Success with contact lenses begins with finding the best match for each individual patient and ensuring that we review that match regularly as patients’ lifestyles and ocular health needs change. Contact lens retention research indicates that 26% of new wearers cease lens wear within the first year, with nearly half of those dropping out in the first two months.1-3 It is evident that a deep understanding of the patient’s needs alongside meaningful clinical evaluations, are key to success. Significant advancements in technology now mean we have a large range of materials, modalities and designs available to best match up with each individual’s specific requirements. Beyond the initial investigation and fitting, viewing each encounter as an opportunity to update this information ensures that the patient has every chance of remaining a successful contact lens wearer.
Patient discussion ‘History and symptoms’
The initial conversations within a contact lens assessment are key to gaining a comprehensive evaluation of the patient. Determining any contraindications to contact lens wear alongside the initial clinical assessment will provide you with the information needed to help recommend the most appropriate lens for the patient. If we can select the best lens the first time, it helps not only to reduce the need to trial alternatives, and hence use more chair time, but also serves to reduce drop out in those first few months or thereafter.
A comprehensive evaluation should include discussion around:
- Motivation
- Occupation
- Lifestyle
- Ocular history
- General health
In addition to providing you with an understanding of the patient’s vision requirements and expectations, this initial conversation is key to build rapport with your patient. Not only does this make them feel more comfortable but it helps you determine the personality style of your patient and adapt yourself accordingly. For example, the anxious patient may need more reassurance, whereas someone who likes to just get things done may only want the key points highlighting and less in-depth discussion. As per the General Optical Council (GOC) Standards of Practice, we need to treat our patients as individuals and take into account their views, preferences and concerns. Remember patients need to be involved in decisions about their care so by giving them options and recommendations specific to their own requirements, you are very much involving them in the lens selection process.4
Remember, effective communication relies on responsive listening and appropriate body language from you as a practitioner (figure 1). You need to look interested in what they are saying and maintain eye contact wherever possible. It is critical that you make note of any information gathered from the history taking in order to manage the patient effectively throughout their contact lens journey. It is worth considering what your body language is saying, for example, facing away from a patient to record notes, especially with computer-based systems, may change the dynamic of the interaction. Accurate notes are essential, but building a rapport is equally as important.

Figure 1: Body language is an important part of effective communication
Before you start – what do you need?
Before you begin a fit for contact lenses, the patient must have had a valid spectacle prescription – most commonly this is dated within the last two years, but it may need to be more recent if a different recall is specified on their prescription. If the patient has not been to your practice previously, they need to bring a copy of their results to the fitting appointment.5 For those wanting zero powered (cosmetic) contact lenses they should have had a recent sight test.
