The paediatric and low vision clinics in the hospital eye service commonly encounter children and teenagers with features of cerebral visual impairment (CVI). This is not surprising, given that CVI is now the leading cause of severe sight impairment (SSI) in children in England and Wales.1 Identification and characterisation of this condition have been discussed in the first two articles in this series (see Optician 22.03.19 and 10.05.19). This third article presents some practical examples of how suspected CVI can be managed in the clinic setting.
Visual Pathways
An understanding of the affected visual pathways is important to put the case scenarios into context. These are as follows:
- Primary visual pathway. This extends from the retina to the visual cortex. Field defects resulting from damage to this pathway correspond directly with location of lesion. There is no associated inattention with damage here.
- Visual cortex. Analysis of visual fields, contrast, colour, detail (acuity) and movements help locate damage to this region.
- Dorsal stream. Situated in the parietal lobe, this represents the mapping system of the ‘here-and-now’.
- Ventral stream. Situated in the occipital lobe, this can be described as our library of recognition and holds neural representation of such targets as faces, places and objects.
The tree diagram in figure 1 summarises these pathways along with the visual functions they are related to. The diagram should serve as a useful visual aid when different scenarios are discussed.
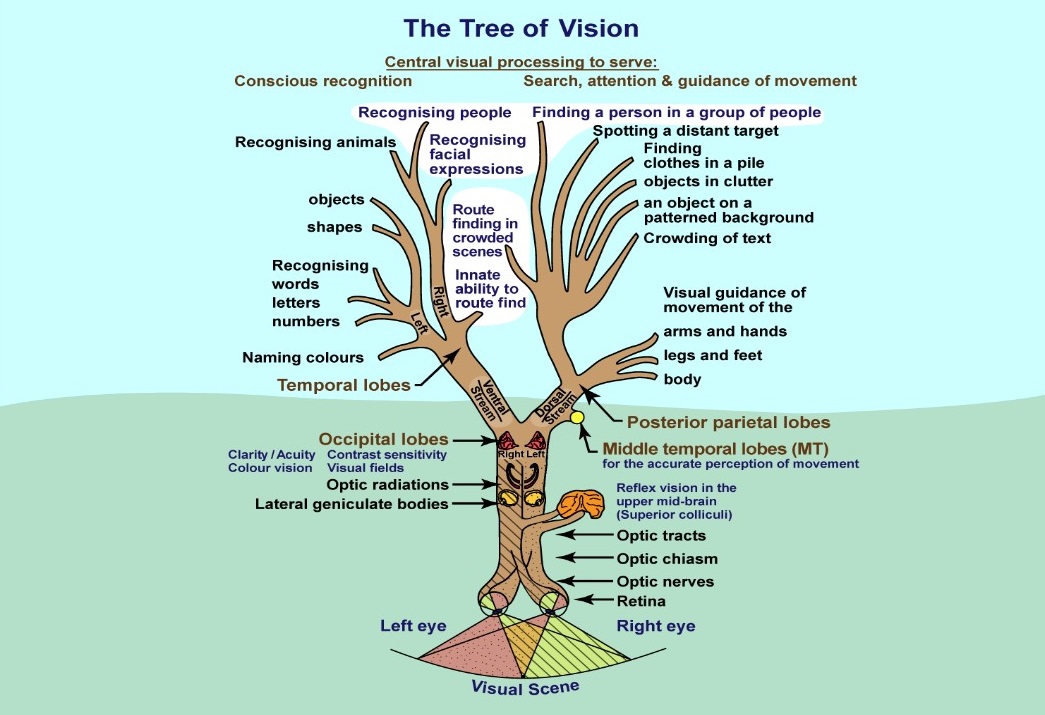
Figure 1: The tree of vision2
CVI often requires a multidisciplinary approach. In some clinics, paediatricians carry out functional vision assessment and consider the recorded visual impairment within the context of the child’s general health and development. This is important as CVI is often associated with other health issues, such as cerebral palsy, hydrocephalus and periventricular white matter injury.3 Dorsal stream dysfunction has also been associated with autism spectrum disorder (ASD)4-6 and dyslexia.7 Due to the complex nature of CVI and associated conditions, it is essential that a diagnosis is made by an experienced and suitably specialised clinician. Typically, this is a specialist paediatrician or ophthalmologist who can assess these patients in a dedicated functional vision clinic. Orthoptists, visiting teachers for the visually impaired (VTVIs) and optometrists can further contribute to the management of CVI. The optometrist’s role is as yet not clearly defined. In this article, the author describes her personal experience in dealing with CVI cases within the hospital eye service. All the scenarios are based on real-life encounters.
