Motor fusion in a binocularly normal subject maintains the alignment of the visual axes giving bifoveal fixation of the object of regard even if it moves, thereby allowing for sensory fusion and stereopsis. The failure or absence of motor fusion may be obvious when the patient reports diplopia*, or to the naked eye when there is a large misalignment present (heterotropia)**, but apparent alignment of the eyes in an asymptomatic individual in no way ensures true alignment or fusion.
There may be a misalignment that is too small to see (even by close observation of the corneal reflexes), and small eso or hypo/hyper deviations are easily capable of disrupting motor fusion to the point of breaking down to a tropia, with the accompanying failure of sensory fusion. The expected diplopia may be absent due to markedly reduced vision or suppression in one eye.
Even if alignment is true, fusion is not guaranteed, as alignment could be incidental. For example, significant anisometropia (developing idiopathically in childhood, or as a result of monocular keratoconus or cataract surgery) in an orthophoric patient will disrupt sensory fusion due to the dissimilarity of the two retinal images (one clear and one blurred/distorted) and subsequently motor fusion will also fail.
Alternatively, successful cosmetic squint surgery may result in good alignment of the visual axes but without restoration of sensory fusion, for example if the tropia was congenital with no history of binocular experience (hence no potential for restoration of sensory fusion or true binocular vision), or if there is significant amblyopia. If the presence of motor fusion is not always immediately apparent, evidence for it must be sought by appropriate investigations.
One core tool in the demonstration of the presence or absence of motor fusion is the cover test. This generic term includes three different variations on a theme: the cover/uncover test, the alternating cover test and the prism cover test. Each has its own individual features and applications and each needs to be clearly understood. All have the advantage that they are objective tests, the only requirement from the patient being enough compliance to fixate a target of interest. All necessary information to come to a correct diagnosis is available through practitioner observation and interpretation.
Therefore, it is as effective in children as it is in adults. Each can be performed at any chosen fixation distance, and in the clinical setting typically distance (at 6m) and near (typically at 30-40cm) are considered a bare minimum. In some cases, involving distance vision problems, 6m is too close, so it can be repeated with a ‘far distance’ target, such as something out the window, across the street. It should be repeated for any specific