Within this chapter we will consider each aspect of the history taking in turn, highlighting the key things you want to be able to learn about your patient, and more importantly, why (table 1). A history is commonly taken in a pre-defined order and can be a remarkably similar list of questions from one patient to the next. Understanding why each question should be asked, and beyond that, when and how to explore an answer further, provides the practitioner with the additional understanding needed to make any recommendations truly specific to that individual
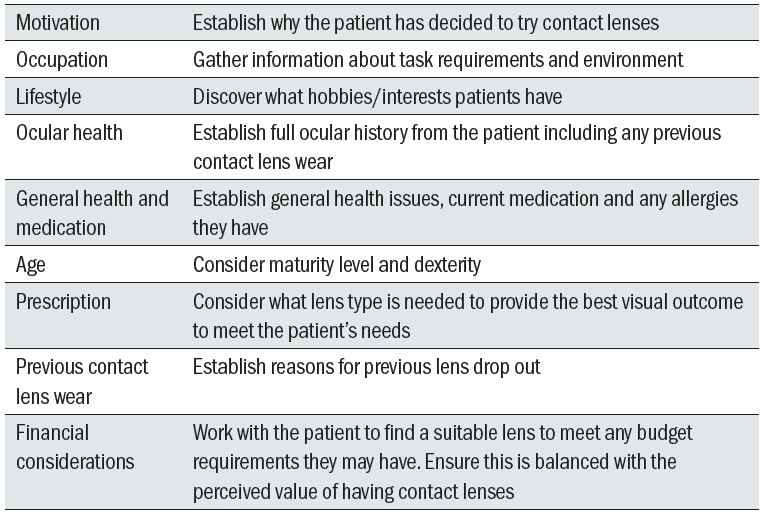
Table 1: Aspects of a thorough history and symptoms
Motivation
When a patient arrives for a contact lens fitting, they have already made the decision that they want to try contact lenses. However, it is still essential to establish why someone has decided to try contact lenses. Is it due to practical reasons such as frustration with reading glasses, to help with sports as spectacles aren’t a practical solution, or is the decision a deeper, more emotional based reason, such as confidence and self-esteem? Finding the true motivation is easier with some patients than others which is why building rapport is key. Open questions like ‘what has prompted you to come in to discuss the option of contact lenses with me today?’ or ‘how do you see contact lenses fitting in to your lifestyle?’ may provide insight. It is important to remember that patients may be less forthcoming with emotional reasons and may provide a practical explanation as an alternative. Non-verbal clues may also provide insight, for example a patient with a significant prescription coming in without their glasses on. Understanding their motivation will help you establish what type of wearing schedule they will want and in turn consider what material properties will be needed. It is important to be mindful when asking questions about potential wearing schedules at this stage, especially if you are using this information in your decision making process. Your patient is new to contact lenses, and while initially may think they only want them for a specific task, may later decide that they want to wear them far more often.
Occupation
Finding out what the patient does for work is critical in order to know what they will be doing when wearing their contact lenses and the specific requirements they will have. A simple job title however, does not always suffice. Again, open questions such as ‘what does a typical day at work look like?’ gathers far more useful information than a job title.
The following are key things to discover:
- Screen use?
If so, what type. Is it a desktop, laptop or even a tablet or phone, as this will affect working distance considerations; something which is particularly important for presbyopic patients. The number of hours spent on these devices is also useful to note as screen use is known to reduce blink rate,6 which may lead to corneal desiccation (figure 2) and ultimately affect the comfort of the lenses, especially if coupled with an air-conditioned environment. Knowledge of screen work requirements can help when considering an appropriate lens material. If they want lenses for work which involves a lot of screen use, lenses with improved wettability and low co-efficient of friction will need to be considered.
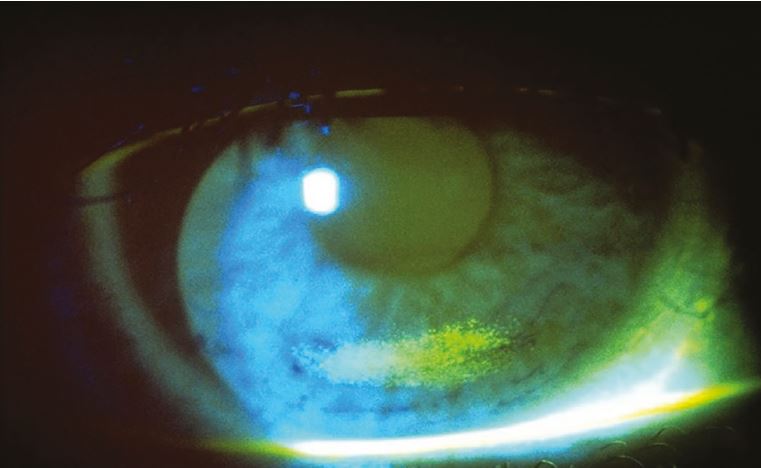
Figure 2: Corneal desiccation staining secondary to incomplete blinking
- Driver?
Blink rate can also reduce when driving and differing environments within the car such as heating or air-conditioning could affect lens comfort. When driving, patients will regularly change gaze directions, meaning rotational stability is a key consideration for toric wearers.
