Obesity is an escalating global problem of epidemic proportions and a major risk factor for several chronic systemic diseases. Those known to have a strong association with obesity include:
- Hypercholesterolaemia
- High blood pressure
- Cardiovascular diseases (CVD) – such as arteriosclerosis, atherosclerosis, occlusive disorders and disorders of the heart
- Stroke (cerebrovascular accident or CVA)
- Obstructive sleep apnoea (OSA)
- Malignant disease – a number of malignant disorders have association with obesity
- Osteoarthritis
- Diabetes mellitus (DM) – the increase in incidence of type 2 diabetes has reflected in the increase in obesity
Changes in the recent socioeconomic environment, lifestyle, and food consumption, as well as an increase in urbanisation have contributed to the rise in obesity.
Definition of Obesity
According to the World Health Organisation (WHO), obesity is defined as an accumulation of excessive or abnormal fat that is associated with an increased risk of medical illness. Body mass index (BMI) is a commonly used indicator of body fat, calculated by dividing a person’s weight in kilograms, by the square of their height in metres (kg/m2), giving a weight to height ratio. WHO classify any BMI value ≥25 as overweight, and any BMI value ≥30 as obese (see table 1).
Waist-to-hip ratio (WHR) is a relatively new anthropometric index that is normalized by body size and represents a better predictor of disease or mortality risk than BMI.
The aetiology of obesity is based upon the energy imbalance between caloric intake and caloric expenditure. To maintain a healthy body weight, the amount of calories entering the body should equal the amount of calories leaving the body. Obesity is a result of an accumulation of calories leading to a build up of fat (as different forms of adipose tissue).
It was initially thought that adipose tissue was merely a fat storage mechanism, only playing a passive role in the development of obesity. However, it has been discovered that this metabolically active hormone-secreting tissue maintains the regulation of metabolism, energy intake and fat storage.1 An increase in body fat causes the adipose tissue to become dysfunctional and disturbs the secretion of hormones, thus causing it to become inflamed, hypoxic and scarred, rendering it unable to store surplus nutritional fat. Such conditions predispose the body to several metabolic disturbances such as insulin resistance2 and atherosclerosis.3
As the first health assessment for many patients may be their routine eye examination, optometrists are at the front line of detecting an array of undiagnosed systemic and ocular diseases that are a result of obesity.
Why Do We Put On Weight?17
- The Palaeolithic diet was sporadic and not assured as it depended on finding dispersed food in order to eat it, and success in this was not guaranteed. Because of this, if food was available, we developed the instinct to eat and, if possible, store the energy in our bodies to be used up the next time that availability was restricted. We still have this instinct but, in modern society, the ready availability of food means that if we indulge it we can overeat.
- Cooking food releases more nutrients for digestion than if it is eaten raw. The cell walls of both meat and vegetables are broken down, releasing the nutrients to our digestive systems. Processing foods, for instance by grinding grains into flour, also releases the nutrients, and greatly increases the surface area of the food accessible to digestive enzymes. It is suggested that the time saved from foraging by these more concentrated forms of food has freed up time for us to develop our intellects and more complex societies.
- The human microbiome is a population of some one to two kilograms of symbiotic bacteria in the gut, and we are coming to realise that this has a much more important part to play in both digestion and health than was previously known. The bacteria break down many foods indigestible to us into forms that we can more readily absorb, and the profile and nature of this population therefore plays a considerable part in our use of the food that we eat.
- The simplified approach to reducing weight is to eat fewer calories than are burnt in a normal day of activity. As with anything biological, this is an over-simplification and subject to the influence of several other factors. Our calorific need goes up with body weight, as we have to support the additional weight that we put on. Consumption of fewer calories leads to loss of weight until our body mass adjusts to the new intake and then weight loss will stop. To continue to reduce weight, we need to reduce our intake to a level supporting an even lower mass.
- With a reduced intake, the first step is to burn up sugars stored in the liver, and as these are dissolved in water, their use means that the water is no longer needed. It is therefore excreted, leading to fairly rapid initial weight loss that slows when all the water is excreted – the body then switches to burning fat and subsequent weight loss will tend to be slower. A slow rate of loss is not to be underestimated – a kilogram does not sound like much when looking at the scales, but if you consider the size of a kilogram block of butter or lard, it is considerable, and its loss should be appreciated.
- An inactive lifestyle is one of the greatest risk factors for obesity. Exercise builds muscle which, whether it is working or not, burns more calories than fat. However, muscle is also denser than fat, and so weighs more, possibly making fat-loss look less than it actually is when using scales.
