Light. It is, of course, essential for life. Without the Sun’s heat and light, the Earth would be a lifeless ball of ice-coated rock. The Sun gives energy to plants which provide food and oxygen for life on Earth. Sunlight is essential for human health, producing Vitamin D. Low levels of sunlight exposure have been associated with higher risks of type 2 diabetes, hypertension and multiple sclerosis.1 From a practical point of view, even indoors, sufficient light is needed to be able to see, study and work.
Light intensity varies enormously. While our ears cope with a relatively small range of volumes, eyes are regularly exposed to an extraordinarily large range of light levels (figure 1). On a typical day, a person will move from a fully adapted dark state upon waking, to indoor illumination levels, spend time viewing illuminated digital devices, head outside into sunlight, and then drive in both daylight and nighttime conditions, likely having spent time in an office with a mixture of artificial and natural light in between. All of these situations require the eye to adapt to many different light intensities, and when that state of adaption cannot be achieved quickly enough, it can result in sensations of discomfort. Averting or shading the eyes, squinting, and wearing sunglasses are all common examples of coping mechanisms that are adopted when faced with bothersome light. It is not hard to appreciate that this constant need for adjustment can be tiring and ultimately uncomfortable.
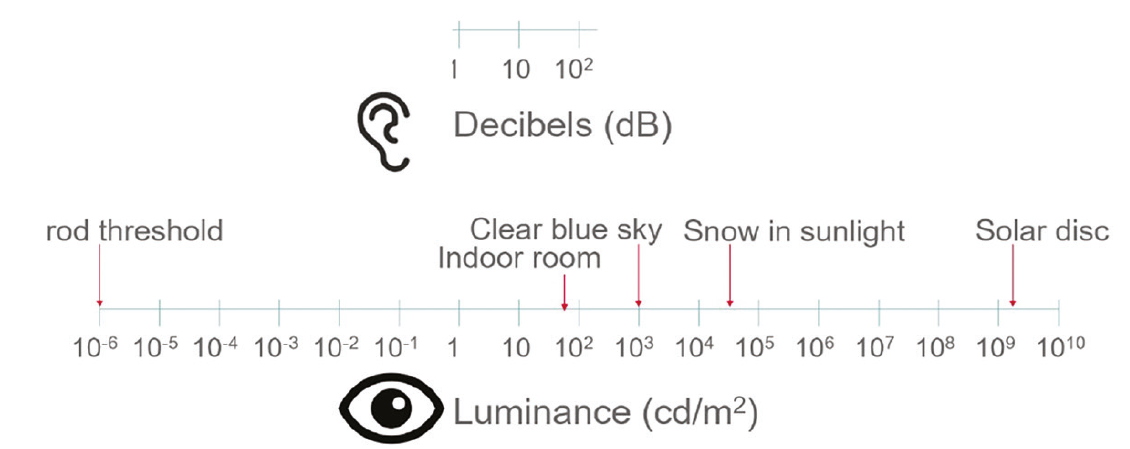
Figure 1: Range of sound levels ears can tolerate compared to range of light intensities eyes are exposed to. (Adapted with permission from Dr Trusit Dave)
Key points
- A typical day filled with normal daily tasks such as viewing digital devices, moving from indoor to outdoor lighting and driving at night presents huge challenges to the visual system.
- Visual experience is defined by a large range of factors beyond simply high contrast visual acuity.
- Nearly two-thirds of consumers are bothered by light on a daily basis.
- Spectral filtration with spectacle and intra-ocular lenses has been shown to improve measures of functional vision compared to clear lenses.
- The clinical results for a first-of-its kind photochromic contact lens are now starting to appear and show unique benefits to improve contact lens wearers’ visual performance and comfort.