- Environment?
It is important to consider if the environment is suitable for contact lens wear. Dusty environments may present a contraindication to contact lens wear as will environments where toxic fumes are present.
Depending on the work environments contact lenses may not be suitable for work purposes but could still be an option for outside of work. For example, pilots are only allowed to wear distance-only contact lenses. Monovision and multifocal options are not permitted so it may be that a presbyopic pilot requires different contact lenses for work than for social purposes.7 Dual wear of glasses and contact lens wear is a key opportunity and understanding what type of visual correction suits when, will enable your patient to have the best set up for them. Honest conversations about realistic expectations of what lenses can and cannot do is key at this stage.
Lifestyle
In addition to any occupational information, it is useful to know what hobbies or interests people have, particularly if contact lenses are to be used for specific activities. The best way to start this discussion is with an open question such as, ‘what do you like to do in your spare time?’ or ‘do you have any particular hobbies or interests?’ Further questions will then often be required to provide further clarification. For example, if the answer is ‘sports or exercise’ further details are needed to establish the type of sport or activity to ensure appropriate advice is given. Soft contact lenses, as opposed to RGPs, are more advisable for sports in general, particularly for contact sports, due to safety implications.
Swimming is always an important thing to discuss with potential contact lens wearers because of the increased risk of serious infections such as microbial keratitis and acanthamoeba keratitis due to accumulation of microbial organisms on or in the contact lens.8 If a patient wants contact lenses for swimming, then a frank and open discussion around the increased risk must be had. General advice is that contact lenses should not be worn for swimming or participating in water sports without wearing tight-fitting goggles over the top. Research has shown fewer bacterial colonies were found on goggled contact lenses, therefore if a patient wants them for swimming we should encourage them to wear tight fitting goggles. This, in conjunction with a daily disposable option which can be removed and discarded immediately after swimming – or indeed any other activity where there will be contact with water – will minimise the risk.9
If the lenses are to be worn outdoors for significant periods of time, then UV protection is worth discussing with your patients as they can provide protection to the cornea, lens and retina. Many patients are unaware that contact lenses can also provide this health benefit. It is important that wraparound sunglasses and wide-brimmed headgear are still recommended in addition for activities which involve high concentrations of UV light, such as skiing or sailing, in order to fully protect the eye and surrounding tissue.
Ocular history
A full and detailed ocular history is invaluable for successful contact lens fitting.
In general, it is good to establish if patients have had any previous infections, surgery, trips to hospital for their eyes or any ocular conditions that have previously been mentioned or they are currently receiving treatment for. Perhaps most importantly, it must be established if they have worn contact lenses previously. A detailed history into previous lens wear and specifically, why they ceased lens wear, can provide valuable and necessary insight.
Contraindications to contact lens wear would include any acute or sub-acute inflammation of the anterior segment, or acute or chronic eye infection.10 Certain ocular conditions may be a contraindication to contact lens wear or may mean you decide to still fit the patient but do so with caution and may need to limit wear times accordingly. Ocular conditions that may be relevant include corneal dystrophies and patients with pterygium or pinguecula. Patients with dry eye or blepharitis will necessitate additional advice or investigations prior to fitting, while patients with a history of previous microbial keratitis may affect your advice on contact lens replacement frequency. Ocular conditions requiring frequent drop use such as glaucoma, or even the regular use of anti-histamine eye drops will require specific recommendations. It is worth noting that fitting contact lenses in the presence of active pathology should not be undertaken without the prior approval of the treating ophthalmologist.