Scenario 1: Identifying possible CVI
This scenario serves as an example of the challenges in identifying CVI during a routine eye test.
Children who fail the pre-school vision screening test may be referred to a community optometrist or to the local eye hospital for further assessment. This usually includes a binocular vision assessment, followed by retinoscopy and ophthalmoscopy. Conditions such as amblyopia and strabismus, as well as
refractive error and ocular pathology, are identified and treated. Sometimes, the findings of the assessment cannot be fully explained by these conditions. The author has found that asking a few simple questions about the child’s behavioural features can highlight the need for further assessment in a functional vision clinic.
Consider the situation where a child fails the pre-school vision screening test with a logMAR vision of 0.28 in either eye. Initial findings include:
- General health and birth history are unremarkable
- There is a family history of strabismus and amblyopia
- The parents have noticed an eye-turn and wonder if this explains their child’s ‘clumsiness’
Further questioning reveals that the child has been finding it difficult to concentrate and stay on task for longer than 10 minutes. Objects that are pointed out in the distance are not identified, even if quite large. When the child is asked to find a specific toy in a toy box, the child cannot see it even if it is right in front of them.
All the other boys and girls in the preschool group are able to write their names, but this child struggles to copy any shapes, let alone write numbers, letters or their name. The parents also report that the child has no sense of traffic safety and runs right in front of cars and bikes.
These behavioural traits are in keeping with dorsal stream dysfunction, commonly seen in CVI.
Further clinical assessment is as follows:
- Cover test reveals exotropia without fusion or stereopsis
- Ocular motility is grossly full
- Cycloplegic refraction reveals minimal hypermetropia (not accounting for reduced vision)
- Ocular health is normal
Strabismus, and especially exotropia, is a common feature in CVI.8 Furthermore, Kheptal and Donahue state that patients with better initial visual acuity tend to show more improvement in visual function.9
Sometimes, there is no clear signpost as to why a child may have developed features suggestive of CVI. These might include low birth weight or a history of pre-term birth. However, this does not exclude the possibility of CVI and it is still prudent to seek further advice when CVI is suspected.
The child should be referred to an ophthalmologist for onward referral to a paediatrician who then carries out functional assessments to confirm diagnosis. The optometrist’s responsibility in this case has been to identify patients for further investigation. The paediatrician’s role is to tease out differential diagnoses, as some traits that are seen in CVI may be attributable to other developmental issues.
Scenario 2: Prioritising support
This scenario is based upon a child with complex needs that have been only partially addressed. What can optometrists contribute if a child with complex needs seeks their advice?
Children with complex needs are often referred to the HES after failing the pre-school vision screening test. This can be due to poor vision or due to limited ability to cooperate with the tests on offer.
Let us assume this child’s vision is measured to be 6/12 with both eyes open. Sometimes it is not possible to test each eye
separately as a child may object to occlusion. If a child objects to occlusion of just one eye, this strongly suggests that the vision is likely to be poorer in the unoccluded eye.
The Hirschberg test is a gross assessment of strabismus undertaken by observing the symmetry of the corneal reflexes. It is useful when the cover test cannot be performed. Motility and convergence can be assessed directly or, grossly, through observation during the consultation.