Ocular diseases associated with obesity
While the effect of obesity on the body is well documented, there is less talk on the implications of obesity on ocular health. Let us consider some ocular conditions with association with obesity. We will first consider those affecting anterior eye structures, then posterior structures and finally those affecting the structures of the eye indirectly.
Anterior eye complications
Floppy eyelid syndrome (FES)
FES is characterised by hyperelasticity of the upper eyelids. Many of FES patients are obese and it is believed that nearly 100% of them suffer from obstructive sleep apnoea. In FES, the upper eyelid can evert easily, especially when the patient sleeps on one side. During this position, the eyelid turns and exposes the palpebral conjunctiva to the pillow. The patients will usually present with recurrent unilateral red eye that does not respond to any of the conventional treatments. They are often erroneously diagnosed with either infectious conjunctivitis, blepharitis or dry eye and receive various treatments that do not solve the condition. FES is also associated with the following changes:
- Ptosis
- Keratoconus
- Superficial punctate keratopathy
- Lower lid ectropion
- Keratinization of the conjunctival surface of the affected upper eyelid
- Secondary dry eye
- Blepharitis (due to inflammation and abnormalities of the tarsal and accessory lacrimal gland – see figure 1)
- Lash misdirection.
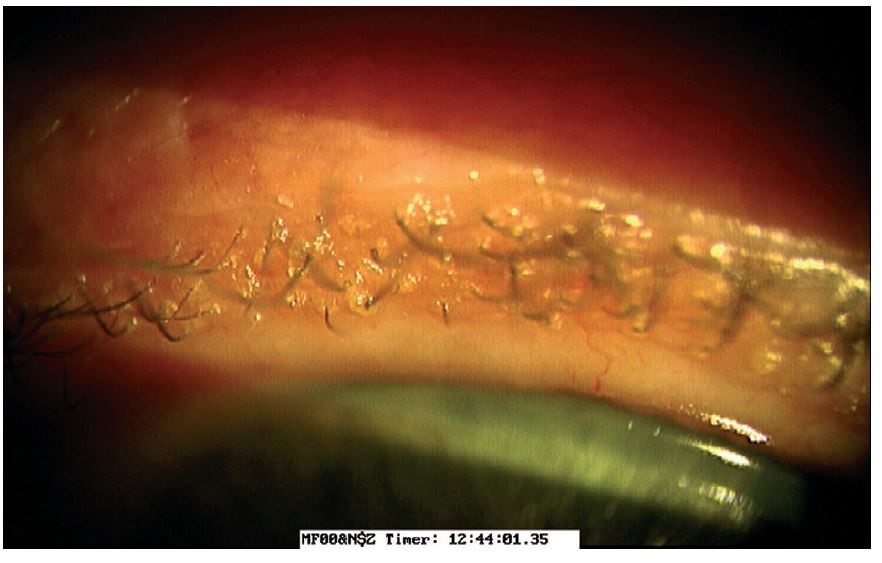
Figure 1: Blepharitis may be present in floppy eyelid syndrome
When diagnosed, FES patients also need to be referred for sleep studies as well as for surgical correction of their condition. Other management measures can include lid taping/patching, tear sub- stitutes and steroids for the ocular inflammation.
Dry eye disease (DED)
DED is defined as ‘a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play aetiological roles.’4
It has been shown that diabetes doubles the risk of asymptomatic meibomian gland dysfunction (MGD), contributing to symptoms of DES.5 The effect of diet has also been correlated to the maintenance of a healthy and functional tear film. Indeed, 500,000 new cases of malnutrition-induced xerophthalmia have been found to occur in various regions of Asia each year,6 illustrating the influence of nutrition on tear film quality.
Besides a confirmed, specific diagnosis and management of the DES, optometrists could offer suggestions in improving diet and intake of nutritional supplements, primarily vitamin A, which can all improve the quality of the tear film and the health of the ocular surface.
Cataract
Although the association between cortical and posterior subcapsular cataract and obesity is documented, the exact causal relationship is not fully understood, although a high oxidative stress and increased inflammation are regarded as the most likely candidates. In addition, obesity and cataract have other factors in common, such as diabetes, hyperlipidaemia and hypertension. Many epidemiological studies, including Barbados Eye Study, Blue Mountain Eye study and Age-Related Eye Disease Study (AREDS), found an association between waist-to-hip ratio (WHR) and cortical cataract. The Nurses’ Health and the Health Professionals Follow-up Study reported that obesity increases risk of posterior subcapsular cataract (figure 2) even after adjusting for variables such as smoking, age and diabetes.7 However, there is no clear evidence to show that weight loss prevents cataract formation.
