occur, but even as we approach the limits eyestrain may occur. These are two of the most common symptoms of a struggling vergence mechanism.
There are a number of inputs to this vergence mechanism:
- Tonic vergence – the resting state of the alignment of the eyes in the absence of any other input. It is due to an underlying baseline level of activity in the extra-ocular muscles (activity in these muscles is never zero). Assessing this resting position requires viewing a distant while suspending fusion by dissociation, which can be achieved by the Maddox Rod or the distance cover test. Ideally, the visual axes should be parallel while looking at a distant target: this is often not the case.
- Proximal convergence – awareness of target proximity will automatically stimulate convergence, and the closer the target the greater the convergence response. A change in proximity will also lead to blurring of the retinal image, thereby stimulating a change in accommodation.
- Accommodative convergence – any increase in accommodation in response to a near target also drives the convergence mechanism.
If the combination of proximal and accommodative inputs is appropriate, then axes alignment and bifoveality will be maintained for near vision. The alignment can be assessed with the Maddox Wing or the near cover test. Often, particularly in the elderly, this combined input is inadequate for the chosen target distance, leaving the axes too divergent. In some cases (typically young children) it may overshoot, leaving the axes too convergent.
Any such misalignments of the visual axes, whether at distance or near, will result in a global misalignment of the retinal images and therefore global retinal disparity, resulting in diplopia with the loss of sensory fusion. There is nothing wrong with the muscles or their nerve supply in these cases, it is just that the combined inputs sum up to a vergence position this is inaccurate. However, at this point a further and final crucial input into the vergence mechanism may restore bifoveality: this input is fusional vergence. The stimulus is retinal disparity and the response is a change in the vergence position so as to eliminate this retinal disparity, thereby restoring bifoveality which in turn allows for flat fusion, binocular single vision and hopefully stereopsis. This, in essence, is motor fusion and its role is to facilitate sensory fusion. (Note that due to the lateral displacement of our eyes relative to each other, the above proximal, accommodative and fusional vergence movements were horizontal. Vertical and/or rotational misalignments can also occur, but will only be affected by fusional vergence: the other inputs have no vertical or cyclo influence.)
Ortho and Hetero, Phoria and Tropia
The misalignments of the visual axes described above will result in diplopia in the absence of motor fusion but will result in single vision if motor fusion is present or or there may be no misalignment: we have three separate situations, each of which is clinically important.
The first situation meets the definition of a heterotropia: a manifest deviation not kept in check by fusion.3 This in turn leads to failure of sensory fusion and hence the reporting of diplopia. There is no binocular vision. If, however, motor fusion is present and is able to restore binocularity, then we have a heterophoria: a deviation kept latent by the fusion mechanism.3 The evidence of motor fusion proves the presence of sensory fusion, and there may be stereopsis. The third situation, where there was no manifest or latent deviation, is orthophoria. Note that motor fusion has not been demonstrated in this situation, hence sensory fusion cannot be assumed: orthophoria does not quite guarantee binocular vision. However, the presence of motor fusion can easily be confirmed by the performance of fusional reserves, and the presence of sensory fusion can be confirmed by stereopsis tests. Because the orthophoria and heterophoria groups have no manifest deviation and both display bifoveality with sensory fusion under normal associated viewing conditions, they effectively behave as a single group and can be collectively described as orthotropic in order to distinguish them from the functionally different heterotropic group. For the heterotrope, prism can be applied such that it corrects the deviation, thereby eliminating the retinal disparity and providing bifoveal stimulation by the object of regard. This patient can now be tested for both sensory and motor aspects of fusion, to see whether true binocular vision has been restored, ie we are investigating for binocular potential. Whether or not binocularity can be restored plays a major influence on how we would manage these patients.
Comitant / Incomitant Deviations
Previously it was stated that phorias or tropias were not due to abnormality of the muscles or their nerve supply. Clearly, however such an anomaly could exist, and if one or more of the extra-ocular muscles were compromised, then logically we would expect a misalignment to occur. The resulting deviation would be largest in the direction of gaze that needed the most input from the affected muscle, and would be smallest where it was needed least. This would lead to changing amounts of retinal disparity and therefore changing amounts of diplopia.
Where the deviation is small, motor fusion may still be possible and hence there may be single vision in some directions of gaze but not in others (figure 5). A deviation that changes in size in different directions of gaze is termed incomitant, meaning that the eyes are not moving equally as a pair. This can be highly indicative of pathology. Deviations occurring due to inaccurate input from the vergence components would not change in different directions of gaze, and would be described as comitant or concomitant, ie the eyes do move equally as a pair. Ocular motility testing is designed to distinguish between comitant and incomitant deviations.