Electromagnetic spectrum
The visible part of the electromagnetic spectrum is, of course, just one small band within the whole spectrum of radiation. Across the spectrum as the wavelength increases, the energy of the radiation reduces. For visible light, this means blue light has a shorter wavelength and higher energy than red light. Ultraviolet (UV) radiation sits just beyond visible blue light. It is understood that UV radiation can penetrate cells, causing changes at a molecular level. This can lead to both aging changes and sunburn for skin, and to the formation of pterygia and cataracts,2,3 and an association with age-related macular degeneration for eyes.4,5
High energy visible (HEV) blue light is generally defined as having wavelengths between 400-500nm. Given that HEV light is not filtered by ocular media, and that it is of relatively high energy compared to other sections of the visible light spectrum, concern has been raised about its ability to cause damage in the eye. Some evidence exists for an association between HEV light and progression of severe age-related macular degeneration for example,4,6 and certainly these wavelengths of light have been shown to cause damage to cells in vitro,7-9 however, the in-vivo evidence remains equivocal.10,11 Consumer interest in HEV is perhaps heightened due to the fact that it is emitted from the screens of digital devices, however, it must be appreciated that the amount of HEV emitted by the sun far surpasses that coming from electronic devices (figure 2). In fact, it has been said, in terms of HEV exposure, that 15 minutes outside equates to 10 to 13 hours of looking at digital devices.12
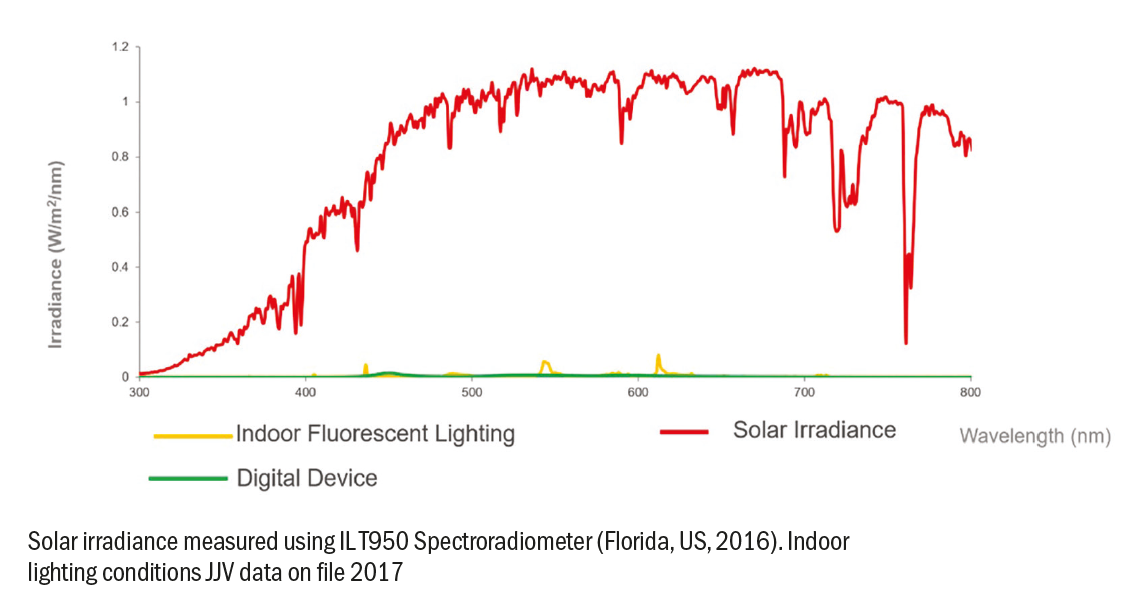
Figure 2: Outdoor and indoor light intensities plotted on the same scale
Defining the visual experience