tasks performed by the patient at a closer distance than the typical reading position. It should also be considered for intermediate tasks, for example computer work, if the distance and near results are not both satisfactory (if both are satisfactory, then positions in between are likely to also be satisfactory). The practitioner must also consider whether it should be done with or without refractive correction in place, or indeed repeated for both situations. Although easy to perform, the cover test can also be catastrophically error strewn: good technique is essential. Table 1 lists some of the common errors that can creep into poor technique, some potential consequences and clinical implications, and some suggested remedies.
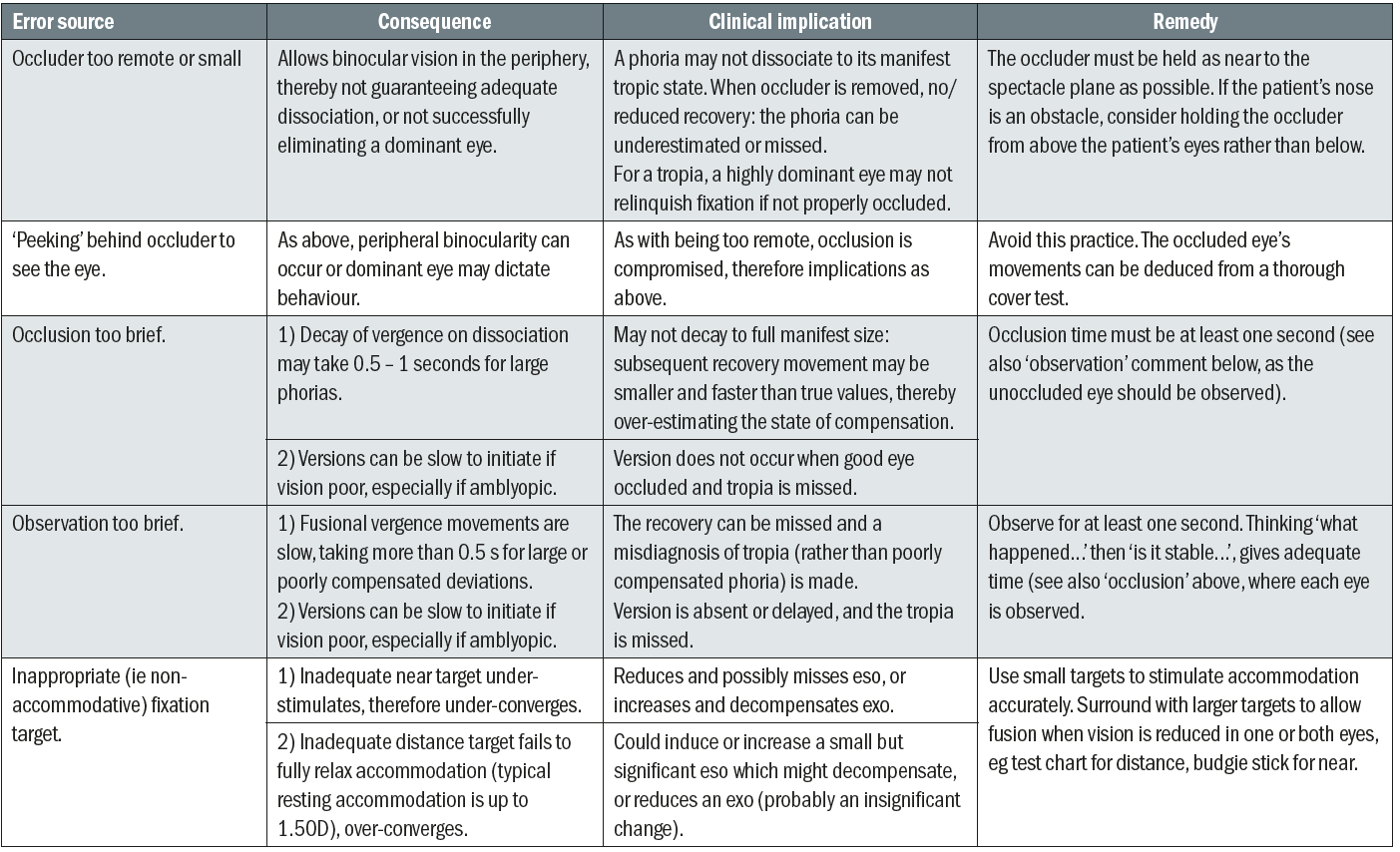
Table 1: Common errors in performing cover test and their potential implications
Performance and interpretation of tests
The three commonly used variations of the cover test are:
- Cover/uncover test (CT)
- Alternating cover test (ACT)
- Prism cover test (PCT)
All three variations of the cover test involve the insertion of an occluder over one eye, followed by either removal of the occluder or swapping the occluder over to the other eye. Care must be taken to ensure full occlusion (see table 1). All movements of the occluder should be rapid, followed by a significant pause, long enough for any subsequent eye movement to be fully completed by the patient and for the practitioner to interpret what eye movement occurred and if the outcome is stable. This pair of observations typically takes at least one full second of occlusion / observation, and shortening this time is a common source of error. Longer periods of occlusion, five seconds or more, to establish stability of the size of a deviation may also be required (see table 6, the alternating cover test).
Insertion of the occluder causes dissociation by eliminating the retinal image from the occluded eye, hence only allowing the brain access to one image from the unoccluded eye. The patient cannot have simultaneous perception of both retinal images, therefore flat fusion (which is the fusing together of both retinal images with the ultimate aim of stereopsis) is impossible and in turn motor fusion will also be impossible. Therefore, while occluded, any latent deviation (heterophoria) will become manifest (heterotropia) and hence the two will become indistinguishable. This will remain the case as long as the occluder is present, whether held in front of one eye or alternating between the two. On removal of the occluder the potential for simultaneous perception is restored and motor fusion should overcome any misalignment of the eye behind the occluder, thereby also restoring sensory fusion. The practitioner must judge if this is the case.