Cycloplegic or Mohindra refraction should always be attempted (figure 2). This can be done with or without a trial frame. If lenses are not tolerated in front of the eye, the brightness and direction of the retinoscopy reflex can give some indication of the approximate prescription.
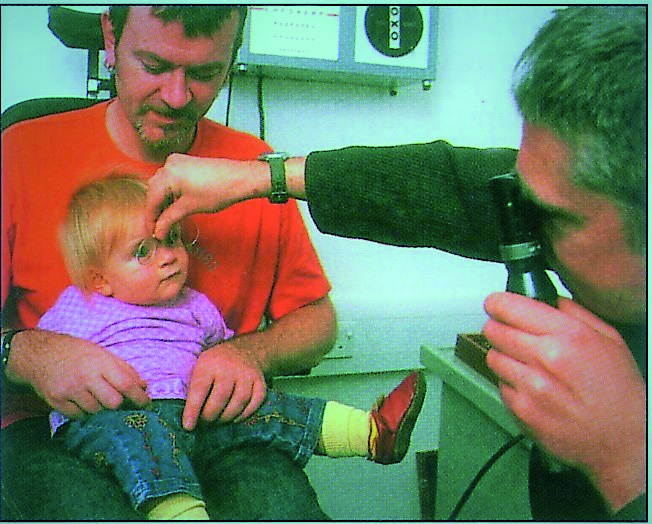
Figure 2: Cycloplegic or Mohindra refraction should always be attempted
Ophthalmoscopy should always be attempted to assess ocular health. Let us assume that this child’s eyes are healthy, with symmetrical corneal reflexes and no significant refractive error. However, the vision is reduced and a child with complex needs has an increased risk of CVI.3 It is prudent to ask a few questions to put this case into context:
- What condition(s) have been diagnosed to date?
- Does the family have any concerns?
- What has been explained about the child’s condition(s) so far?
- Were birth and pregnancy normal?
In the author’s experience, if the optometrist asks parents if they are worried about the child’s vision, the parents often say ‘no’. If, on the other hand, the parents are asked if they have any concerns about the child’s general functioning and behaviour, more information is elicited. Behavioural features are often ascribed to the existing diagnoses, typically conditions such as autism or Down’s syndrome. Parents often do not link the features, typical of dorsal stream dysfunction, with sight impairment. It is common for these features or compensation strategies not to be adequately discussed with the patient and, therefore, the child cannot reach maximum potential.
- Behavioural features to identify and discuss include where the child is:
- Overwhelmed with sensory overload (smells, sounds, touch, visual)
- Bumping into things on either or both sides
- Tripping over things, walking into things, especially low furniture
- Has reduced sense of spatial awareness
- Either running around aimlessly or refusing to walk
- Objecting to cross-bar being removed from buggy
- Demonstrates worsening behaviour or increased anxiety in crowded places, such as a supermarket
- Not tolerating bright lights
Children with complex needs may display features that are similar to the ones displayed in CVI. So, it is worth asking the following:
- Are the features attributable to the known diagnoses?
- Might there be additional CVI?
Rather than focusing on the diagnosis (which may only complicate matters further), the optometrist may offer some coping strategies and interventions to manage the behavioural features. For example, advice can be given to declutter the home environment to ensure that the child does not have to cope with information overload. A systematic approach to toy storage can be discussed. In cases of suspected lower field inattention, it might be helpful advise the carer to store toys above the child’s waist level and to remove low standing furniture.
In order to encourage physical exercise and mobility, the use of a walker might be considered. The crossbar on a buggy can often provide a sense of security. In the same way, a walker can provide a sense of security, especially in more crowded places where the child potentially gets frightened by people and objects suddenly appearing in front of him or her. A walker also allows a child to feel the ground ahead of them (offering tactile guidance), which is especially helpful for children with lower field impairments.
Some children also benefit from ear defenders in crowded places to reduce the sensory overload. The use of a sensory tent can be discussed (figure 3). This is simply a tent with only one single toy inside it. It is commonly recommended to children with autism or CVI.