It is not possible to appreciate how the dynamic range of light intensities that eyes are exposed to affects overall visual performance through just one measurement.13 Measuring high contrast visual acuity with a Snellen letter chart could never capture the richness of a world filled with colour, movement, dynamic changes in light and object distance. The limitations of high contrast visual acuity become clear when the contrast sensitivity function is considered. The contrast sensitivity function (CSF) curve is derived by measuring the threshold for detection of sine-wave gratings of various frequencies across a range of contrasts.14 On the resulting graph, high contrast visual acuity represents just one extreme value, however, the more holistic measure of spatial vision is determined by assessing the area under the curve (figure 3).15 This area represents spatial vision under a large range of conditions,16-18 and is more sensitive to early pathological changes such as cataract and macular degeneration than high contrast acuity alone.15
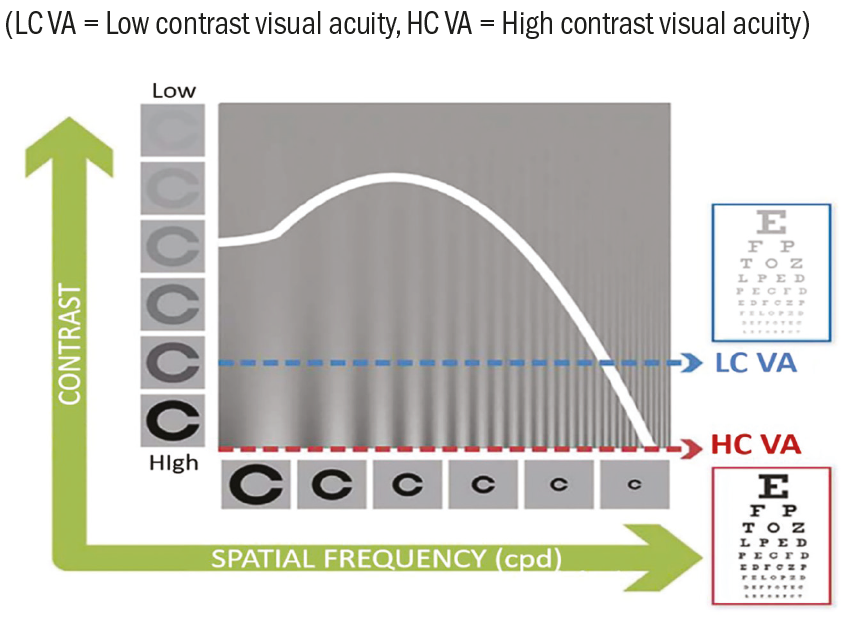
Figure 3: Contrast sensitivity function
What else contributes to the dynamic nature of vision? The optics of the eye change with time: aberrations vary with pupil size and with age, the ability to accommodate on near objects varies with time as well as changes which occur in the tear film both with the blink and longer term with age.19 These all contribute to the quality of the final image that is seen. Moving away from the eye, the environment presents continually changing situations. Light levels vary enormously between indoors and outdoors; the wavelengths of sunlight change over the course of the day, becoming less blue towards the evening. Nighttime additionally introduces significant sources of glare against a dark background.
Factors that affect visual satisfaction and comfort
There are many factors that contribute to overall visual satisfaction. In addition to visual acuity and contrast sensitivity, a recent summary by Hammond et al discussed the effect of light on visual experience.19 Those effects include disability glare, discomfort glare, chromatic contrast, starbursts, squint response and the limitations on visual range due to blue light scatter (table 1).