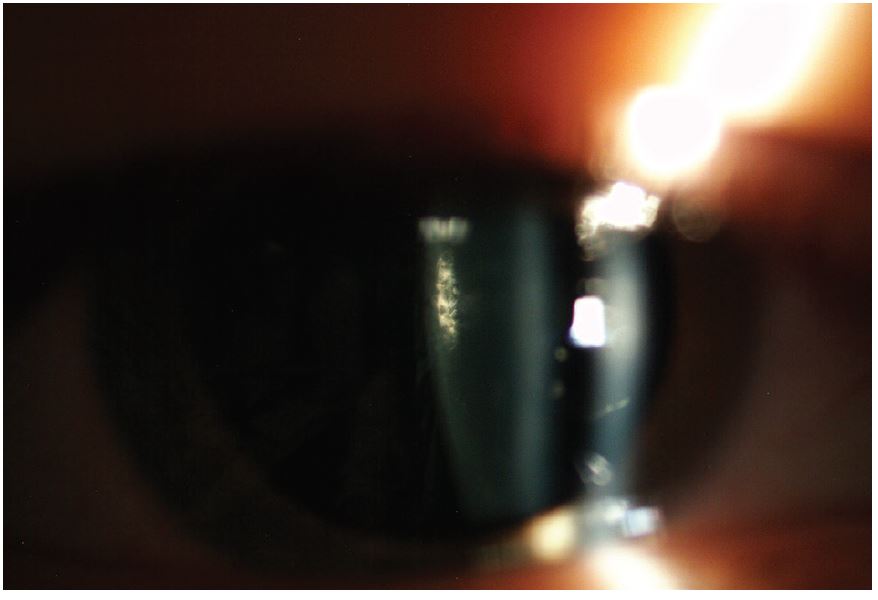
Figure 2: Posterior subcapsular cataract
Posterior complications
Hypertensive Retinopathy
Systemic arterial hypertension is often associated with obesity and represents the main cause of stroke and a major risk factor for heart disease, such as heart attack and heart failure. It can also induce severe kidney disease and ultimately, kidney failure. Approximately one-third of people with systemic hypertension are still undiagnosed and the disease is responsible for more than 62,000 preventable deaths through stroke and heart disease each year (data from Blood Pressure UK).
At the ocular level, the first signs of high blood pressure (BP) are represented by retinal arteriolar narrowing (figure 3).
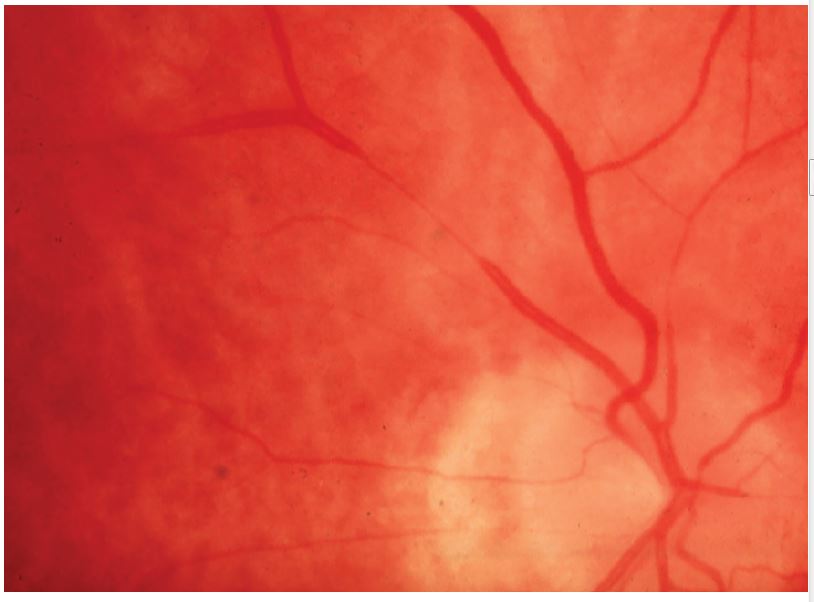
Figure 3: Arteriolar narrowing
Focal retinal arteriolar narrowing and arteriovenous nipping are structural vascular signs that reflect high BP (figure 4). In addition, wider retinal veins are commonly associated with an increased risk for stroke.