Observation of eye movements.
Throughout the cover test, on each move of the occluder the practitioner looks for any eye movements and if seen, the practitioner must evaluate the type, direction, size and speed of the movements in order to come to a meaningful interpretation. The eye movements observed may be versions or vergences. Version eye movements are where the eyes move as a pair with the alignment of the visual axes remaining unchanged, in order to fixate a target. These are the movements we typically make to view different parts of a visual scene at a constant depth, eg viewing a painting or reading lines of text. If the visual axes were initially aligned, they remain aligned. But if there was a misalignment then this misalignment persists. The maintenance of such a misalignment demonstrates that the patient has a heterotropia, with motor fusion failing to occur. These version movements are rapid eye movements, typically being completed within a fraction of a second if the vision is good in the fixing eye. Their speed makes them relatively easy to see, even when small. However, if vision is poor and amblyopia is present, these movements may be slower to initiate and less stable in their end-point for the weaker eye. Enough observation time must be given in order to appreciate this.
Vergence eye movements involve a change in the alignment of the visual axes with respect to each other. They exist to allow us to shift our gaze to objects at different distances from us, requiring convergence of the visual axes for a near object, and divergence for shifting towards a more remote object. Vergence movements should not occur if we are maintaining fixation at a constant distance, hence we would not expect to see them while performing the cover test. However, we often do see a vergence movement on removal of the occluder when performing the cover/uncover test. Observation of a vergence movement on removal of the occluder is explained by the patient needing to re-adjust the direction of the visual axis of the just-unoccluded eye in order to direct it back to the fixation target, in order to eliminate the diplopia caused by the misalignment that became manifest by the dissociating occluder. The observation of this recovery movement is key in confirming the presence of motor fusion and is diagnostic of heterophoria.
A summary of the movements associated with movement of the occluder is given in table 2. From this table it can be seen that sometimes a single observation on a single move of the occluder can be diagnostic, for example a tropic eye taking up fixation on insertion of the occluder to the fellow eye, or the removal of the occluder in a heterophoric subject. However, this is not always the case, for example insertion of the occluder will not reveal a phoria or a tropia of the occluded eye. In order to ensure a correct diagnosis in all cases, a strict protocol of insertions and removals needs to be followed.