Dry eye is worth a specific mention here as discomfort is often a key reason for patients dropping out of contact lens wear. Table 2 summarises some of the risk factors which were categorised as consistent, probable and inconclusive in terms of risk of developing dry eye disease from the Dry Eye Workshop (DEWS) II report.10 If a patient has any of these risk factors, discussion about dry eye symptoms is useful at this stage. Key words to listen out for include ‘gritty’, ‘burning’, ‘watery’ or ‘stingy’, all of which would indicate a potential eye dryness issue. The use of a specific dry eye questionnaire such as Dry Eye Questionnaire-5 (DEQ-5) or the Ocular Surface Disease Index (OSDI) can be used to indicate if the patient suffers from dry eye disease.11 This topic will be discussed in more detail in a later chapter of this series.
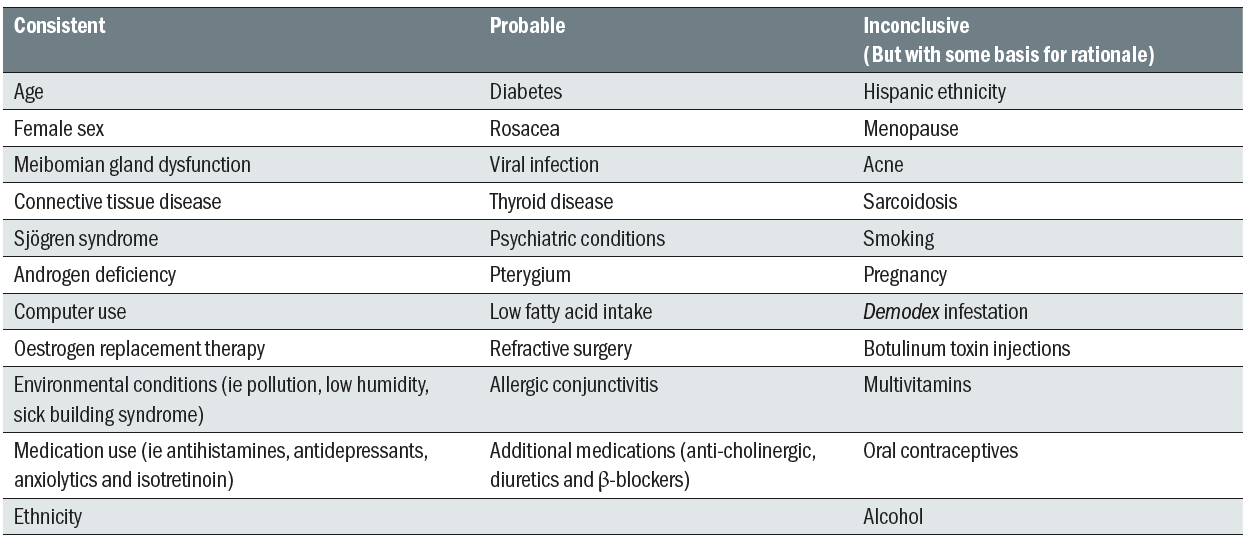
Table 2: Risk factors for dry eye (Table generated using information from the DEWs II Executive Summary 11)
General health
This is another area where specific lists of questions are routinely asked. It is important to consider how you ask a question, and whether it adds any value to your consultation. Open questions are needed initially but take care in the way they are asked. If you ask a well-controlled, diet managed diabetic ‘how is your general health?’ they would probably reply by saying ‘fine’ as they are well controlled. Many practitioners will follow up this type of question by asking if they take any medication. In this instance – the patient would truthfully answer ‘no’ and you may completely miss the fact they are diabetic. Instead, try ‘tell me about your general health’ or ‘tell me about any general health issues currently being managed by your GP or other healthcare professional’. You may then need to use closed questioning to ask about medication, allergies or certain conditions you feel may be relevant.
Gaining an impression of the patient’s general health is important as certain general health issues may affect suitability for wearing contact lenses or affect the type of lenses that should be worn.
- Diabetes
It is estimated that the cornea is adversely affected in up to 70% of all patients with diabetes.12 Clinical manifestations are variable and may include corneal epithelial issues such as slow and incomplete wound healing and neuropathy meaning loss of corneal sensitivity.13 Patients with diabetes are also at increased risk of microbial keratitis,12 so daily disposable lenses may be indicated. Further questioning around duration of diabetes, level of glycaemic control and presence of retinopathy may be important considerations.