Figure 3: Sensory tent
Scenario 3: Management options
This scenario serves as an example of how visual impairment may be characterised and managed in a patient who has been formally diagnosed with CVI.
As CVI is now the leading cause of SSI in childhood, it becomes more common for a low vision practitioner to encounter children and young adults with this condition. Poor eyesight and
perceptual difficulties impact on social interaction, access to information and mobility.10 This scenario will illustrate these different aspects and show some possible interventions.
A 16-year-old child attends the low vision clinic with a diagnosis of CVI having been made in early childhood. With normal intelligence and good parental support, the child attends mainstream school. The visiting teachers for the visually impaired (VTVIs) have introduced a number of adaptations, such as enlarged textbooks and talking scales for science class. In class, an iPad is used to view everything in large font.
As this child progresses through school, their visual demand increases with smaller text size requirement increasing and a greater number of different reading tasks. Vision can be variable, depending on fatigue and stress levels. It becomes more difficult for the child to keep up with the teaching within the classroom and also with homework tasks. Accessing material with a very slow reading speed or through optical character recognition speech technology can cause a child to lag behind.
For some children with reading difficulties due to CVI, it is worth considering learning Braille and this can be mentioned to the VTVI. Herzberg et al report that motivation is key to success.11 The availability of Braille teachers can be limited, which is why Wagh et al are introducing a self-learning Braille kit.12 Animations shown in the classroom to illustrate the lesson content may be inaccessible due to dorsal stream dysfunction or poor vision or contrast. Furthermore, not all teachers understand the visual problem unless this has been clearly explained to them in understandable language. For this reason, a comprehensive report, with an explanation of the visual impairment and recommendations about adaptations, is extremely important. The child can take this report to the relevant teachers.
It can be very difficult for a child with simultanagnosia or severe visual field impairments to spot friends in a busy classroom or on the school grounds. Even when standing with a group of friends, the child may not see people who are right beside him or her. The fast-moving changes of facial expressions are not seen in dyskinetopsia or with impaired vision or contrast sensitivity, which makes it difficult to gauge the mood of the person talking to the child.
Team sports also become more challenging as balls move faster and games become more complex. Dyskinetopsia can lead to a ball not being seen until it slows down and hits the face without time to catch it. With simultanagnosia, only single elements of a scene are seen but the elements cannot be combined to build a complete picture of a scene. Visual field impairments are common in CVI, especially lower field defects 10 and this can lead to the ground not being seen or team mates and balls not being seen. Class mates may not understand the visual challenges and may make a child out for being clumsy. They may start shunning this child which then leads to social exclusion.
Social inclusion of pupils with a visual impairment in high school can be enhanced through building on strengths, developing relationships with peers and fully accessing the curriculum alongside peers.13 Social inclusion can be encouraged in various ways. Goalball UK offers sessions in schools of children with a visual impairment, whereby the whole class joins in with this ballgame wearing blind folds. The use of balls with bells and explaining the particular difficulties to school staff and classmates can make a real difference. For children with an interest in sports, a disability sports coordinator or Goalball UK can point to local sports clubs for people with a VI. Some patients may even make it to the Paralympics.
Peer support from other visually impaired children can further help to build confidence and a sense of belonging. It is worth checking your local area. For example, in some areas, the RNIB runs after-school or other clubs for visually impaired youngsters. Another source of support and information is Haggeye, a forum for children and young people with a VI.
CVI can also be associated with difficulties in wayfinding. This can become more problematic when a child moves on to become more independent. Moving around within the school grounds can be a challenge and can lead to stress and delays in getting to lectures. A child may not be able to go to school independently and the prospect of transition into adulthood can be daunting. Relying on others and the use of a cane or guide-dog are common strategies for young people with a sight impairment living in a city. The use of a hiking pole is another aid to feel the ground ahead. It is common for children with CVI to bump into obstacles and to become agitated in crowded places, such as busy traffic and shopping malls. This is a feature of dorsal stream dysfunction.10 Independence in mobility can have a positive impact on mental health.