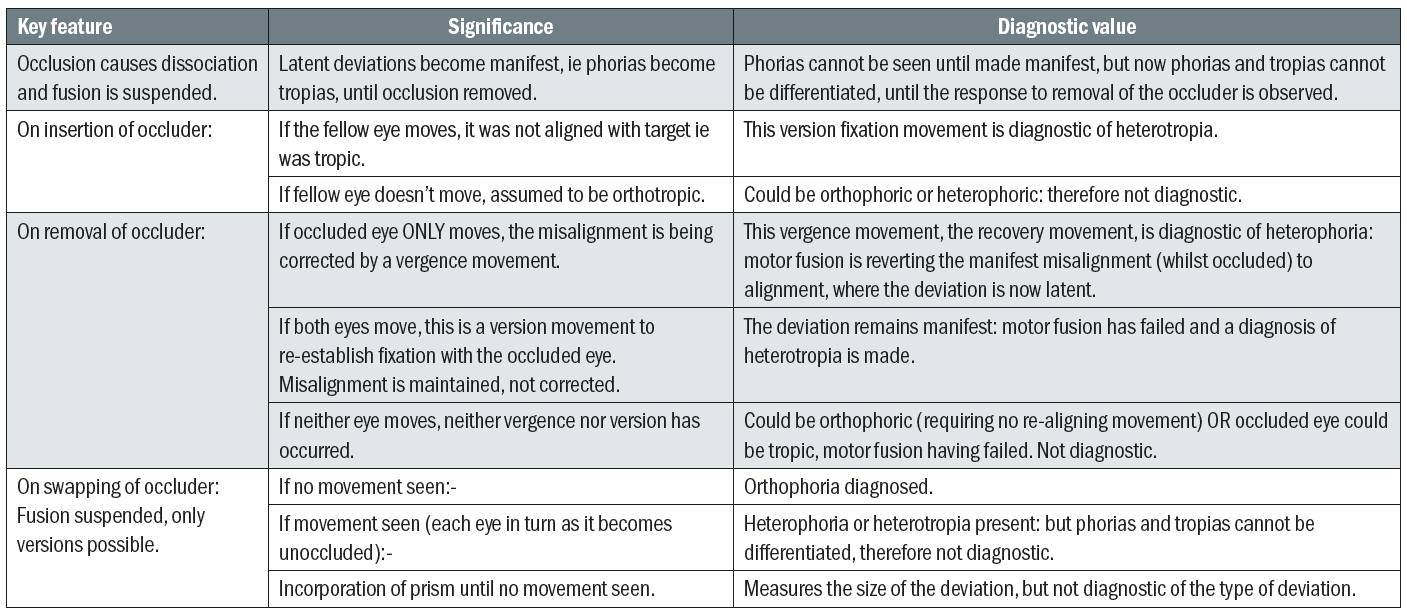
Table 2: Key observations during cover test performance and their clinical interpretation. Note that no single action / observation is adequate in diagnosing all potential outcomes (orthophoric, heterophoric or heterotropic)
Table 3 outlines a typical administration of the cover/uncover test in an orthophoric patient. In this patient, the lack of any movement at any point confirms the absence of any misalignment, either phoria or tropia.
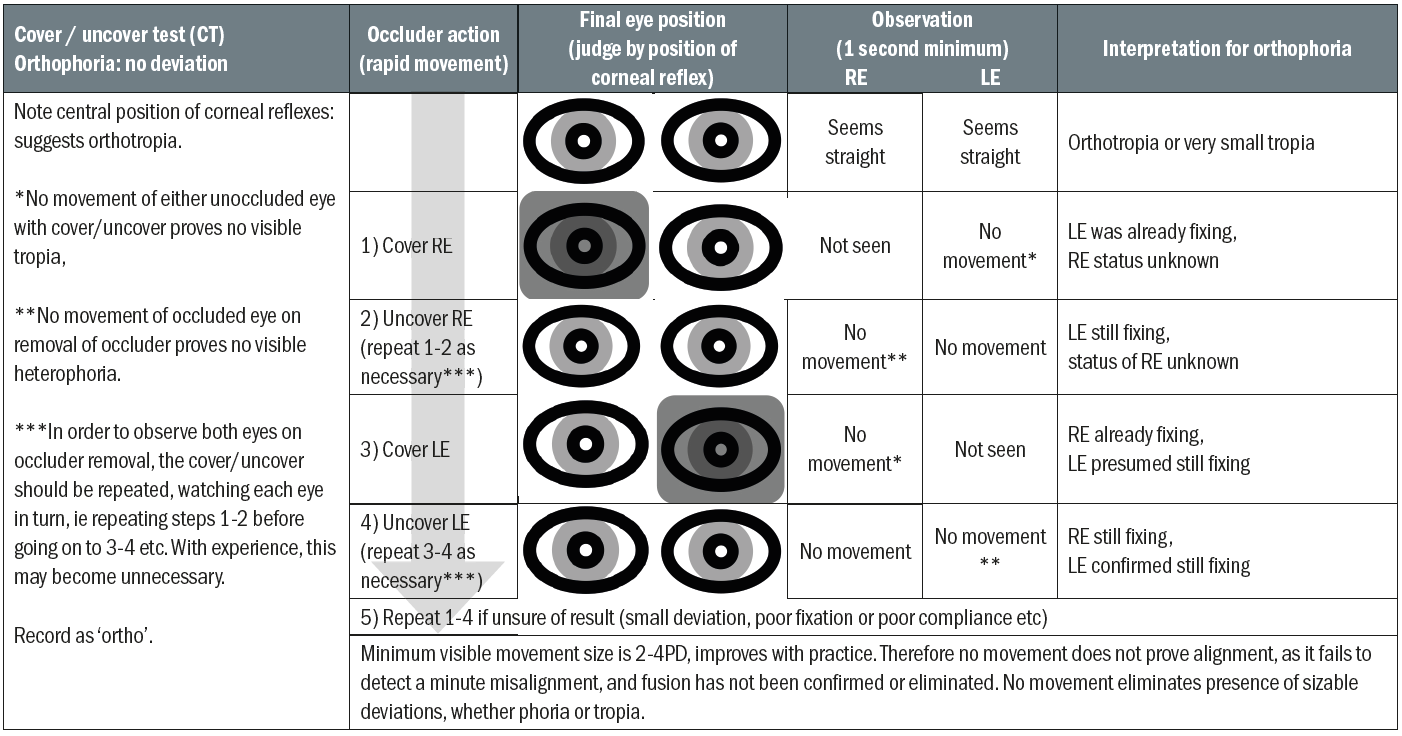
Table 3: Step by step analysis of cover/uncover test in orthophoria. Note no movement at any stage
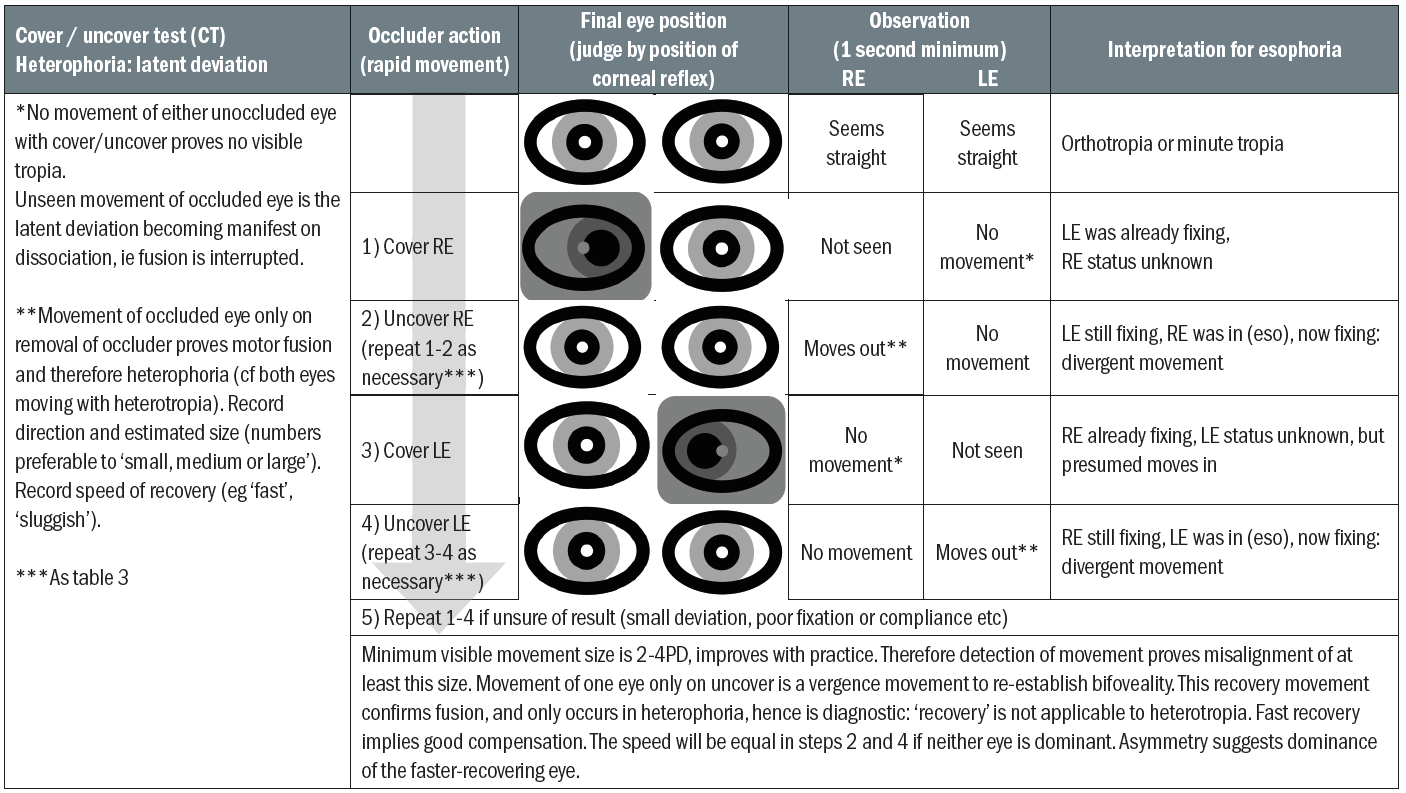
Table 4: Step by step analysis of cover/uncover test in esophoria. Note divergence movement on removal only
Tables 4, 5 and 6 illustrate the results seen using the same protocol for esophoric, right esoptropic and alternating esotropic patients respectively. It can clearly be seen that a diagnosis is not always possible in these cases without following through this sequence of cover/uncovers, but that with the complete sequence, all have demonstrated a unique pattern of movements that allows for correct differentiation between these three types of eso-deviations. (The process is exactly the same for exo or hyper/hypo deviations, it is only the direction of eye movements that change. These patterns can easily be sketched out by the reader.)