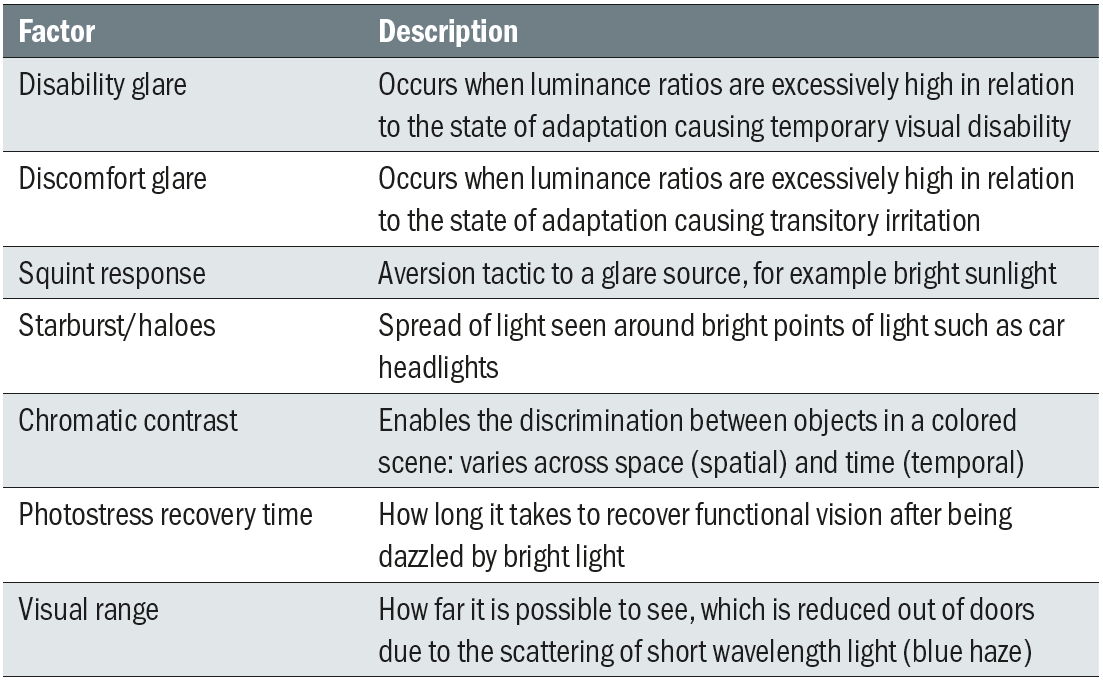
Table 1: Examples of how light can affect visual performance
The typical response to bright light is to squint, shield or avert the eyes to try and reduce the amount of light entering the eye. Looking away from oncoming headlights when driving at night is an example of dealing with bright light using aversion. Those headlights can form starbursts and haloes which add to the sensations of visual discomfort (figure 4).

Figure 4: Example of headlights being a glare source, resulting in starbursts and causing discomfort and potentially disability glare
The way in which the visual system has to continually adapt to changing light levels plays a significant part in the perceived level of overall visual comfort that a patient experiences. Many of these adaptive mechanisms such as squinting, pupil constriction, and avoidance, can lead to sensations of discomfort and fatigue.20,21 These sensations are in addition to other factors known to be associated with ocular discomfort such as uncorrected refractive error, especially astigmatism, oculomotor imbalances, and vergence anomalies.22-24
Visual task also influences comfort, and there is an increasing amount of evidence for the reduction in visual comfort that results from the use of digital devices.25,26 Prolonged use has been linked to eyestrain, blurred vision, dry eye, headache and discomfort, with these detrimental effects being higher in relation to digital device use compared to reading printed materials.27
Overall visual comfort is a complex and dynamic experience.28 Optical factors within the eye, varying with time, environmental conditions and visual task all combine to present a significant challenge to the visual system. For those patients who are also contact lens wearers, a further element must be factored into their visual experience. The contact lens may disrupt the tear film,29 which in turn can directly affect vision. Patients may also experience varying comfort levels associated with contact lens wear. The physical experience of wearing a contact lens, driven by tear quality, lens design, lens age and material,30 must be considered when assessing overall visual satisfaction for this group of patients.
Perhaps unsurprisingly, research demonstrates for wearers of both reusable and daily disposables that the proportion who rate their contact lens performance as excellent declines significantly from insertion to the end of a single day of wear.31 For all three attributes that were rated – vision, comfort and overall satisfaction – consistently only around half the number of subjects were still able to rate their experience as excellent by the end, compared to the beginning, of the day (70% vs 36% vision, 43% vs 20% comfort, and 59% vs 28% satisfaction).31
What do patients experience?