Preparations need to be made for transition to university, college, work or independent living and the right support needs to be in place to make this transition smooth. The specific needs have to be understood and addressed.14 Familiarising oneself with local referral pathways and available support can be extremely helpful. The RNIB and My Guide can offer good advice. The ‘Children, Young People and Families (CYPF) Transition’ team and ‘Identify, React, Intervene and offer Sustained Support’ (IRISS) service are useful contacts.
Smartphones and tablets are tremendously useful, with many apps that are specifically designed to help the visually impaired user (figure 4). For example, apps can assist in accessing written material and in wayfinding. One can never assume that a young person is making full use of the available apps and it is worth finding out what support is available in your local area.

Figure 4: Smartphones and tablets are useful
Conclusion
This article has aimed to show that children with suspected or diagnosed CVI are managed in different ways, depending on the situation in which they present, the unique features of their CVIs and the specific needs for each individual. Sometimes our initial role may be to identify children for further investigation. Sometimes our role may be to offer strategies and interventions. The presented scenarios are a snapshot of the author’s emerging experience in managing this condition and are not intended as a strict guideline to follow.
Cirta Tooth is a hospital optometrist based in Edinburgh with a special interest is low vision and functional vision.
Acknowledgement
Tree diagram was reproduced with kind permission from Professor Gordon Dutton.
References
- Mitry, Danny; Bunce, Catey; Wormald, Richard; et al. 2013. Childhood visual impairment in England: a rising trend. Archive of Diseases in Childhood 98(5)
- Lueck, Amanda H.; Dutton, Gordon N. (Eds.) (2015). Vision and the Brain: Understanding Cerebral Visual Impairment in Children. New York: AFB Press.
- Gorrie, F. et al. 2019. Towards population screening for cerebral visual impairment: validity of the five questions and the CVI questionnaire. Plos One 14(3), Article Number e0214290.
- Manning et al. 2013. Processing slow and fast motion in children with autism spectrum conditions. Autism Research 6(6), pp. 531-541
- Greimel, E. et al. 2013. The temporal dynamics of coherent motion processing in autism spectrum disorder: evidence for a deficit in the dorsal pathway. Behavioural Brain Research 251, Special issue, pp. 168-175
- Spencer, J. et al. 2000. Motion processing in autism: evidence for a dorsal stream deficiency. Neuroreport 11(12), pp. 2765-2767
- Pellicano, E. and Gibson, L.Y. 2008. Investigating the functional integrityof the dorsal visual path-way in autism and dyslexia. Neuropsychologica 46(10), pp. 2593-2596
- Baeteman, C. et al. 2008. Primary exotropia: importance of cerebral MRI. Journal Francais d’Ophthalmologie 31(3), pp. 287-294
- Kheptal, Vijay; Donahue, S.P. 2007. Cortical Visual Impairment: Etiology, associated findings, and prognosis in a tertiary care setting. Journal of American Association of pediatric Ophthalmology and Strabismus 11(3), pp. 235-239
- Zihl, J. and Dutton, G.N. 2015. Cerebral visual impairment in children. 1st ed. Wien. Springer-Verlag
- Herzberg, T.S. et al. 2017. Teachers’ experiences with literacy instruction for dual-media students who use print and Braille. Journal of Visual Impairment & Blindness 111(1), pp. 49-59
- Wagh, P. et al. 2016. E-Braille: a self-learning Braille device. Conference: 22nd National Conference on Communications (NCC). Location: Guwahati, INDIA
- Jessup, G. et al. 2017. The social experiences of High School students with visual impairments. Journal of Visual Impairment and Blindness 111(1), pp. 5-19
- Van Schalkwyk, G.I. and Volkmar, F.R. 2017. Autism spectrum disorders challenges and opportuni-ties for transition to adulthood. Child and Adolescent Psychiatric Clinics of North America 26(2), p. 329
