Silicone hydrogel (SiHy) lenses have come a long way since they were first introduced for extended wear. From the plasma oxidation or surface treatment processes of the earliest lenses to the naturally wettable options available today, materials have been repeatedly modified in an effort to provide a more comfortable wearing experience for patients.
SiHy lenses offer excellent ocular health benefits and patient comfort, and many clinicians have made SiHy contact lenses their preferred lens of choice for planned replacement lenses. Current UK prescribing trend data for 2018 revealed that 63% of daily disposable fits were in SiHy materials ‘v’ 90% of reusable daily wear were in SiHy compared to hydrogel materials.1
The goal of this article is to highlight to eye care professionals the ocular health benefits of fitting SiHy daily disposable lenses. A review of the literature will provide the reader with a better understanding of SiHy material benefits, consequences of corneal hypoxia, perceived SiHy barriers, as well as today’s contact lens market trends.
Silicone Hydrogel: History
Like silicone hydrogel, daily wear lenses have also evolved, and the marriage of material and the daily disposable modality has led the industry to create options that more closely align with the needs of modern patient populations. In 1984, the seminal study by Holden and Mertz 2 evaluated the relationship between corneal oedema and hydrogel lens oxygen transmissibility for daily and extended lens wear. They determined the critical oxygen levels to avoid corneal oedema for daily and extended wear contact lenses to be values of 87 x 10-9 oxygen transmissibility (Dk/t) for overnight wear and 24 x 10-9 for daily wear.3
Table 1: The consequences of limited oxygen
That study was the last time anyone looked closely at oxygen needs for daily wear, and it only addressed the necessity of oxygen to avoid corneal swelling in the average eye. How different are patients’ lives today than they were in 1984? How much has technology and our understanding of the ocular surface evolved since then? Are 1984 standards still relevant today?
Respectfully, Holden and Mertz established the original benchmark on oxygen transmission and corneal oedema, but recent literature substantiates the need to re-evaluate these standards. A 2015 article by Fonn and Sweeney3 addresses the fact that the Holden and Mertz daily wear benchmark has not been challenged, and reviews why silicone hydrogel daily disposable lenses are their preferred option for daily wear. Fonn and Sweeney describe how ‘the criterion does not address the potential chronic effects of exposing corneas to a lower level of oxygen, nor does it address individuals’ corneal needs for oxygen.’ There is an assumption that some patients who exhibit high levels of corneal swelling will develop signs and symptoms of hypoxia when wearing contact lenses with the 24 x 10-9 level of Dk/t, even though this Dk/t meets the criteria for daily wear.4
The authors cite numerous studies as evidence that all hydrogel contact lenses cause hypoxia, which can result in some unacceptable – and sometimes irreversible – corneal and ocular changes.4 Although the risks are smaller with daily wear than they are with extended wear, the bottom line is that the risks still exist.
However, these risks can be reduced by prescribing silicone hydrogel daily disposable contact lenses. The authors assert that ‘sentiment has been expressed that silicone hydrogel lens materials should be routinely prescribed over traditional hydrogel lenses for daily wear.’ The authors also state that given ‘the availability of SiHy daily disposable lenses on the market today, this is especially sensible for patients who have greater oxygen demands and who have to wear thicker lenses because of higher and more complex prescriptions.’4
While often prescribed in hydrogel materials, daily disposable lenses may not be ‘good enough’ to maintain ocular health in all wearers. Research shows that even daily disposable wearers often do not follow safe wearing instructions and have lifestyles that present significant challenges to safe, comfortable lens wear.
In 2015, Dumbleton and colleagues 5 investigated compliance with daily disposable contact lens (DDCL) wear and investigated the re-use of lenses according to country and DDCL material worn. During this study, optometrists in four countries asked 805 daily disposable contact lens wearers to participate in a survey regarding their wearing habits. They found that the average daily disposable lens wearer wore their lenses for an average of 14 hours per day. In addition, 75% of respondents reported napping in their lenses, 28% reported sleeping overnight in their lenses, and 59% reported wearing their daily disposable lenses for seven days. The authors also noted that overnight lens wear of DDCL may place patients at a greater risk of corneal infection. They concluded that it is imperative that eye care professionals (ECPs) exercise caution in what materials they are dispensing for DDCL wearers who may be napping and sleeping in their lenses. They recommended that ECPs properly educate and counsel all DDCL-wearing patients on the importance of appropriate lens wear and compliance.