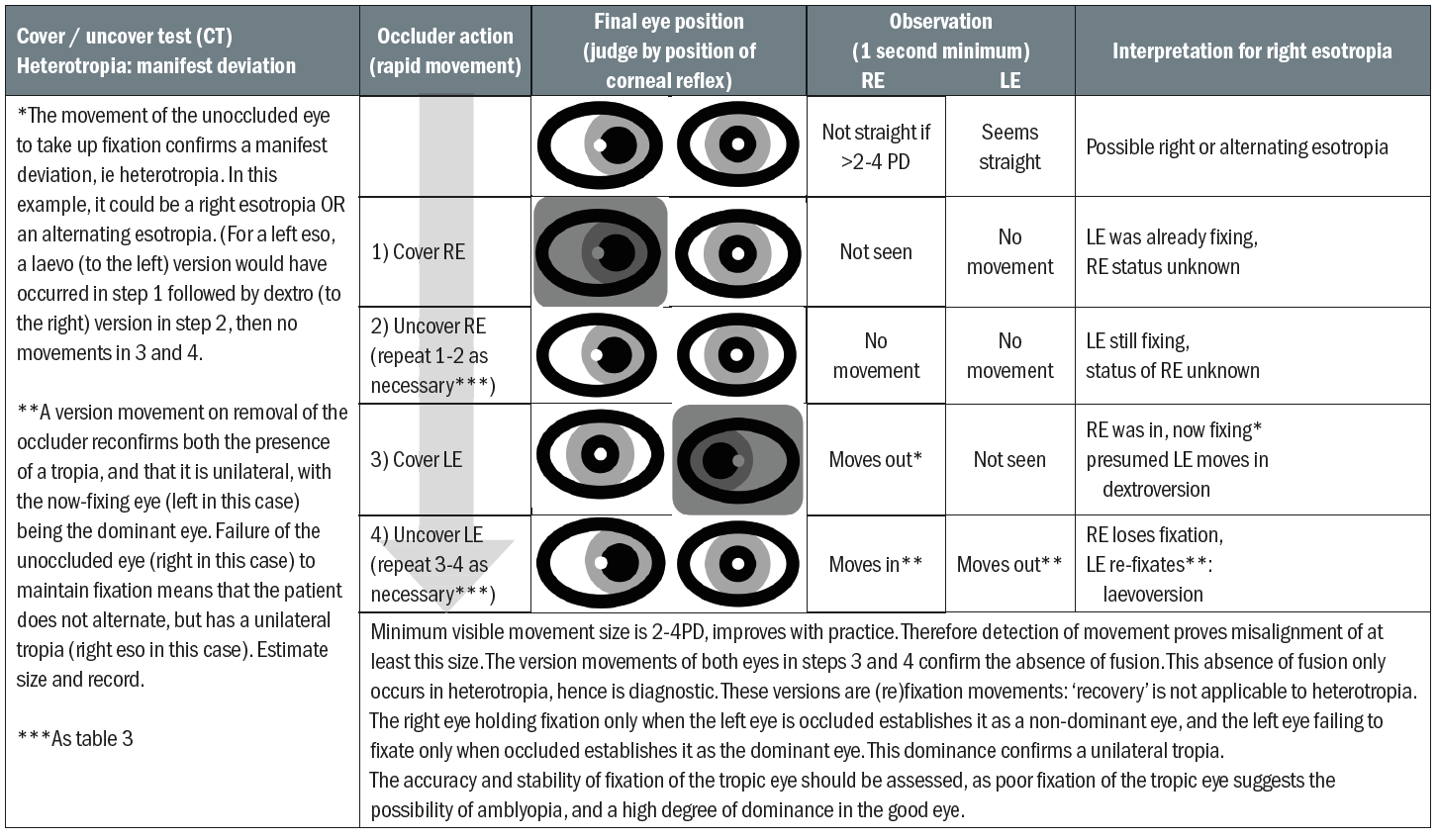
Table 5: Step by step analysis of cover/uncover test in right esotropia. Note version movements on selected insertion and removal of occluder
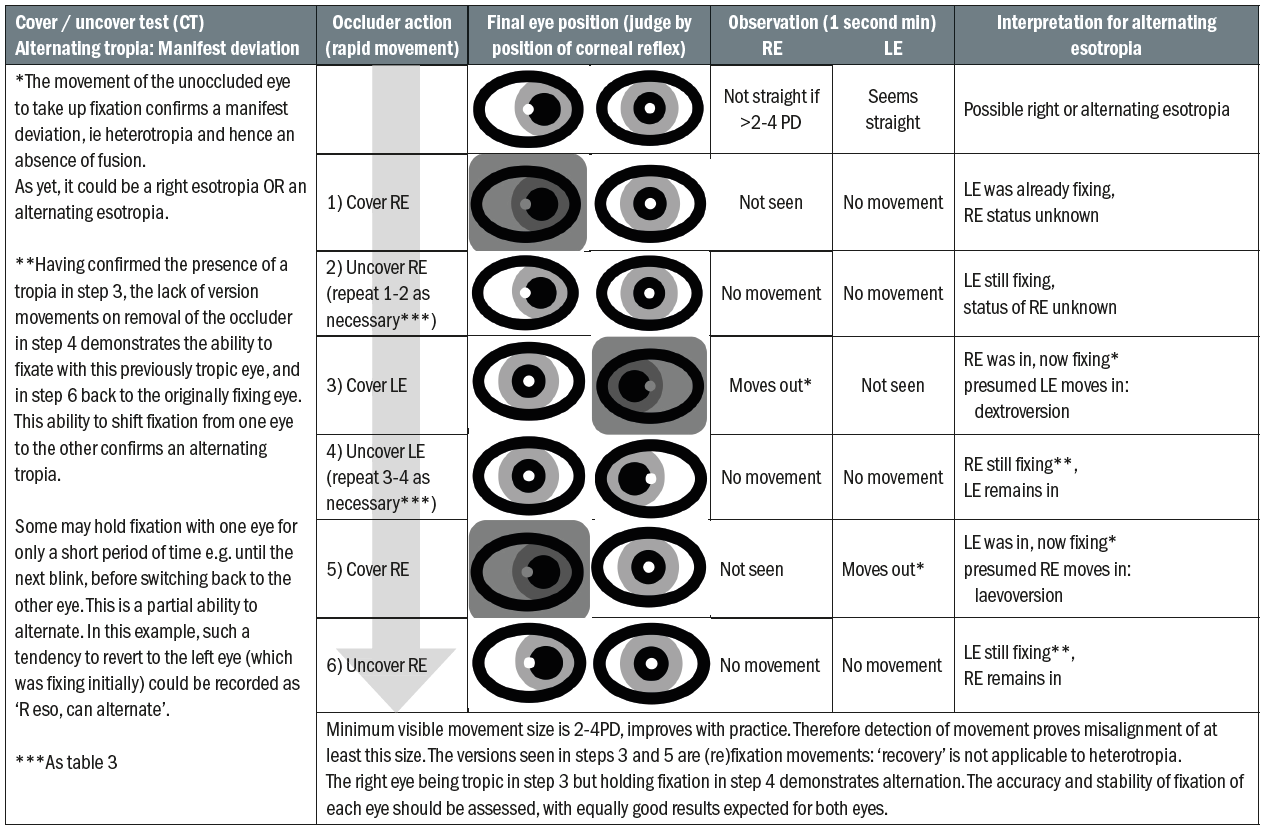
Table 6: Step by step analysis of cover/uncover test in alternating tropia. Note version movements on insertion of occluder only
Table 7 moves on to the alternating and prism cover tests. Here, the occluder swaps rapidly from eye to eye with no binocularity in between, but again time must be taken between movements for accurate observation. The ACT is typically performed after the CT has been completed. It cannot differentiate between a phoria or a tropia, or between a unilateral or alternating tropia, therefore it can never be diagnostic on its own. However, there are a number of advantages to the ACT.