Given the complexities of vision in a world of ever-changing visual tasks and environments, it is important to understand a patient’s actual experience. Photophobia, literally the ‘fear of light’ is perhaps the most severe example of the discomfort experienced with bright light. Photophobia is linked with a number of systemic and ocular conditions such as migraine, traumatic brain injury and both anterior and posterior segment ocular disease.32 An association between dry eye disease and photophobia has also been reported in the literature, with one study finding 75% of subjects with dry eye reporting increased sensitivity to light.33
Although the experience of photophobia has been reported as being common,32 and is likely to cause significant debilitating symptoms, it represents, as mentioned, the extreme end of the spectrum in terms of problematic symptoms caused by light. What is less well covered in the literature is the answer to the broader question: ‘How often are people bothered by light?’ To investigate this further, a survey of US consumers was recently conducted. When asked about light sensitivity, of the 1,000 people surveyed, one in three (34%) said that they were sensitive to light.34 What is interesting, however, is it that when those consumers were asked if their eyes were ever bothered by light during an average day, nearly two-thirds (64%) said that they were.34 The difference in response is significant. The first question suggests that the individual has an actual problem with their eyes – being light sensitive – and is not something people so readily either identify with or wish to admit to. In contrast, discussing moments in their day where light troubles them normalises the question and likely elicits a more accurate response that demonstrates just how widespread the issue is.
Of those consumers who are bothered daily by light, almost all (94%) admit to adopting compensating behaviours to help them cope. These are summarised in table 2, and include shading eyes, squinting, turning off lights, turning down screen brightness, switching rooms and putting on sunglasses.34
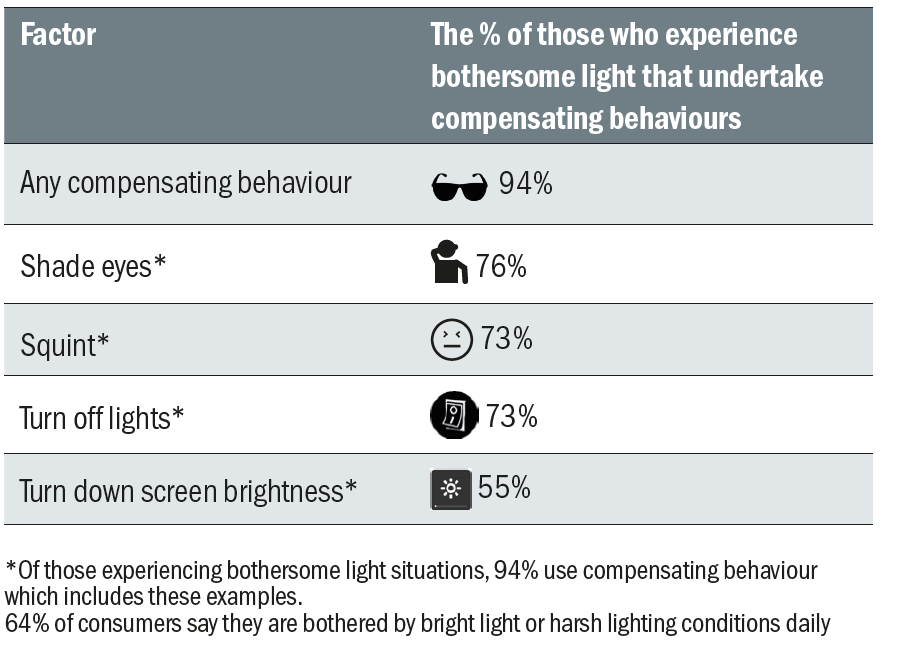
Table 2: Common compensating behaviours employed by consumers to help alleviate the effects of bothersome light
Eye care practitioner (ECP) approach to the potential discomfort caused by light exposure was also evaluated. Across the 250 ECPs surveyed, less than four in 10 (38%) routinely ask about light sensitivities, with the most common reason being ‘because the patient didn’t initiate a discussion about the issue’.34 The gap in communication is clear. In the same way recommendation for contact lenses is held back because ECPs wait for patients to ask, and patients assume they are not suitable if their ECP has not suggested lenses to them, the troublesome experience with light is largely going unnoticed. The survey results show ECPs are not routinely asking about bothersome light, and also that of the nearly two-thirds of consumers who experience problems, only one-third (34%) have proactively mentioned it to their ECP.34
These insights show the majority of people are bothered daily by light, and this is information which will best be established through improved ECP-patient communication asking about bothersome light moments.
