Cerebral visual impairment (CVI) is considered the leading cause of severe sight impairment (SSI) in children in England and Wales, according to Mitry et al.1 They also noticed that SSI registrations with CVI as the commonest single cause had increased in the first decade of this century. This increase is thought to be due to the improved survival rate of extremely premature infants and those with other causes of brain injury.2,3 Further advances in prenatal, perinatal and postnatal care could potentially help to prevent CVI in the future. This is a form of primary prevention.4
Secondary prevention deals with the early diagnosis and treatment of conditions, as opposed to preventing the pathology in the first place. In the UK, new-borns’ eyes are screened just after birth and vision milestones are checked by the health visitor. The UK National Screening Committee (2013)5 recommends orthoptic-led screening for visual impairment between four and five years of age. This screening is aimed at detecting amblyopia by measuring visual acuities and does not currently include specific screening for CVI. It is the parents’ responsibility to take the child to the community optometrist for regular eye tests.
Tertiary prevention is aimed at managing the child with established visual impairment.4 It is outside the realm of this overview to discuss the specific needs and possible (re)habilitation strategies for children with CVI.
The focus of this article is the optometrist’s role in secondary prevention. Firstly, CVI will be explained. Then the risk factors will be discussed. Finally, some advice will be given for identifying patients who may require further investigation by an ophthalmologist or paediatrician. Although CVI can be acquired at any age, this article will focus on CVI in childhood.
CVI
In the literature, CVI is referred to as ‘cerebral visual impairment’6,7 or ‘cortical visual impairment.’8,9 As yet, there is no internationally accepted definition.10 In this article, the term CVI is used to describe visual impairment as a result of damage to the brain. In order to understand how CVI may affect a person’s visual perception, one has to understand the mechanisms of visual perception in an unaffected brain. This will be discussed first.
Mechanism of Visual Perception
What we experience as ‘seeing’ is in fact our brain’s representation of the outside world. The image from our retina is sent to our brain and the brain combines the visual input with input from different brain areas to form a meaningful image, both for visual perception as well as for visually controlled action. The picture that is created in the brain usually closely matches reality. The different brain processes that are involved in creating an image will be discussed in more detail now.
Starting from the image on the retina, where some information is already processed, the information travels to the occipital lobes. In this area, visual field, colour, contrast, acuity and movement are analysed. From the primary cortex, there are two broad ‘streams’ of projections, known as the ‘ventral stream’ and the ‘dorsal stream’.
- The ventral stream projects towards the temporal lobes where visual memories are stored. This area is responsible for object and face recognition and 3D mapping for way-finding.
- The dorsal stream projects towards the posterior parietal lobes, where the scene in the here-and-now is mapped. This is crucial for seeing the scene as a whole (simultaneous visual perception) and for moving through space (visually guided movement), movement perception and visual attention.
This is a simplified version of the very complex structure of different brain areas that contribute towards visual processing and is meant as an aid to understand some aspects of CVI. Figure 1 shows a schematic tree diagram illustrating these visual pathways and their functions.11 If the brain is damaged, the mental created picture may look rather different from reality and this is sometimes referred to as a child’s altered visual world.
