As the population of the UK continues to grow so does the opportunity for eye care practitioners (ECPs) to grow their contact lens business. Technological advancements resulting in new designs of contact lenses and materials mean that we have a growing number of lens options to fit an expanding patient base. Office of National Statistics figures show that the largest proportion of the population in 2013 were aged 45-49 years, very closely followed by 40-44 year-olds (Figure 1). This group are also the most likely to be seeking advice about their eyes and eye care, and for many a presbyope this will be for the first time. The number of presbyopes is predicted to increase significantly in the coming decades (1.8 billion globally by 20501).
[CaptionComponent="2815"]
Presbyopia impact
We live in a world where information can be accessed at click of a mouse or the touch of a screen on mobile devices such as phones and tablets. Early presbyopes may not realise their vision is changing but can become frustrated when a simple task, such as reading texts or e-mails on a mobile phone, becomes difficult. As such, it falls to ECPs to ensure that we educate our patients from their mid-30s onwards of the insidious change to near vision that will inevitably appear and reinforce the fact that there are solutions available as their vision changes.
Presbyopia is caused by age-related elasticity changes in the crystalline lens and its capsule. To understand the progression, consider that the average 12-year old European child can comfortably maintain accommodation of 12.00DS, allowing a comfortable nearest point of clear vision to be held at about 8cm. The average 48-year-old European male adult (and gender and ethnicity have influence) might only manage 3.00DS, allowing a nearest point of clear vision of about 33cm. Indeed most authorities take a reduction below 3.00DS of accommodation to be the point at which presbyopia begins. The average 60-year-old European adult has minimal accommodation and relies upon depth of focus (aided by pupil miosis) or artificial assistance such as with lenses.1
Communication challenges
Presbyopic ECPs are likely to be in a better position when it comes to appreciating the impact of presbyopia and so be able to empathise with new presbyopes. It is more of a challenge for a younger ECP to appreciate fully the day-to-day frustration of presbyopia and care should be taken not to belittle or minimise the apparent challenge facing the patient.
Predicting and communicating the expected changes related to presbyopia at the earliest stage may also make it easier for ECPs to discuss the eventual move into spectacles and contact lenses for near vision tasks. Hopefully, predicting presbyopia will strengthen the patient/ECP relationship and make the transition much smoother. An informed patient may have fewer problems with adaptation if they have been fully aware of and understand any management plan in advance.
It is also a mistake to assume that a presbyope will want the quickest or ‘easiest’ solution. Changes in near vision will direct patients back to your clinic. It is at this time that all available and suitable options, including the multifocal contact lens option, are considered. Fitting these early presbyopes (those with no previous correction having near vision corrected for the first time are often referred to as neophytes) very often has the most successful outcome. You have a willing patient who is looking to you for the answer to their visual problem.
Making a case for multifocal contact lenses for an existing presbyope corrected by spectacles is a little more interesting. Some will attend for a routine eye examination and careful questioning may elicit situations where glasses are a nuisance or even an unwanted option. Many established presbyopes are likely to be retired. This often means they may lead a more active, less sedentary, lifestyle. They may take up and spend more time on new sports or hobbies for which spectacles may be a hindrance. It’s often useful to talk to patients about their ‘visual wardrobe’ or range of corrective solutions. In today’s hectic world one vision correction isn’t necessarily the best option. It is also existing spectacle wearing presbyopes that may subscribe to misinformation about lack of contact lens suitability. Advising them of contact lens options may come as a pleasant surprise.
Perceived barriers
The use of multifocal contact lenses in correcting presbyopia is still seen by many patients and ECPs as an option available for the few. There are many reasons for this, including:
- Spectacles are seen as a quick and easy fix often available instantly
- Challenges in meeting patient visual expectations were well known with early multifocal designs and this may have left a lasting negative impression on ECP and patient alike
- Many think of multifocal as difficult to fit
- Increased chair time is usually needed when fitting multifocal contact lenses
- ECPs might consider the process expensive both in terms of chair time and ‘wastage’ if more than one design is tried.