Material Benefits of Silicone Hydrogel
The benefits of oxygen transmissibility should not be understated. Good oxygen transmissibility lessens the incidence of chronic and acute hypoxia, limbal hyperaemia, and corneal neovascularisation. In 2006, Holden and colleagues 6 asserted that Dk (oxygen permeability) and Dk/t (oxygen transmissibility) do matter. According to the authors, ‘the clinical imperative remains to maximise oxygen transmissibility for all lens wearers.’
The authors pointed out that the eye has the greatest likelihood of good health if it receives the highest possible levels of oxygen, and that wearers need the highest Dk possible for one simple reason: the cornea is designed for ‘normoxia’ during the day and the (lower) levels of oxygen provided through the eyelid at night. Any reduction in oxygen availability requires some adjustment by the cornea, and long-term compromise will, ultimately, be deleterious to corneal health (see table 1).
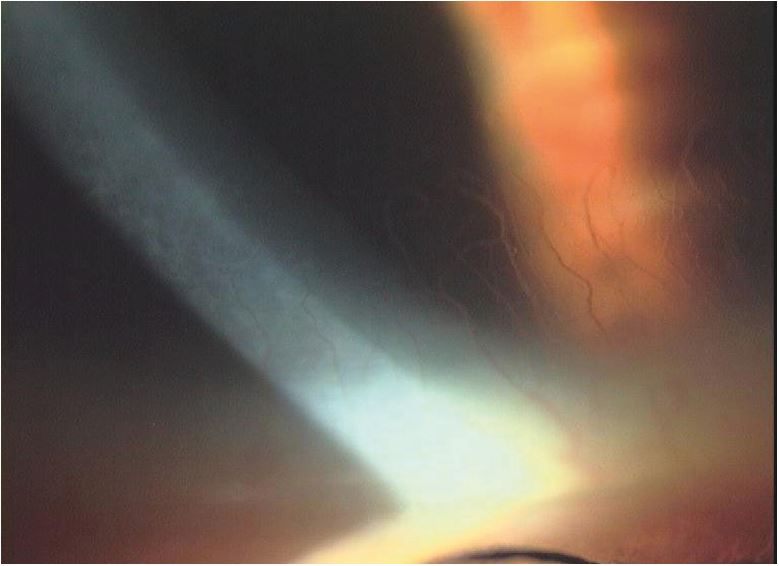
Severe corneal neovascularisation – a thing of the past?
Hypoxia and Hyperaemia
Brennan and Morgan 7 asserted that all hydrogel lenses induce corneal hypoxia. They further reported that open eye wear of hydrogel lenses leads to limbal hyperaemia, the most obvious sign of hypoxia that occurs in most people during hydrogel lens wear. The oxygen permeability benefits of silicone hydrogel lenses, therefore, provide significant health advantages for the wearer.
A study by Morgan and colleagues 8 was designed to derive central and peripheral Dk/t thresholds for soft contact lenses to avoid hypoxia-induced corneal swelling (increased corneal thickness) during open eye wear. Central and peripheral corneal thicknesses were measured in a masked and randomised fashion for the left eye of each of seven subjects before and after hours of afternoon wear of five conventional hydrogel and silicone hydrogel contact lens types offering a range of Dk/t from 2.4 to 115.3 units. Curve fitting for plots of change in corneal thickness versus central and peripheral Dk/t found threshold values of 19.8 and 32.6 units necessary to avoid corneal swelling during open eye contact lens wear for a typical wearer.