- Arthritis
These patients may suffer with associated dry eye issues, but also the arthritis may affect their manual dexterity. This may affect their ability to handle contact lenses and as such a lens with a higher modulus may be of benefit here.
- Skin conditions such as eczema
These patients may be vulnerable to excessive deposits, lid irritations, punctate keratitis and blepharitis and therefore careful consideration of lens material and modality is necessary.
- Thyroid dysfunction
Patients with thyroid dysfunction can suffer with associated thyroid eye disease (TED). The major concern here is exposure keratitis, however only 5-10% of patients have orbitopathy.14 Dry eye is the most common cause of ocular discomfort in these patients so questioning around this is key to see if they are symptomatic. Research has shown incomplete blinking and meibomian gland structural loss of the upper eyelid are more prominent in patients with TED than those with dry eye so this again highlights the need for a comprehensive anterior eye assessment.14
- Mental health conditions
It is also important to note any history of mental health issues, as patient’s taking antipsychotic medications may be more
vulnerable to dry eye issues (see table 2). The College of Optometrists guidance states: ‘You must not fit a patient with contact lenses if they are not able to use them safely’, so this should always be considered during the initial consultation.5
- Allergies
Approximately 25 per cent of the population suffer from allergies at some point in their life time.15 It is important to establish an atopic history for the patient as this may influence which type of lens you prescribe. Atopic patients are more likely to have papillae present under their lids initially, or could be more vulnerable to contact lens induced papillary conjunctivitis. Patients prone to allergy may also be more susceptible to contact lens solution reactions or be adversely affected by deposits that form on a contact lens surface. Daily disposable lenses have been shown to be an effective strategy for managing allergy suffering contact lens wearers.14
A significant number of commonly prescribed medications list dry eye as a potential side effect (table 2). While not every patient taking this medication will experience this side effect, it is important to consider as this may influence contact lens comfort. An accurate record of current medication is therefore crucial in all patient assessments.
When assessing patients for suitability for contact lens wear asking them if they smoke is very important as research suggests smoking is associated with a 3.7x increased risk of moderate and severe microbial keratitis.16 When eye care practitioners were asked what standard questions they ask on initial fitting only 59% asked if the patient smokes.17 This is something that we may need to get more comfortable asking our patients about, especially as our role as professionals extends into preventative health care.
Other considerations
Age of patient
- Children
Often parents will ask ‘how old do children need to be to wear contact lenses?’ A survey conducted by the College of Optometrists highlighted that the maturity of the child is of much greater importance than the age when deciding on suitability.18 A practitioner must also be able to satisfy themselves that a patient will be able to use them safely.5 The decision to wear contact lenses should come from the child, and not just a parent. Directing conversation and questions around contact lens wear to the child specifically, rather than the adult can, in some cases, provide invaluable insight into who actually wants them to wear contact lenses.
- Presbyopes
It is important to be aware of the natural changes to the eye that occur with age (table 3), as well as potential changes in manual dexterity, all of which may affect the potential success of the contact lenses. It is important to know and understand the patient’s specific visual needs, alongside discussing the different correction options. Newer generation multifocal lenses provide functional distance, intermediate and near vision, while maintaining the patient’s binocular vision and stereo acuity. It is important to set realistic expectations during this discussion stage, before you move onto the fitting section. Over-promising and under-delivering is a recipe for failure, whereas time spent managing and setting realistic expectations will help drive success. We are fortunate to now have a range of options to suit the presbyopic patient, so presbyopia should no longer be a barrier to successful contact lens fitting.