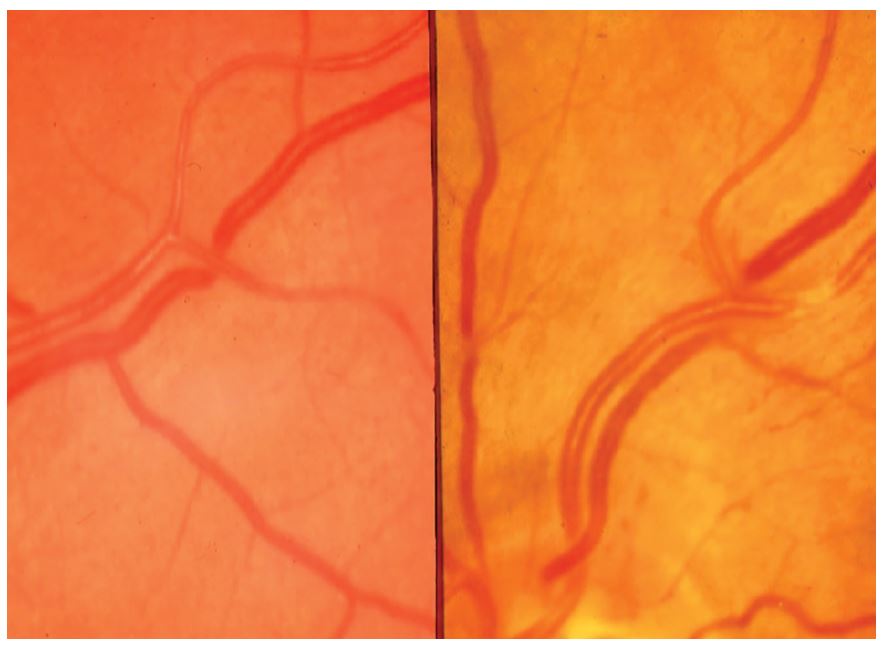
Figure 4: Arteriovenous nipping
Other retinal vascular changes associated with hypertension include:
- arteriovenous nipping
- generalised retinal arteriolar narrowing
- cotton wool spots
- microaneurysms
- flame and blot-shaped retinal haemorrhages
- exudative maculopathy
- disc oedema.
In addition to detecting and monitoring the above fundoscopic changes, optometrists can also play a role in BP monitoring. It is often the case that our patients have a well-controlled systemic hypertension through their treatment. However, in other situations the patients are either non-compliant with their treatment regime or the medication is inefficient. Therefore, on the spot checking of BP by the optometrist can often detect abnormal values in individuals with fundoscopic changes that suggest systemic hypertension (figure 5). Nevertheless, despite the fact that measuring systemic BP does not require specialist training, only a small proportion of optometrists use BP monitors in their practice. There is, therefore, a high need to increase awareness among optometrists and possibly offer them specialist training for measurement and interpretation of BP values.
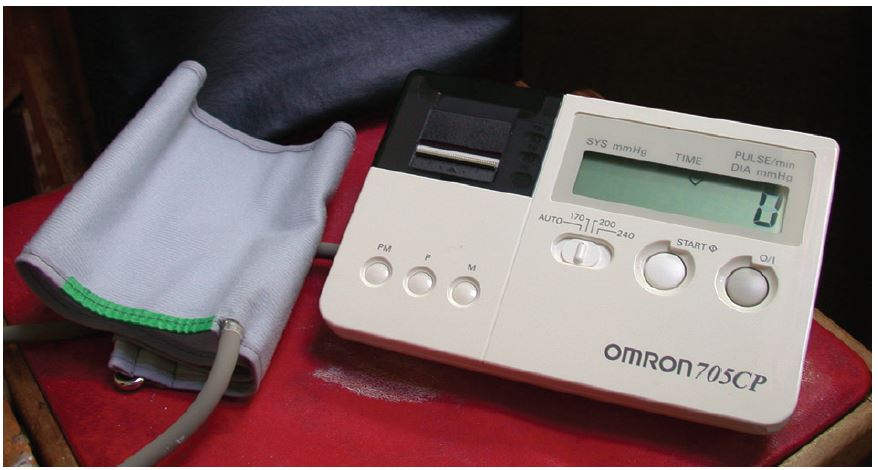
Figure 5: Modern electronic blood pressure measuring devices are reliable and easy to use
Diabetic retinopathy (DR)
Most of the available studies suggest that a high BMI is associated with an increased risk of DR. In addition, there are new data that show obesity is associated with retinopathy signs in the general population and non-diabetic persons,8 including:
- retinal haemorrhages
- microaneurysms
- hard exudates
- cotton-wool spots (figure 6)

The suggested links between obesity and DR are via hyperlipidaemia, hypertension, oxidative stress, blood viscosity and serum angiogenic factors, including VEGF.