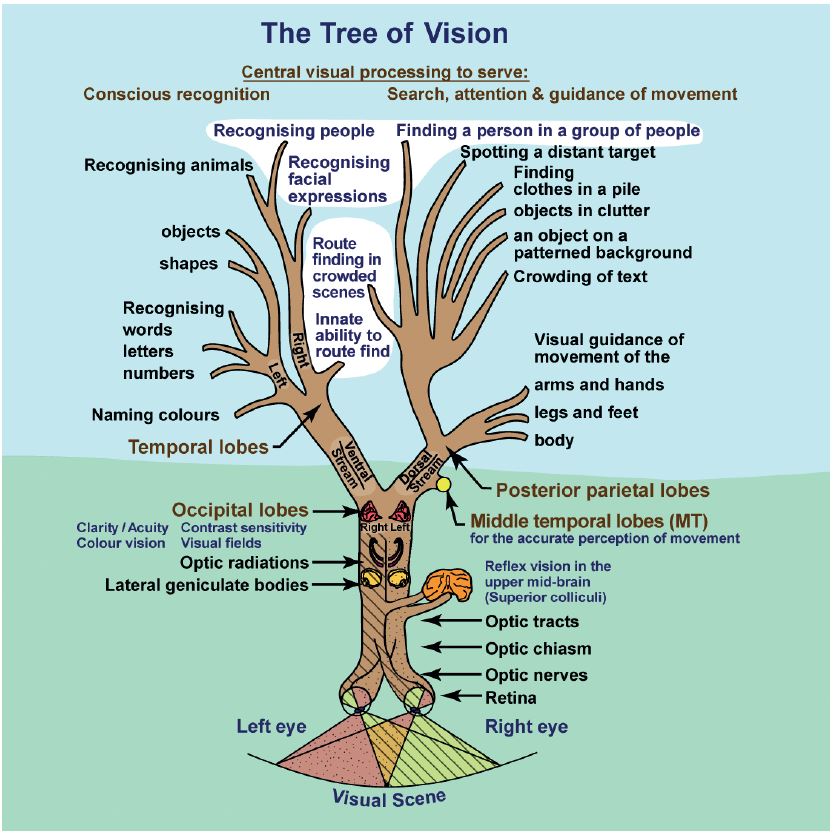
Figure 1: The tree of vision 11
Impact of CVI
For a sighted person it can be difficult to imagine what it is like to have a visual impairment. When the visual impairment is caused by problems in the eye or peripheral visual pathway, the visual limitations are relatively easy to simulate or explain. One can understand or simulate low visual acuity, a scotoma, a loss of contrast sensitivity or visual field defects. It is more challenging to simulate or explain higher visual processing dysfunction.
Patients with CVI are all unique in terms of how their vision is affected. Each affected person has their unique ‘altered visual world’ and it is crucial for (re)habilitation that the child’s parents, carers and teachers take an interest in understanding this unique visual world. Although each child is unique, there is a number of traits that are commonly observed in patients with CVI. Zihl and Dutton provide a helpful list of these difficulties and how these difficulties affect the child’s behaviour as well as adaptations and approaches to overcome these difficulties.12 The categories that deal with higher processing difficulties will be discussed here, along with some examples.
- Perception of movement may be impaired (dyskinetopsia), which can result in children getting startled and upset by small fast-moving animals. Children may also experience difficulties in ball sports due to an inability to see the ball when it moves fast. Speed of traffic may be difficult to judge and rapid facial expressions may not be seen due to dyskinetopsia.
- Visual field defects are common in CVI, particularly lower field defects and hemianopia. One has to be careful to distinguish between a pure field defect and inattention as inattention has a more severe impact on functioning in daily life. Traffic, food, people and toys on one side may not be perceived and this may not be compensated for by head and eye turn due to inattention being body-related (and needing a body turn) rather than related to gaze-direction. A lower visual field defect may be associated with dorsal stream dysfunction and can also be associated with inattention. Patients are unaware of anything in that part of their visual field and frequently bump into low furniture, have difficulty going down stairs and walking on uneven ground.
- Dorsal stream dysfunction can lead to impaired visual guidance of movement. This may be expressed in difficulty with accurately reaching for objects or judging the height or depth of objects. This is distinct from stereopsis, which can be present even in the presence of profound optic ataxia. Thus, motoric depth and the perception of depth are different. Dorsal stream dysfunction can also cause an inability to pay attention to more than one issue at once (simultanagnosia). Some children may not be able to look and listen at the same time or they may find it challenging to copy information in a classroom setting. Some children cannot cope with too much visual information and struggle to function in busy, crowded places like shopping malls or social groups.
- Ventral stream dysfunction is rarely an isolated feature. It tends to accompany dorsal stream dysfunction. Affected children may have difficulties recognising faces (prosopagnosia), objects (object agnosia) or familiar places (topographical agnosia). Although it is not expected from an optometrist to have an in-depth knowledge about CVI, it is helpful to familiarise yourself with CVI in order to identify if a patient needs further investigation. This may be further facilitated if one is aware of particular risk factors for CVI.