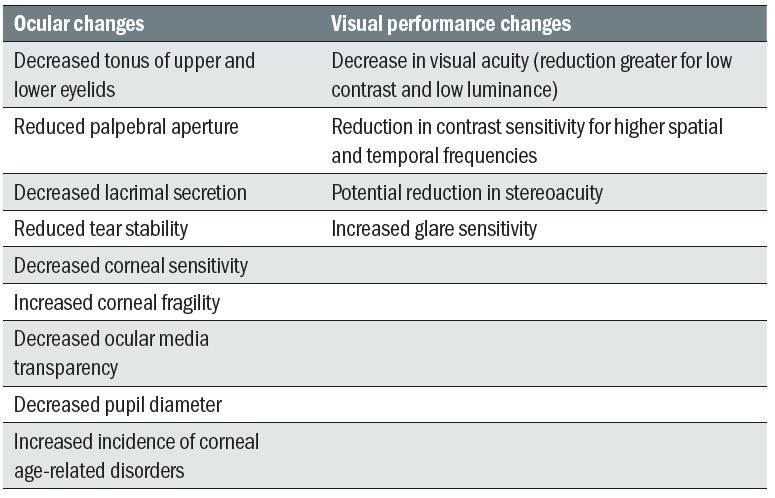
Table 3: The effects of ageing on the eye (Adapted from Woods 19,20)
Prescription considerations
The range of prescriptions available for contact lens wear is extensive, and many of the recommendations made will focus on the best material and modality options for the patient. Vision is often accepted as a ‘given’. However, an awareness of prescription availability is always handy before you launch into making your specific recommendation. Discussing with patients the benefits of contact lenses for them in terms of loss of spectacle magnification and increased field of view is worthwhile at this stage as it gives them further motivation to trial the lenses. Binocular status needs to be considered, and while binocular function can be improved compared to spectacles in the anisometropic patient, contact lenses are unable to correct any prism prescribed within the spectacle prescription. High ametropia, or large astigmatic corrections may lend themselves to different lens types or forms.
Previous CL wear
If patients have worn lenses previously it is important to determine what type of lenses they wore and reasons for ceasing wear. You also want to be aware of any complications they had when wearing contact lenses previously as this may influence your choice of contact lens this time round. Studies continue to show that handling and comfort are commonly cited performance-related reasons for drop out, but visual problems, especially in toric and multifocal wearers, are more of a factor in drop out than previously thought.21 With the newer technologies available, alongside increased prescription ranges, we can often overcome these issues with appropriate contact lens selection.
Financial considerations
In an ideal world, every patient would choose to wear the best product for them. On occasions, financial considerations may necessitate a change in recommendation. It is, however, important not to pre-judge a patient’s financial status or indeed feel protective of their finances. Our role is to listen to their requirements, assess their suitability and from that, make the most appropriate recommendation for them. At this point they need to be informed of the cost and if it is not suitable, then you can work together to see if a more cost-effective option is available and advise them of the loss of benefit – if any – that this option delivers. It is often useful to break cost down to price per wear as this often helps them see it is an affordable option for them. Crucially, although cost is a constant between patients, value can be very different between patients and as health care providers it is important not to judge what value patients attach to the change in lifestyle contact lenses may provide on the basis of cost.
Top tip
Asking patients to bring in a copy of their current medication list can be very useful, rather than relying on a patient’s memory.
Summary
A great contact lens recommendation comes from a combination of understanding the patient’s individual needs and evaluating the eye health. A comprehensive history can help a practitioner enormously with the first element. The information gathered in an initial discussion which will help aid decisions around which material properties are important to consider for the individual patient. With so many areas to cover and often with limited time available, effective communication is key to enable you to extract the information needed from your patient in a timely manner. While it is good to follow a systematic approach to use the time effectively and ensure information is not missed, it is important to maintain a conversational style and good rapport with the patient. In many ways this improves time efficiency as selecting the right lens for the patient’s needs and managing their expectations will reduce follow-up appointments and remedial actions.