Although some conventional hydrogel soft lenses are able to achieve this criterion for either central or peripheral lens areas (depending on lens power), in general, no conventional hydrogel soft lenses meet both the central and peripheral thresholds. However, silicone hydrogel contact lenses typically meet both the central and peripheral thresholds, and the use of these lenses, as the authors concluded, avoids swelling in all regions of the cornea.7
The oxygen advantage appears to be equally as important in daily wear as it is in extended wear. As described earlier, oxygen capabilities also must apply across the entire lens.
According to Brennan and Morgan,9 most values for hydrogel lenses give a false impression of their oxygen capabilities. They suggested that a Dk/t of above 20 is the desirable range for daily wear. Many hydrogel lenses on the market today provide a Dk/t of 10 across the entire lens (centre to periphery) and due to this, Brennan and Morgan recommend SiHy daily wear contact lenses to avoid hypoxia.9
In addition, Covey and colleagues 10 studied whether subjects wearing SiHy lenses could be discriminated from non-wearing subjects. This study was a prospective masked assessment of 32 subjects, 16 of whom wore experimental high-Dk soft contact lenses and 16 of whom did not wear contact lenses. Tear film characteristics, staining and vascularisation of the cornea, conjunctival staining, and the presence of microcysts in the corneal epithelium were assessed using slit lamp microscopy.
The endothelium was examined for polymegathism. No differences were found between the two groups in any of the studied parameters except for the high Dk lens-wearing group, which had twofold more tear film debris and 2.5-fold more conjunctival staining than the non-lens-wearing subjects. There were no observable hypoxia-associated effects in SiHy lens wearing eyes.10
In 2013, Sweeney 11 reviewed the literature to determine whether or not silicone hydrogel lenses have eliminated corneal hypoxia. Results from clinical studies, including short-term laboratory studies and retrospective and prospective clinical trials that have assessed the cornea’s response to silicone hydrogels, were evaluated. The review revealed that silicone hydrogels have eliminated the physiological signs associated with lens-induced hypoxia, including ocular and limbal redness, neovascularisation, epithelial microcysts, and endothelial responses. Responses to these markers are similar to those observed with non-lens wearers. Sweeney concluded that SiHy lenses have effectively eliminated hypoxia for most patients, regardless of wearing schedule.11
In addition, Morgan and colleagues 12 compared neophytes who wore daily disposable silicone hydrogel lenses to non-lens wearing controls and, after one year, bulbar and limbal hyperaemia were clinically equivalent between the wearers and non-lens wearing controls.
Comfort
A common concern among eye care practitioners is contact lens comfort. Some practitioners believe hydrogel lenses perform better on the comfort scale compared with silicone hydrogel lenses. One reason for this assessment could be the hydrophobic nature that is inherent in silicone. The good news is that many manufacturers have discovered that combinations of different materials as well as changing the shape and structure of silicone can improve the hydrophilic properties, while still maintaining great oxygen transmissibility. A retrospective analysis by Diec and colleagues 14 on approximately 40 participants compared a silicone hydrogel daily disposable with hydrogel daily disposable contact lenses. No differences in comfortable wearing time were found between groups (P=0.41); Comfort at insertion, during day, and end of day was also no different (P=0.71).