Table 1 summarises some of the perception terms found in CVI.
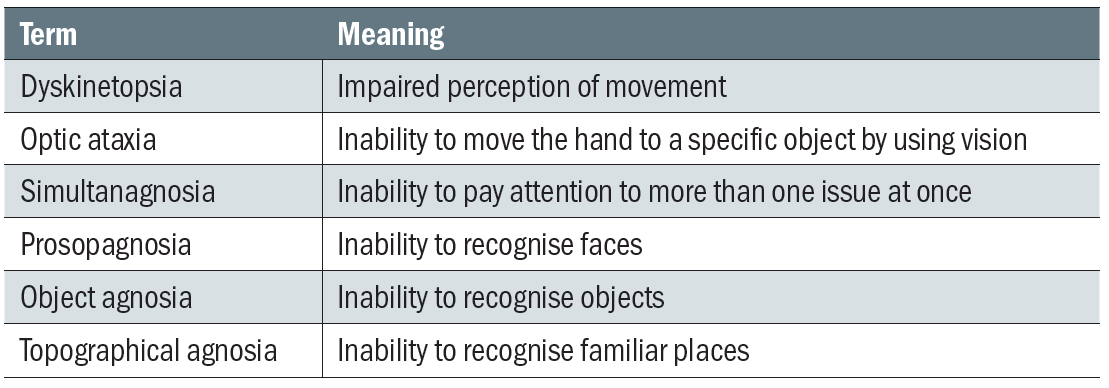
Table 1: Terminology of perceptual problems associated with CVI
Risk Factors for CVI
As eye care professionals, we are likely to encounter children and adults with CVI in community practice and it is therefore helpful to know which patients are particularly at risk. Knowing which patients are at risk will prompt the practitioner to investigate the possibility of CVI.
The first step in any consultation is history taking. Optometrists are familiar with the symptoms commonly explored in an eye examination, such as clarity of vision, presence of double vision, eye-strain, headaches, photophobia, and so on. In children, it is important to also include birth history and general health and development. This allows the practitioner to establish the presence of common aetiologies of CVI, including:
- Perinatal hypoxia
- Prematurity
- Hydrocephalus
- Structural nervous system abnormalities
- Seizures
Associated neurological findings include:13
- Seizures, cerebral palsy
- Periventricular leukomalacia
- Hemiparesis
- Impaired hearing
During the eye examination, refraction, binocular function and ocular health are assessed. One has to bear in mind that CVI is strongly associated with various ocular abnormalities. These include:
- Esotropia (19%)
- Exotropia (40%)
- Nystagmus (21%)
- Optic atrophy (42%)
- Significant refractive error of > +3.00DS or < -2.00DS (20%)
- Impaired accommodation
History and Symptoms
If the history, symptoms and ocular findings suggest an increased risk of CVI, the optometrist can ask some additional, specific questions to investigate the likelihood of CVI. Dutton et al recommend using five questions as a rapid clinical method of identifying children who warrant more detailed investigation.14 One has to be careful not to use this as a diagnostic tool, however, as CVI is a very complex condition that needs to be assessed by an ophthalmologist and/or paediatrician. The questions are listed in table 2.