The association between hypertensive retinopathy and DR is well documented and, in patients with diabetes, the presence of retinopathy is not only related to hyperglycaemia and duration of diabetes but to the presence of other cardiovascular risk factors as well, including high blood pressure and hyperglycaemia. It has been shown that treating high blood pressure in patients with DM prevented or delayed progression of retinopathy9. Therefore, it has been proposed that in diabetic patients, retinopathy is a multifactorial microvascular complication dependent on a large variety of factors, including blood pressure, BMI and lipid concentration.10
Although the impact of weight loss in obese individuals, on prevention and regression of retinopathy has been inadequately investigated, it is generally accepted that weight reduction should be advised in obese diabetic individuals to reduce the risk of cardiovascular disease and, possibly, of DR.
Age-related macular degeneration (AMD)
The first study to report a relationship between obesity and AMD (figure 7) was published in 199611 The AREDS also reported associations between higher BMI and more advanced AMD.12 Later, other studies, such as Blue Mountains Eye Study, Beaver Dam Eye Study and The Pathologies Oculaires Liées à l’Age (POLA), also found various association between BMI and various stages of AMD. Central obesity, as defined by the waist circumference or WHR, has also been found to increase risk of progression to advanced AMD.13
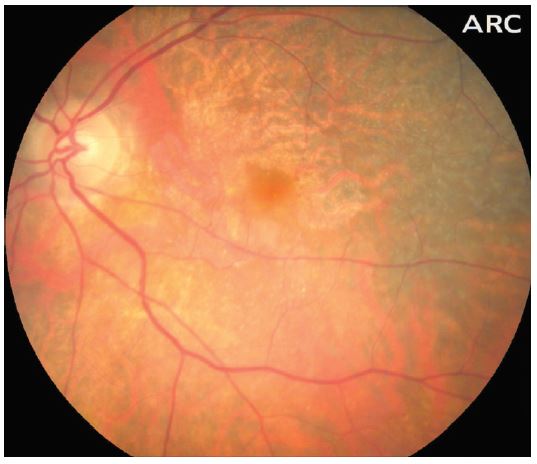
Figure 7: Age-related macular degeneration
As with other association between obesity and ocular diseases, the role of weight loss in AMD prevention is not sufficiently researched and proven.
Glaucoma
It has been previously stated that there is a link between primary open-angle glaucoma (POAG) or elevated intraocular pressure (IOP) and general adiposity (figure 8). Nevertheless, the available research is contradictory. In a recent meta-analysis study, Liu et al14 have looked at 15 studies involving more than 2.4 million individuals.
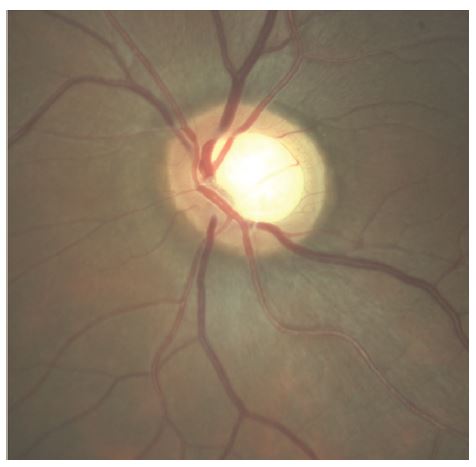
Figure 8: Primary open angle glaucoma
The main conclusion from their study was that there is evidence showing that adiposity is associated with high IOP and abdominal adiposity is linked to the occurrence of POAG, especially in female patients. Proposed risk factors responsible for the association between adiposity and high IOP/POAG include higher trans-lamina cribrosa pressure difference (TLCPD) in obese individuals, excess orbital fat tissue that results in an increase episcleral venous pressure and blood viscosity, oestrogen levels and high oxidative stress.
To date, no research has looked at the effect of weight loss on glaucoma progression in obese individuals.