Research shows that when soft lens patients in low Dk materials switched to a high Dk/t silicone hydrogel daily wear, they experienced improvements in corneal and conjunctival signs of health and a reduced prevalence of uncomfortable wear and end-of-day dryness. A large, multisite (United States and Canada), single-masked study 15 enrolled experienced daily wear, low Dk/t, two-week replacement soft contact lens wearers. Patients were refitted into a silicone hydrogel lens for a two-week period. After two weeks, subjects returned for assessment to compare the silicone hydrogel lenses with their habitual lenses. Data from 760 subjects were analysed. Biomicroscopy evaluations showed improvements in signs related to corneal health with silicone hydrogel. Conjunctival and limbal redness, corneal neovascularization, corneal oedema, and corneal and conjunctival staining all decreased significantly from baseline. Silicone hydrogel lenses performed better than habitual lenses in terms of comfort, symptoms, and overall preference. When wearing silicone hydrogel lenses, significantly fewer subjects reported problems compared with their habitual lenses, including uncomfortable lens wear (-20.3%), redness (-44.5%), dryness during the day (-40.2%), and dryness at the end of the day (-34.4%). What is more, 47.9% of subjects reported that they could wear the silicone hydrogel lenses longer than their habitual lenses. At the end of study, among those with a preference, a significantly greater proportion of patients (60.3%) preferred the silicone hydrogel lenses to their habitual lenses.15
Refitting existing low Dk lens wearers with SiHy lenses on a daily wear basis can result in a decrease in hyperaemia, which may result in an improvement in symptoms of dryness and discomfort. Investigators studied the clinical performance and physiological responses in successful long-term wearers of conventional hydrogel lenses when refitted with daily wear SiHy contact lenses.16 Eighty-seven successful soft lens wearers were refitted and returned after one week, one month, and two months of daily wear with SiHy contact lenses. Ninety-three percent of subjects were successfully refitted. Both objective and subjective evaluations showed that bulbar and limbal hyperaemia decreased significantly in all quadrants during the study. Subjects reported a reduction in end-of-day dryness and improved end-of-day comfort compared with their habitual lenses. No significant changes in refractive error, tarsal papillary response, corneal curvature, or corneal thickness were found during the study. The authors concluded that ‘Silicone hydrogel lenses on a daily wear basis can result in a decrease in hyperaemia, which may be significant for some subjects and also results in improvement in symptoms of dryness and a decrease in discomfort.’16
Silicone hydrogel lenses on a daily wear basis can result in a decrease in hyperaemia, which may be significant for some subjects and also results in improvement in symptoms of dryness and a decrease in discomfort.’16
Another two-part study 17 estimated the prevalence of problems occurring with soft contact lenses wearers and tested the effect of refitting patients with silicone hydrogel lenses. Part one utilised 1,092 lens wearers. Fifty-two percent (564 wearers) had some qualifying criteria, with dryness reported by 23%, discomfort reported by 13%, and 27% reported at least two hours of uncomfortable wear. Six percent of subjects had qualifying limbal hyperaemia; 10% had bulbar hyperaemia; and 12% had corneal staining. In Part two, 112 of the 564 wearers classified as ‘problem patients’ were refitted with silicone hydrogel lenses and reassessed two weeks later. After refitting all 112 problem patients, 75% had less dryness; 88% had better comfort (P<0.0001 each); and 76% had fewer uncomfortable hours of wear (P=0.004). Although the average wearing time was unchanged, comfortable wearing time increased significantly (10.4 to 11.6 hours) (P=0.004). All 35 eyes with qualifying limbal hyperaemia before the refit also improved (P<0.0001), as did 80% (40 of 50) of those with bulbar hyperaemia (P<0.0001) and 76% (26 of 34) of those with corneal staining (P=0.005).
The authors noted that ‘Significant improvement in both signs and symptoms … less dryness, better comfort and fewer hours of uncomfortable wearing time were achieved with silicone hydrogel refitting.’18
Reducing Contact Lens Dropout
When patients experience problems with their contact lenses, it can result in contact lens dropout, which can have a negative effect on the financial side of a practice. Silicone hydrogel contact lens fits may be key in maintaining a happy, healthy contact lens population, which, in turn, would help maintain a successful contact lens business.
Current and lapsed contact lens wearers residing in Canada were recruited using Facebook to take part in an online survey investigating contact lens-wearing experiences during 2008 to 2010 and to establish the percentage of participants who temporarily and permanently discontinued CL wear during the period surveyed.17 Their primary reported reasons for discontinuation were discomfort (24%), dryness (20%), red eyes (7%), and expense (7%).
Perceived Barriers
Commonly reported obstacles to SiHy fits are cost, allergic response, and parameters. Let us discuss these in more depth.
Cost
In a 2015 survey,20 patients considered health one of the most important factors when choosing between two contact lens brands. Ninety-five percent of contact lens wearers who said health was important reported willingness to pay more for contact lenses that ensure eye health.