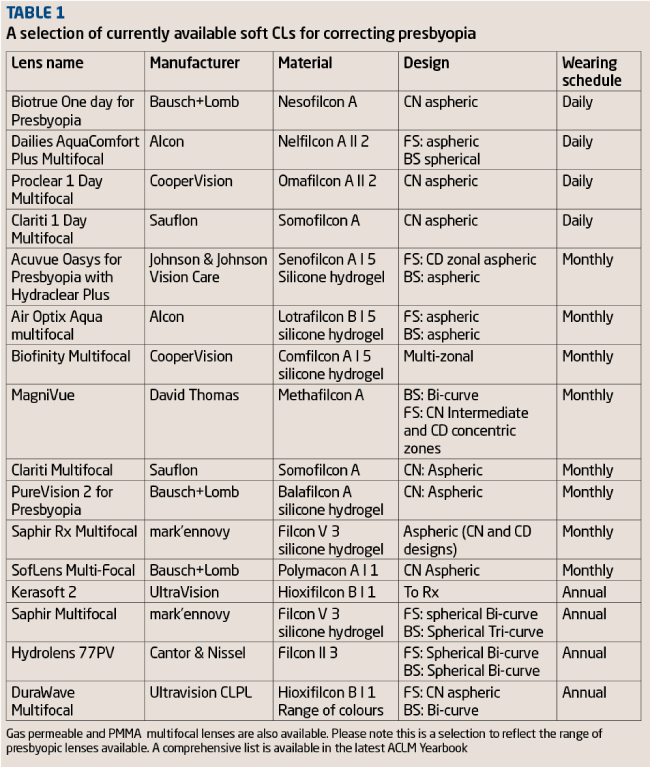
Although multifocal contact lenses have been around since the 1950s,2 the number of designs and available wear modalities have significantly increased in recent years. ECPs need to be aware of this expanding range if they aim to offer the best available management options to their patients. It is useful for ECPs to become familiar with a range of multifocal CLs of differing materials, different optical designs and wearing regimes. It should then be possible to find the one lens that best suits an individual patient and allows an alternative if the initial lens selection is rejected. Table 1 shows a selection of currently available lenses of different designs, materials and wearing schedules.
Dropout rates
Contact lens dropout increases with age. Many factors can contribute to this. Contact lens related discomfort is thought to be the biggest hurdle to overcome, followed by vision. After the age of 40, dropouts are often the result of combined comfort and vision issues.3
Contact lens dropout due to dryness symptoms increases with age and it is important that ECPs proactively discuss and manage dry eye conditions. Dry eye management is a rapidly evolving area and we are increasingly spending time in clinic treating dry eye. Further discussion on this will continue in Part 3 of this series.
Almost as many patients drop out of contact lens wear when over 40 due to poor vision as they do due to discomfort and convenience.
As well as presbyopia and the near vision problems it creates, astigmatism in adults changes with age from with-the-rule in young adults to against-the-rule in older patients.4 The prevalence of astigmatism also increases with age.5 There may further be a need to consider more frequent refraction to ensure that the patient is wearing the most suitable contact lens correction.
Careful discussion can reveal much about a patient’s day-to-day visual needs and often this is poorly correlated with high contrast acuity targets in the consulting room. In reality, fitting multifocals is more about giving all-round comfortable vision rather than attempting to correct vision. A useful, although somewhat flippant, rule of thumb used by the authors is ‘think 6/happy and N mobile phone.’
Acceptable distance vision through a multifocal is essential and most patients will return unhappy if their distance vision is unsatisfactory, especially for driving.6 The authors’ experience is that successful multifocal contact lens wearers should achieve the vast majority of their daily visual tasks without thinking about their vision. The remaining challenges will usually be reported as a lack of clarity when attempting very small print (medicine bottles, ingredients on packaged foods etc) and in these instances a separate pair of spectacles is usually advised to supplement near vision.
In the past, many practitioners will remember ‘dropping minus’ or ‘adding plus’ binocularly to existing corrections to help with near tasks. This practice has now been virtually eliminated and presbyopes can be upgraded to one of the new generation of multifocal lenses with relative ease.
Multifocals versus monovision
Monovision has been the preferred choice of contact lens correction for presbyopia by ECPs for decades and is still very much prominent even among our most newly qualified colleagues.
Although monovision may be seen as a quick solution for correcting a presbyopic patient, it does start to fail as the reading add increases and depth perception is disturbed. A recent study published by Fernandes et al reviewed the objective and subjective results for vision corrected by each method and concluded that stereoacuity was significantly better in patients wearing multifocal contact lenses as compared to monovision.7 The study also found that, while providing minimal binocular disruption compared to monovision, continued reported improvement in vision was observed from 1-15 days, which suggested an adaption effect in multifocals that was not observed with monovision.
While the authors advocate the use of multifocal contact lenses in the first instance for the correction of presbyopia, there are times when, depending on the visual demands of the patient, both modified or enhanced monovision are useful.
This entails emphasising distance correction for one eye, typically the dominant eye, and near correction in the other eye. This works well for patients who want or need better distance or near vision than is typically achievable using multifocals without bias alone. The resulting prescription may include different adds, a single-vision and multifocal combination, or a single-vision toric and multifocal combination.
Today’s presbyopes
The currently available reusable multifocals that are replaced monthly, or less, mostly utilise simultaneous vision correction of either centre near or centre distance design or a combination of the two and are available in either hydrogel or silicone hydrogel. Some materials are licensed for overnight or even continuous wear regimes. For the occasional lens wearer, one day multifocals are available, all of which use the centre near design. The greater the range of options, the more likely the success.
Today’s generation of middle-aged consumers could not be more different from stereotypes of older people. They want to remain contemporary and fashionable well into their 40s, 50s, 60s and beyond. To stop trying would, they feel, be an admission of defeat, a surrender to the horrors of old age. They don’t want to grow up to resemble their parents; they want to carry on looking like their children for as long as possible.