Technical solution
Spectral filters
If time is spent in practice uncovering patient concerns with how they cope with changing light conditions, it is of course important to understand what can be done to help them. One of the obvious strategies people employ for bright outdoor daylight is to wear sunglasses. This filtering reduces the amount of light entering the eye, making vision feel more comfortable. In terms of glare, the addition of sunglasses does not change the luminance ratio, but visual comfort is improved because overall retinal illumination is reduced. This can help with both types of glare: increasing tolerance in disability glare and increasing the bandwidth of comfortable visual operation in discomfort glare.
As described earlier, squinting is a typical response to glare. Given that squinting occurs in reaction to excess light, it is reasonable to believe that the use of spectral filters would help to reduce the magnitude of the response. In fact, the size of the squint response, quantified by the change in vertical palpebral aperture height, is used in research to assess discomfort glare.
Spectral filters can also increase visual range by preferentially blocking the scattered blue light associated with haze. Increased visual range can enable the resolution of detail in a scene from further away. This could in theory deliver benefits for patients ranging from improved visual discrimination further down the fairway during a golf game through to improved visual performance for airline pilots. Related improvements have been found with the use of spectral filters to improve spatial vision through better detection of objects in a scene.35,36 Spectral filters have also been shown to result in faster recovery of vision following stressing the visual system with a bright light source.37,38
Photochromic spectacle lenses
Photochromic technology incorporated into spectacles results in a lens which adjusts to the light level it is in, darkening on exposure to UV radiation, and becoming clearer when removed from the UV stimulus. It thus acts as a variable spectral filter. Research has examined visual function while wearing photochromic spectacles compared to clear lenses. Three different partially-activated photochromic lenses were randomly assigned to 75 subjects, and compared to a standard clear polycarbonate lens.39 Measures of disability and discomfort glare, chromatic contrast and photostress recovery were taken, with light sources designed to closely replicate the typical outdoor experience. All elements of visual function measured were significantly better for the photochromic lenses compared to the clear control. This demonstrates photochromic lenses help the subject both to cope better with intense lighting conditions and also adapt back to normal more quickly after being exposed to a photostressor.39
These findings are relatable to real-world situations. To maintain significantly better chromatic contrast enables better discrimination between the coloured borders of objects in a scene (figure 5). A faster photostress recovery time could translate into being able to more easily follow the flight of a golf ball down the fairway against the glare of the sky.

Figure 5: Chromatic contrast is used to distinguish between the coloured objects in this scene
Blue-light filtering
Another visual device which employs spectral filtering are intra-ocular lenses (IOLs). Some IOLs contain visible blue-light filters and, when compared to IOLs with no blue-light filter, subjects with the blue-light filtering IOLs had significantly reduced disability glare and improved measures of safe driving in a driving simulator.40 Again, think of translating those results to driving in the real-world, being able to improve functional vision while driving in the presence of glare is a potentially important safety advantage. Further studies have also shown significant improvements in disability glare, chromatic contrast threshold and photostress recovery in eyes with blue-filtering IOLs compared to non-blue-light filtering controls.38
Conclusion
Light. Essential, for life, for vision? Of course. Difficult to cope with? It would appear so. The visual system is challenged on a daily basis: constantly adapting to the huge range of luminance encountered between indoor and outdoor lighting; coping with photostress from sources of glare and doing its best to maintain the best possible visual range through the disruption of blue light scatter.
Most consumers encounter moments daily where they are bothered by light, and when they do are driven to using compensating behaviours that are at best inconvenient, and, at worst, lead to discomfort and fatigue over time. The use of spectral filters has been shown to improve functional vision compared to clear controls in both spectacle and IOL corrections. A recent study has shown meaningful improvement in the same measures for a first-of-its-kind photochromic contact lens.41 These results will be summarised in a future article, along with key product features and other unique benefits.
In practice, ECPs should remember to ask their patients about bothersome light, and talk to them about the visual corrections options available.