Allergy
Silicone allergy is still up for debate. A literature review 19 was undertaken to review evidence concerning the role of an allergic reaction to silicone as the basis for the reported increase in contact lens-associated infiltrates in wearers of silicone hydrogel contact lenses. As the authors clearly state, immune cells cannot interact with silicone directly. Inflammatory reactions associated with silicone hydrogel contact lens wear are not caused by an allergic reaction to silicone alone. Antigens found on lenses could be due to tear film deposits, microbial contamination, or components of care systems.
The authors concluded that ‘Silicone cannot elicit a response from the immune system … Clinicians do a disservice to their profession, their scientific training, their patients, and to industry by invoking the phrase ‘silicone allergy’ as the explanation for problems their patients might encounter with silicone hydrogel lenses.’19
Parameters
Limited parameters are no longer an obstacle in the daily disposable SiHy market. More fitting options, and a broad range in spheres, torics, and multifocals exist, allowing practitioners to fit a wider range of patient needs. Each year, it seems more and more manufacturers are coming out with extended parameters, which has significantly helped practitioners meet the needs of their patients.
The Silicone Hydrogel Market
A vast majority (76%) of soft fits in the UK in 2018 were silicone hydrogel, presumably due to the superior oxygen performance benefits. However, adoption of SiHy is still lagging in the daily disposable modality (63% of total).1 Use of SiHy in specialty daily lenses (torics and multifocals) lags even further behind planned replacement modality fits, according to industry reports.1
How To Meet Patient Demands
The demands of the modern patient are perhaps the best argument for making the switch to a one-day SiHy contact lens. As patients increase their daily wearing time, a hydrogel one-day contact lens may become a concern. Think about how many hours your typical contact lens patient is wearing his or her lenses. Many patients are wearing their lenses for 14 hours or more. Patients have busy lifestyles that often require the maximum breathability and corneal health maintained by a one-day silicone hydrogel contact lens.
Consumers are also on a quest for healthier lifestyle choices. Health and wellness are becoming more and more important to people across the world. Take, for example, the organic food industry. Consumer demand for foods without preservatives and chemicals has become increasingly popular throughout the past decade. There are many documentaries, advertisements, and books all pushing the importance of prevention and well-being in cosmetics, beauty, food, and drink. Daily disposable silicone hydrogel use is aligned with that interest because daily lenses maintain a healthy ocular surface that could be even healthier than non-daily lens counterparts.
What is the relevance of oxygen to contemporary contact lens practice? A review of the literature was conducted,10 and results indicate that oxygen is required for a number of processes that occur in the normal, healthy eye to ensure ideal function. These processes could potentially be affected by the presence of a contact lens. Evidence from laboratory, clinical, and modelling studies indicates that normal oxygenation depends on the physiological system under consideration, corneal location, and the state of eye closure. This diversity is reflected in the wide range of minimum lens Dk/t requirements that are present in the literature. As a result of these findings, the authors suggest that ‘… it does not seem unreasonable for a clinician to attempt to satisfy the highest [oxygen criterion] that available lens technology will permit. This pragmatic approach has considerable appeal, particularly when, as is increasingly the case, access to suitable materials and lens designs can be had.’21
Conclusion
More oxygen to the eye is a good thing and is essential to eye health. We’ve seen a huge reduction in oxygen-related problems as new and improved lens designs and materials have been unveiled in recent years, and we continue to see improvements in contact lens technology. Most practitioners have made the switch to silicone hydrogel in monthly and two-week lens modalities, so why not embrace those advantages for one-day contact lens patients as well? The evidence strongly supports offering silicone hydrogels to all new and existing patients, regardless of modality.10,22 Even if patients do not opt for a silicone hydrogel daily lens, it could still be presented as a new option, especially if they are having issues with their current lenses.
Knowledge is power. Educating patients about new contact lens options will help keep them interested in the latest innovations in contact lens design and materials. Educating patients about their eye health and how certain contact lenses can benefit their eyes is usually all it takes for patients to make a change. Patients look to you – their eye care professional and an expert in the field – to help them make the best contact lens decisions based on their prescription, eye health, and lifestyle needs.