Other ocular diseases associated with obesity
Pseudotumor cerebri or idiopathic intracranial hypertension
This represents a vision-threatening disorder that predominantly affects obese women of childbearing age. Its incidence is 12 to 20 per 100,000 people per year. However, younger patients are also affected, more so because of the increasing number of obese individuals among children and adolescents. The clinical presen-tation of pseudotumor cerebri can be variable but common symptoms include headaches, neck pain, vision loss, pulsatile tinnitus, transient visual obscurations, and binocular horizontal diplopia. It may be seen as papilloedema on ophthalmoscopy (figure 9).

Figure 9: Papilloedema
Exophthalmos.
Bilateral exophthalmos is observed in a large number of obese individuals, and it is important that these cases are differentiated from Graves’ disease.15
The role of optometrist
Obesity is associated with a wide range of ocular disorders, and table 2 summarises some key points.
It is unequivocal that obesity has perilous effects on the body, including the eye.
Beside ocular diagnosis and management, optometrists can also get involved in obesity management by first opening the subject with their patients. Providing the patients with the leaflet ‘Lifestyle and Eyes’ available from the College of Optometrists could be a good starting point for a more open discussion that could otherwise be more difficult.
Offering evidence about the link between their presenting ocular pathology and obesity, could offer the patients an unprecedented insight into their situation as well as increase their motivation to adopt a better lifestyle. Moreover, optometrists should also collaborate with the other healthcare practitioners involved in the care of obese patients, in order to maximise the positive results.
Dr Doina Gherghel is a lecturer in ophthalmology at the School of Life and Health Sciences, Aston University and Nisha Ramchandani is an optometrist practising in London.
References
- Greenberg AS, Obin MS. Obesity and the role of adipose tissue in inflammation and metabolism. The American Journal of Clinical Nutrition. 2006;83(2):461S-5S.
- Hotta K, Funahashi T, Bodkin NL, Ortmeyer HK, Arita Y, Hansen BC, et al. Circulating concentrations of the adipocyte protein adiponectin are decreased in parallel with reduced insulin sensitivity during the progression to type 2 diabetes in rhesus monkeys. Diabetes. 2001;50(5):1126-33.
- Hotta K, Funahashi T, Arita Y, Takahashi M, Matsuda M, Okamoto Y, et al. Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Arteriosclerosis, thrombosis, and vascular biology. 2000;20(6):1595-9.
- TFOS DEWSII. Available at http://dx.doi.org/10.1016/j.jtos.2017.05.001
- Viso E, Rodriguez-Ares MT, Abelenda D, Oubina B, Gude F. Prevalence of asymptomatic and symptomatic meibomian gland dysfunction in the general population of Spain. Investigative ophthalmology & visual science. 2012;53(6):2601-6.
- Sommer A, Tarwotjo I, Hussaini G, Susanto D, Soegiharto T. Incidence, prevalence, and scale of blinding malnutrition. Lancet (London, England). 1981;1(8235):1407-8.
- Weintraub JM, Willett WC, Rosner B, Colditz GA, Seddon JM, Hankinson SE. A prospective study of the relationship between body mass index and cataract extraction among US women and men. Int J Obes Relat Metab Disord. 2002 Dec; 26(12):1588-95
- van Leiden HA, Dekker JM, Moll AC, et al. Risk factors for incident retinopathy in a diabetic and nondiabetic population: the Hoorn study. Arch Ophthalmol. 2003;121:245–51
- UK Prospective Diabetes Study Group: Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 317:703–713, 1998
- http://care.diabetesjournals.org/content/25/8/1320
- Hirvelä H, Luukinen H, Läärä E, Sc L, Laatikainen L. Risk factors of age-related maculopathy in a population 70 years of age or older. Ophthalmology. 1996 Jun; 103(6):871-7.
- Age-Related Eye Disease Study Research Group. Risk factors associated with age-related macular degeneration. A case-control study in the age-related eye disease study: Age-Related Eye Disease Study Report Number 3. Ophthalmology. 2000 Dec; 107(12):2224-32.
- Seddon JM, Cote J, Davis N, Rosner B. Progression of age-related macular degeneration: association with body mass index, waist circumference, and waist-hip ratio. Arch Ophthalmol. 2003 Jun; 121(6):785-92.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5485359/
- https://www.ncbi.nlm.nih.gov/pubmed/15017102)
- Cheung N, Wong T. Obesity and Eye Diseases. Surveys in Ophthalmology, 2007; 52(2): 180–195.
- Grant R. Obesity and the eye. Optician, 19.06.15, 12-15.