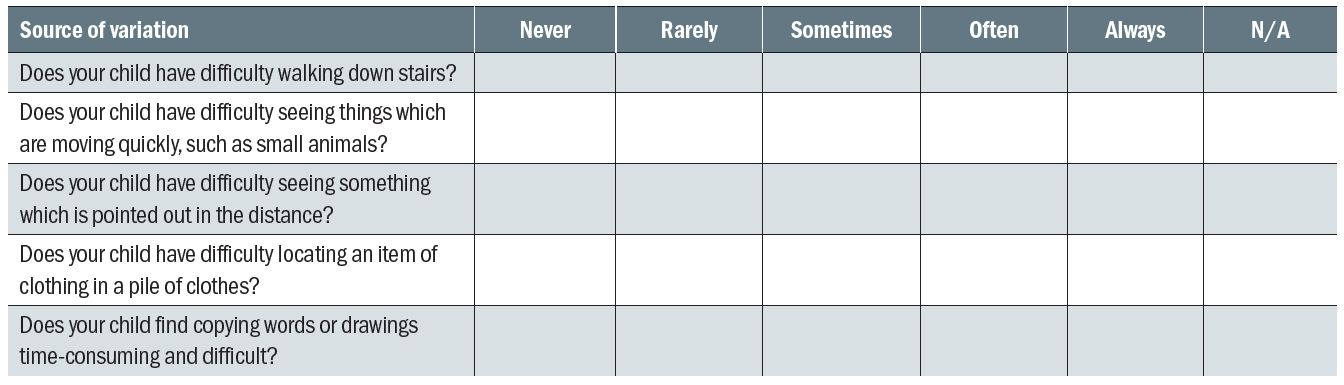
Table 2: Questions for use as rapid clinical method of identifying children who warrant more detailed evaluation. Modified from Dutton and Bax 14
Three or more positive responses (‘Often’, ‘Always’) suggest the possibility of CVI and those children would benefit from a referral. Optometrists are recommended to check the local referral pathways to ensure that the child is referred appropriately. Once a diagnosis of CVI has been confirmed, a more detailed question inventory can be used to obtain a more detailed picture of the patient’s altered visual world.
Dutton and Bax developed a question inventory with seven sets of questions, used to characterise the visual problems. It is used for children with a vision of 6/60 or better.14 The seven sets of questions are related to seven areas of visual difficulties, as outlined in table 3. As with the questions in table 2, the answers on the questions within each category are marked as ‘Never’, Rarely’, ‘Sometimes’, ‘Often’ or ‘Always’. The question inventory helps to gain an understanding of the ‘altered visual world’ of the child and an intervention plan can then be discussed. For example, if a child has a lower visual field defect with inattention, the child may benefit from having plain boundary-free floor coverings in the house to improve mobility around the house. It would also be helpful to remove low furniture such as coffee tables. For going down the stairs, holding on to a banister for tactile guidance improves confidence. Doing up buttons may be easier in a full-length mirror. In the school environment, the use of a book-stand ensures that the lower part of the page is seen. These and other possible interventions can all be explored with question inventories such as this. A detailed discussion about the use of question inventories and the possible interventions is outside the scope of this article.
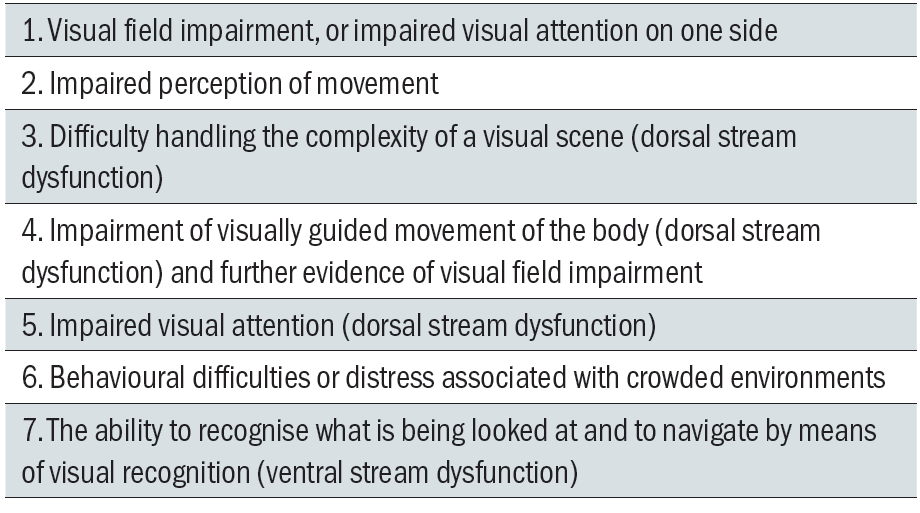
Table 3: Seven categories for the question sets. Modified from Dutton and Bax14
Conclusion
CVI is a condition that optometrists are likely to encounter. However, it is currently under-diagnosed, which means that those children are compromised in their learning. Being able to identify children who warrant further investigation can have a huge impact on their education and their well-being. In the UK the two main charities that provide education for professionals and patients are CVI Scotland and the CVI society. It is worth having a look at their websites for more information on this topic. They are:
- CVI Scotland website. Available at www.cviscotland.org
- CVI Society website. Available at cvisociety.org.uk
Useful information to understand how CVI is diagnosed by ophthalmologists/ paediatricians is available at:
- VINCYP (Visual Impairment Network for Children and Young People). Guide to Consistent Diagnosis of Cerebral Visual Impairment (CVI). www.vincyp.scot.nhs.uk/wp-content/uploads/2018/04/2018-CVI-Diagnostic-Guidance-v1.0.pdf
Cirta Tooth is a hospital optometrist based in Edinburgh with a special interest is low vision and functional vision.