Dr Casey Hogan and Dr Stephanie Woo are optometrists based in the US. Thanks to Neil Retallic for adapting for the UK.
REFERENCES
- Morgan PB et al. International contact lens prescribing in 2018. Contact Lens Spectrum, 2019: 34(1):26-32
- Holden BA, Mertz GW. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthalmol Vis Sci. 1984;25:1161-1167.
- Fonn D, Sweeney D. The benefits of silicone hydrogel daily disposable lenses. Contact Lens Spectrum. 2015;30:42-45.
- Polse KA, Sarver MD, Harris MG. Corneal edema and vertical striae accompanying the wearing of hydrogel lenses. Am J Optom Physiol Opt. 1975;52(3): 185-191.
- Dumbleton KA, Richter D, Woods CA, Aakre BM, Plowright A, Morgan PB, et al. A multi-country assessment of compliance with daily disposable contact lens wear. Cont Lens Anterior Eye. 2013;36(6):304-312.
- Holden B, Stretton S, Lazon de la Jara P, Ehrmann K, LaHood D. The future of contact lenses: Dk really matters. Contact Lens Spectrum. 2006. Available at: https://bit.ly/2yj4aO3; last accessed June 18, 2018.
- Brennan N, Morgan P. Clinical highs and lows of Dk/t. Part 1 – Has oxygen run out of puff? Optician. 2009;238(6209):16-20
- Morgan PB, Brennan NA, Maldonado-Codina C, Quhill W, Rahshid K, Efron N. Central and peripheral oxygen transmissibility thresholds to avoid corneal swelling during open eye contact lens wear. J Biomed Mater Res. 2010;92(2):361-365.
- Brennan NA, Morgan PB. Reader’s Forum: Another view of oxygen transmission. Contact Lens Spectrum. 2005. Available at: https://bit. ly/2M3owNh; last accessed June 18, 2018.
- Covey M, Sweeney DF, Terry R, Sankaridurg PR, Holden BA. Hypoxic effects on the anterior eye of high-Dk soft contact lens wearers are negligible. Optom Vis Sci. 2001;78(2):95-99.
- Sweeney DF. Have silicone hydrogel lenses eliminated hypoxia? Eye Contact Lens. 2013;39(1):53-60.
- Morgan PB, Chamberlain P, Moody K, Maldonado-Codina C. Ocular physiology and comfort in neophyte subjects fitted with daily dis- posable silicone hydrogel contact lenses. Cont Lens Anterior Eye. 2012;36(3):118-125.
- Kinoshita BT, Chalmers RL, Mitchell GL, Richdale K, Lam DY, Sorbara L, et al. Rate of change and predictive factors for increasing minus contact lens powers in young myopes. Clin Exp Optom. 2015;98(4):323-329.
- Diec J, Tilia D, Thomas V. Comparison of silicone hydrogel and hydrogel daily disposable contact lenses. Eye Contact Lens. E-pub ahead of print, Jan. 17, 2017.
- Dillehay SM, Miller MB. Performance of lotrafilcon b silicone hydrogel contact lenses in experienced low-Dk/t daily lens wearers. Eye Contact Lens. 2007;33(6):272-277.
- Dumbleton K, Kier N, Moezzi A, Feng Y, Jones L, Fonn D. Objective and subjective responses in patients refitted to daily-wear silicone hydrogel contact lenses. Optom Vis Sci. 2006;83(10):758-768.
- Riley C, Young G, Chalmers R. Prevalence of ocular surface symptoms, signs, and uncomfortable hours of wear in contact lens wearers: the effect of refitting with daily wear silicone hydrogel lenses (senofilcon A). Eye Contact Lens. 2006;32(6):281-286.
- Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):93-99.
- Data on file. CooperVision patient survey 2015.
- Hall BJ, Jones LW, Dixon B. Silicone allergies and the eye: fact or fiction?
- Eye Contact Lens. 2014;40: 51-57.
- Papas EB. The significance of oxygen during contact lens wear. Contact Lens Anterior Eye. 2014;37(6):394-404.