We are used to hearing the adage 60 is the new 40; today’s presbyopes are more active, health and fashion conscious and better informed than previous generations. We are surely failing in our duty of care not to inform them of all the visual correction options available to them to allow them to continue to live life to the full.
How do we identify suitable patients?
Key indications of the appropriateness of mentioning multifocal correction include:
- Early asthenopic symptoms of presbyopia
- Frustration with loss of near vision reports
- Increased reliance on spectacles, often reluctant
- Current contact lens wearers in their later 30s
- Presbyopes clearly expressing motivation to try something new or different to previously offered solutions.
Talking to all patients about lifestyle and hobbies may elicit an indication for contact lenses, particularly if your patient has taken up a new sport or activity. This is an essential part of the history and symptoms but often is the least thoroughly explored.
It is true that many spectacle wearers have no interest in contact lenses, but there are those who hate wearing spectacles but have never been given an option, while many contact lens wearers do buy spectacles and this sale may also go to the practitioner providing them with contact lenses. A European study into the profitability of the contact lens patient discovered that they are 60 per cent more profitable than spectacle patients alone because they are more likely to have a range of corrections, back up spectacles to their contacts as a minimum.8
Furthermore, ECP recommendation is all important, with one study showing six times more patients being fitted with contact lenses when a proactive approach was taken by their ECP.9
Another way to consider introducing the contact lens correction option was reviewed in the EASE study.10 Ninety-one subjects were randomly assigned into two groups, with the test group being offered contact lenses as an aid to spectacle dispensing. The contact lens wearing group not only spent 32 per cent more on spectacles than the control group, but more relevant to this article, 33 per cent of this test group went on to purchase contact lenses within three months of purchasing their spectacles.
Conclusion
Contact lens manufacturers have made giant leaps in technology, both in materials and design. However, it is still left to ECPs to inform presbyopes of the option of multifocal contact lenses. Having introduced the concept to a patient identified as suitable, the next article will take a look at the process of initial fitting.
Model answers
(The correct answer is in bold text)
1 In 2013, which of the following age groups represents the greatest proportion of the UK population?
A 25 to 25
B 35 to 39
C 45 to 49
D 44 to 45
2 What is the expected level of accommodation for a 45 year old?
A 12.00DS
B 8.00DS
C 3.00D
D 1.00D
3 Which of the following statements about astigmatism with age is true?
A It tends towards with-the-rule
B It tends towards against-the-rule
C It tends to stay constant after teenage years
D It tends to reduce with age
4 Which of the following statements is true regarding monovision?
A It establishes better stereoacuity than multifocal contact lenses
B Patients continue to adapt over two weeks after initial fitting
C It is more appropriate for higher additions
D It is still a viable option if multifocals are rejected
5 Which of the following is one conclusion from the EASE study?
A Presbyopes prefer spectacles
B More patients will want to try contact lens wear if fitted with them to choose their spectacles
C Contact lenses should always be offered as back up to spectacles
D Patients will be less likely to try contact lenses is proactively recommended to try them
6 Which of the following might be most appropriate for a patient to assess their vision levels through multifocal contact lenses?
A Monocular Snellen acuity
B Binocular Snellen acuity
C Binocular low contrast targets
D Binocular variable contrast targets
References
1 Holden B et al. Global vision impairment due to uncorrected presbyopia. JAMA Ophthalmology, 2008.
2 Bowden, T. Contact Lenses:The Story, 2009, Bower House Publications.
3 Akerman, Dwight. 40 is the new 20/20 – Presbyopia equals opportunity CL Spectrum, 03.01.2010.
4 Leung, TW, Lam, AK, Deng, L Kee, CS. Characteristics of astigmatism as a function of age in a Hong Kong Clinical population. Optom Vis Sci, 2012; Jul, 89(7): 984-92.
5 Asano K, Nomura H et al. Relationship between astigmatism and aging in middle-aged and elderly Japanese Jpn J Ophthalmol, 2005; 49: 127-133.
6 Chu, BS et al. The effect of presbyopic vision corrections on night time driving performance. Invest Ophthalmol Vis Sci, 2010, Sep; 51 (9): 4861-6.
7 Fernandes, P et al. Adaption to Multifocal and monovision contact lens correction Optom Vis Sci, 2013; Mar, 90(3):228-35.
8 Ritson M. Which patients are more profitable? CL Spectrum, 03.01.2006.
9 Jones, L, Jones D, Langley C, Houlford M. Reactive or procative CL fitting – does it make a difference? BCLA Journal, 1996; 19:41-43.
10 Atkins NP, Morgan SL, Morgan PB. Enhancing the approach to selecting eyewear (EASE); a multicentre, practice-based study into the effect of applying contact lenses prior to spectacle dispensing CLAE, 2009 Jun:32(3) 103-7.
Indie Grewal is an optometrist and holds an FBCLA. He is franchise partner with Leightons in St Albans. Keith Tempany is the owner of an independent practice in Dorset and was the winner of Contact Lens Practitioner of the Year in this year’s Optician Awards