Before making any final decisions on which lens to recommend, a comprehensive anterior eye examination and tear film assessment will need to be performed. Using the detailed history alongside the health examination results, means that a recommendation which is truly specific to the patient can be comfortably made.
Theresa Cox is an optometrist, member of the Fitness to Practice Committee for the General Optical Council, a pre-registration supervisor and a paid consultant faculty member for the Johnson & Johnson Institute, UK. Dr Rachel Hiscox is a professional education & development manager, UK & Ireland, Johnson & Johnson Vision Care.
This article is the first in a revised and updated ‘Essential Contact Lens Practice’ series originally authored by Jane Veys, John Meyler and Ian Davies. The article was produced without further input or review from the original authors.
References
- JJV Data on File 2017. Independent Market Research, Global Incidence
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye. 2017;40(1):15-24.
- Sulley A, Young G, Hunt C. Prospective evaluation of new contact lens wearer retention rates. Contact Lens & Anterior Eye, 2018; 41(S1):S4
- GOC: Standards of practice for Optometrists and Dispensing Opticians April 2016
- College of Optometrists Guidance. Available at: https://guidance.college-optometrists.org/guidance-contents/knowledge-skills-and-performance-domain/fitting-contact-lenses/Accessed March 2019
- Abusharha AA. Changes in blink rate and ocular symptoms during different reading tasks. Clin Optom (Auckl), 2017;9:133-138
- The Civil Aviation Authority. Guidance and restriction on lenses. Available at: https://www.caa.co.uk/Aeromedical-Examiners/Medical-standards/Pilots-(EASA)/Conditions/Visual/Guidance-on-the-use-of-contact-lenses-pilots/ Accessed March 2019
- Choo J et al. Bacterial populations on silicone hydrogel and hydrogel contact lenses after swimming in a chlorinated pool. Optom Vis Sci, 2005;82(2):134-7.
- Wu YT, Tran J, Truong M, Harmis N, Zhu H, Stapleton F. Do swimming goggles limit microbial contamination of contact lenses? Optom Vis Sci, 2011; 88(4): 456-60
- Lima CA, Kara-Jose N, Nichols JJ. Indications, Contraindications and Selection of Contact Lenses. In: Contact Lenses in Ophthalmic Practice, Mannis MJ et al. 2004. New York, Springer-Varlag.
- TFOS DEWS II Report Executive Summary. Ocul Surf, 2017;15(4):802-812
- Bussan KA, Robertson DM. Contact lens wear and the diabetic corneal epithelium: A happy or disastrous marriage? Optom Vis Sci, 2011;88(4):456-60
- Ljubimov AV. Diabetic complications in the cornea. Vision Res, 2017;139:138-152
- Park J. Baek S. Dry eye syndrome in thyroid eye disease patients: The role of increased incomplete blinking and Meibomian gland loss. Acta Ophthalmol, 2018; 28
- Hayes VY, Schnider CM, Veys J. An evaluation of 1-day disposable contact lens wear in a population of allergy sufferers. Cont Lens Anterior Eye, 2003;26(2):85-93
- Stapleton F. et al. Risk factors for moderate and severe microbial keratitis in daily wear contact lens users. Ophthalmology, 2012; 119(8):1616-21
- Wolffsohn JS et al. British Universities Committee of Contact Lens Educators (BUCCLE). History and symptom taking in contact lens fitting and aftercare. Cont Lens Anterior Eye, 2015;38(4):258-65
- The College of Optometrists. UK Contact Lens Practice for Children and Young People Survey, 2014. Available at: www.college-optometrists.org/the-college/research/research-projects/contact-lens-practice-children.html. Accessed March 2019.
- Woods RL. The ageing eye and contact lenses – a review of ocular characteristics. JBCL A, 1991; 14(3):115-127
- Woods RL. The ageing eye and contact lenses – a review of visual performance. JBCLA, 1992; 15(1):31-43
- Veys J & Sulley A. Pay Attention to Retention. Optician, 2017; 253(6604):26-30