Acknowledgement
Tree diagram was reproduced from: Lueck, Amanda H.; Dutton, Gordon N. (Eds.) (2015). Vision and the Brain: Understanding Cerebral Visual Impairment in Children. New York: AFB Press. (With permission from Dutton GN.)
References
- Mitry, Danny; Bunce, Catey; Wormald, Richard; et al. 2013b Childhood visual impairment in England: a rising trend. Archive of Diseases in Childhood 98(5).
- Kozeis, N. 2010. Brain visual impairment in childhood: Mini review. Hippokratia 14(4), pp. 249-251.
- Philip, S.S.; Dutton, Gordon N. 2014. Identifying and characterising cerebral visual impairment in children: a review. Clinical and Experimental Optometry 97(3), pp. 196-208.
- Solebo, Ameenat L.; Rahi, Jugnoo. 2014. Epidemiology, aetiology and management of visual im-pairment in children. Arch Dis Child 99, pp.375–379.
- UK National Screening Committee. 2013. The UK NSC recommendation on vision defects screening in children. Available at https://legacyscreening.phe.org.uk/vision-child [Accessed on 13 Jan 2019].
- Pehere, Niranjan; Chougule, Pratik; Dutton, Gordon N.; et al. 2018. Cerebral visual impairment in children: causes and associated ophthalmological problems. Indian Journal of Ophthalmology 66(2), pp. 812-815.
- Chandna, Arvind; Norcia, Anthony; Migas, Sylwia. 2017. Relative motion loss in high functioning children with cerebral visual impairment (CVI). Investigative Ophthalmology and Visual Science 58(8),Meeting abstract: 4896.
- Maitreya, Amit; Rawat, Darshika; Pandey, Shubham. 2018. A pilot study regarding basic knowledge of ‘cortical visual impairment in children’ among ophthalmologists. Indian Journal of Ophthalmology 66(2), pp. 279-284.
- Binder, Nicholas R.; Kruglyakova, Jacqueline; Borchert, Mark S. 2016. Strabismus in patients with cortical visual impairment: outcomes of surgery and observations of spontaneous resolution. Journal of American Association of pediatric Ophthalmology and Strabismus 20(2), pp. 121-125.
- Sakki, Hanna E.A.;Dale, Naomi J.; sargent, Jenefer; et al. 2018. Is there consensus in defining child-hood cerebral visual impairment? A systematic review of terminology and definitions. British Journal of Ophthalmology 102(4), pp. 424-432.
- Lueck, Amanda H.; Dutton, Gordon N. (Eds.) (2015). Vision and the Brain: Understanding Cerebral Visual Impairment in Children. New York: AFB Press. Page 34.
- Zihl, Joseph; Dutton, Gordon N. 2015. Cerebral visual impairment in children. Pages 147-155. Wien: Springer-Verlag.
- Kheptal, Vijay; Donahue, Sean P. and Donahue, S.P. 2007. Cortical Visual Impairment: Etiology, as-sociated findings, and prognosis in a tertiary care setting. Journal of American Association of pediatric Ophthalmology and Strabismus 11(3), pp. 235-239.
- Dutton, Gordon N.; Calvert, Julie; Ibrahim, Hussein; et al. 2010b. Impairment of cognitive vision: its detection and measurement. In: Book Dutton, Gordon N. and Bax, Martin. 2010. Visual Impairment in Children due to Damage to the Brain. MacKeith Press, London, pp. 117-128.