Dr Billy R Hammond PhD, is a Professor in the Brain and Behavioral Sciences program at the University of Georgia and is the Principal Investigator of the Visual Sciences Laboratory. John Buch OD, MS, FAAO is Senior Principal Research Optometrist, Jill Gardere MMR is Senior Manager Global Strategic Insights and David Ruston, BSc, FCOptom, DipCl, FAAO is Director of Global Professional Education at Johnson & Johnson Vision Care, Inc.
Dr Billy R Hammond is a paid consultant to Johnson & Johnson Vision Care, Inc.
References
- Mead MN. Benefits of sunlight: a bright spot for human health. Environmental health perspectives. 2008;116(4):A160-A167.
- Taylor HR. Aetiology of climatic droplet keratopathy and pterygium. The British journal of ophthalmology. 1980;64(3):154-163.
- Taylor HR, West SK, Rosenthal FS, et al. Effect of ultraviolet radiation on cataract formation. The New England journal of medicine. 1988;319(22):1429-1433.
- Cruickshanks KJ, Klein R, Klein BE, Nondahl DM. Sunlight and the 5-year incidence of early age-related maculopathy: the beaver dam eye study. Arch Ophthalmol. 2001;119(2):246-250.
- Loeffler KU, Sastry SM, McLean IW. Is age-related macular degeneration associated with pinguecula or scleral plaque formation? Current eye research. 2001;23(1):33-37.
- Taylor HR, West S, Munoz B, Rosenthal FS, Bressler SB, Bressler NM. The long-term effects of visible light on the eye. Arch Ophthalmol. 1992;110(1):99-104.
- Youn HY, Chou BR, Cullen AP, Sivak JG. Effects of 400 nm, 420 nm, and 435.8 nm radiations on cultured human retinal pigment epithelial cells. J Photochem Photobiol B. 2009;95(1):64-70.
- Zareba M, Skumatz CM, Sarna TJ, Burke JM. Photic injury to cultured RPE varies among individual cells in proportion to their endogenous lipofuscin content as modulated by their melanosome content. Investigative ophthalmology & visual science. 2014;55(8):4982-4990.
- Ratnayake K, Payton JL, Lakmal OH, Karunarathne A. Blue light excited retinal intercepts cellular signaling. Sci Rep. 2018;8(1):10207.
- Darzins P, Mitchell P, Heller RF. Sun exposure and age-related macular degeneration. An Australian case-control study. Ophthalmology. 1997;104(5):770-776.
- Hirvela H, Luukinen H, Laara E, Sc L, Laatikainen L. Risk factors of age-related maculopathy in a population 70 years of age or older. Ophthalmology. 1996;103(6):871-877.
- O’Hagan JB, Khazova M, Price LL. Low-energy light bulbs, computers, tablets and the blue light hazard. Eye (Lond). 2016;30(2):230-233.
- Cheng X, Maggio T, Johnson B, Coles-Brennan C. Life demands more than 20/20. Contact Lens Spectrum. 2017;32(November):33-35, 44.
- Pelli DG, Bex P. Measuring contrast sensitivity. Vision research. 2013;90:10-14.
- Owsley C. Contrast sensitivity. Ophthalmology clinics of North America. 2003;16(2):171-177.
- Arden GB, Jacobson JJ. A simple grating test for contrast sensitivity: preliminary results indicate value in screening for glaucoma. Investigative ophthalmology & visual science. 1978;17(1):23-32.
- Jindra LF, Zemon V. Contrast sensitivity testing: a more complete assessment of vision. Journal of cataract and refractive surgery. 1989;15(2):141-148.
- Shandiz JH, Nourian A, Hossaini MB, et al. Contrast Sensitivity versus Visual Evoked Potentials in Multiple Sclerosis. Journal of ophthalmic & vision research. 2010;5(3):175-181.
- Hammond B, Renzi-Hammond LM, Buch J, Nankivil D. Measuring total visual experience Contact Lens Spectrum. 2018;33(December 2018):32-38.