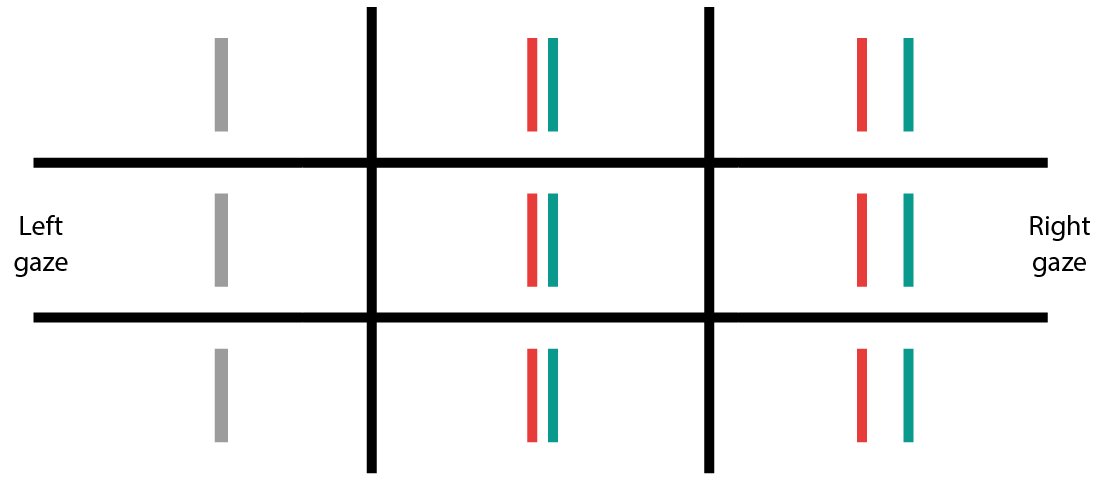
Figure 5: Fusion in an incomitant deviation may be possible in one direction of gaze (to the left in this example of a left medial rectus paresis) but may break down, resulting in diplopia, in the opposite direction. The separation of the images increases as the deviation increases on looking further to the right
Reduced vision and amblyopia
For all situations so far, little mention has been made of the level of visual acuity and the impact that it might have on fusion. Visual acuity is important in two respects.
First, reduced visual acuity will make sensory fusion difficult, especially if the visual acuity is asymmetrical as flat fusion requires two broadly similar retinal images. If sensory fusion is compromised in this way, then motor fusion may become compromised too. This could then lead to a phoria breaking down to a tropia, with the subsequent loss of binocularity.
Secondly, the visual acuity reduction may be due to pathology, or it could be due to amblyopia. This is a condition characterised by reduced visual acuity without any latent or manifest disease of the eye or visual system.4 This is diagnosed by the elimination of refractive error or pathology, and preferably supported by the identification of an appropriate risk factor. The most common risk factors for amblyopia are a constantly blurred retinal image (usually due to uncorrected hypermetropia or astigmatism) or heterotropia that has led to constant suppression of the non-dominant eye in order to eliminate diplopia. The risk factor must be present during the early years of development of the visual system, and if amblyopia is not resolved during these early years, it becomes a lifelong visual impediment to vision and binocularity.
Summary
Understanding motor fusion and sensory fusion is essential to understanding binocular vision and its anomalies: they are the cornerstones of aligning the eyes to generate and maintain matching retinal images, allowing for extraction of detailed information about depth. Compromise of fusion will lead to a reduction in binocular performance. Therefore the ability to assess the state of fusion is essential, and understanding how the range of binocular vision tests available to the clinician do this is crucial. The follow up series to this introduction will relate fusion to common binocular conditions, their investigation, and ultimately management, allowing the optometric practitioner to deal with binocular issues with a little more confidence and a little less trepidation.
Dr Fergal Ennis is a Senior Lecturer (Teaching and Scholarship) at Cardiff University.
References
- Howard, I.P. & Rogers, B.J. (1995) Binocular Vision and Stereopsis. Oxford University Press. New York. 1st ed. page 2.
- von Noorden , G.K. & Campos, E.C. (2002) Binocular Vision and Ocular Motility: Theory and Management of Strabismus. Mosby. St. Louis. 6th ed. page 21.
- von Noorden , G.K. & Campos, E.C. (2002) Binocular Vision and Ocular Motility: Theory and Management of Strabismus. Mosby. St. Louis. 6th ed. page 127.
- Millodot, M. (2000) Dictionary of Optometry and Visual Science. Butterworth Heinmann. Oxford. 5th ed. page 14.