- Thorud HM, Helland M, Aaras A, Kvikstad TM, Lindberg LG, Horgen G. Eye-related pain induced by visually demanding computer work. Optometry and vision science. 2012;89(4):E452-464.
- Lin Y, Fotios S, Wei M, Liu Y, Guo W, Sun Y. Eye Movement and Pupil Size Constriction Under Discomfort Glare. Investigative ophthalmology & visual science. 2015;56(3):1649-1656.
- Wiggins NP, Daum KM, Snyder CA. Effects of residual astigmatism in contact lens wear on visual discomfort in VDT use. Journal of the American Optometric Association. 1992;63(3):177-181.
- Jaschinski W. The proximity-fixation-disparity curve and the preferred viewing distance at a visual display as an indicator of near vision fatigue. Optometry and vision science. 2002;79(3):158-169.
- Wee SW, Moon NJ, Lee WK, Jeon S. Ophthalmological factors influencing visual asthenopia as a result of viewing 3D displays. The British journal of ophthalmology. 2012;96(11):1391-1394.
- Thomson WD. Eye problems and visual display terminals--the facts and the fallacies. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians. 1998;18(2):111-119.
- Portello JK, Rosenfield M, Bababekova Y, Estrada JM, Leon A. Computer-related visual symptoms in office workers. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians. 2012;32(5):375-382.
- Chu C, Rosenfield M, Portello JK, Benzoni JA, Collier JD. A comparison of symptoms after viewing text on a computer screen and hardcopy. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians. 2011;31(1):29-32.
- Buch J, Hofmann G, Ruston D. Getting into your comfort zone. Contact Lens Spectrum. 2018;TBC(TBC):TBC.
- Craig JP, Willcox MD, Argueso P, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Contact Lens Interactions With the Tear Film Subcommittee. Investigative ophthalmology & visual science. 2013;54(11):TFOS123-156.
- Jones L, Brennan NA, Gonzalez-Meijome J, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design, and care subcommittee. Investigative ophthalmology & visual science. 2013;54(11):TFOS37-70.
- Mathews K, Daigle B, Alford. Exploring variability in soft contact lens performance. Optician. 2015;251(6543):32-34.
- Digre KB, Brennan KC. Shedding light on photophobia. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2012;32(1):68-81.
- Galor A, Levitt RC, Felix ER, Sarantopoulos CD. What can photophobia tell us about dry eye? Expert Rev Ophthalmol. 2016;11(5):321-324.
- JJV Data on File 2018: Bothersome Light Need Prevalence Substantiation.
- Luria SM. Vision with chromatic filters. American journal of optometry and archives of American Academy of Optometry. 1972;49(10):818-829.
- Wolffsohn JS, Cochrane AL, Khoo H, Yoshimitsu Y, Wu S. Contrast is enhanced by yellow lenses because of selective reduction of short-wavelength light. Optometry and vision science. 2000;77(2):73-81.
- Hammond BR, Bernstein B, Dong J. The Effect of the AcrySof natural lens on glare disability and photostress. American journal of ophthalmology. 2009;148(2):272-276 e272.
- Hammond BR, Jr, Renzi LM, Sachak S, Brint SF. Contralateral comparison of blue-filtering and non-blue-filtering intraocular lenses: glare disability, heterochromatic contrast, and photostress recovery. Clinical ophthalmology (Auckland, NZ). 2010;4:1465-1473.
- Renzi-Hammond LM, Hammond BR, Jr. The effects of photochromic lenses on visual performance. Clinical & experimental optometry. 2016;99(6):568-574.
- Gray R, Perkins SA, Suryakumar R, Neuman B, Maxwell WA. Reduced effect of glare disability on driving performance in patients with blue light-filtering intraocular lenses. Journal of cataract and refractive surgery. 2011;37(1):38-44.
- Hammond B, Renzi-Hammond LM, Buch J, Cannon J, Toubouti Y. A Contra-lateral Comparison of the Visual Effects of Clear vs. Photochromic Contact Lenses. AAO; 2018; San Antonio, TX.