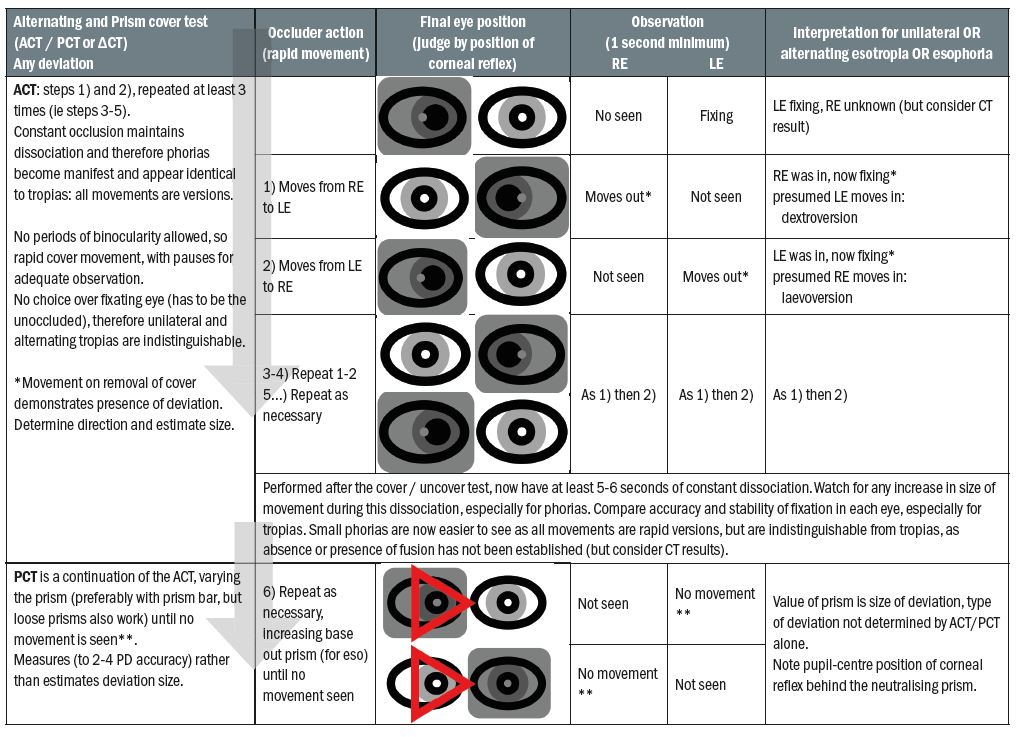
Table 7: Step by step analysis of alternating cover test and prism cover test in a non-specific eso-deviation. Note no period of non-occlusion and therefore version
Phorias remain manifest and therefore the eye movements are versions rather than vergences, and the rapidity of these movements make small deviations easier to see and describe accurately. Once the size and direction have been confirmed, the cover/uncover may be repeated to more readily allow for correct classification as a phoria or tropia.
Secondly, some phorias increase in size with prolonged occlusion. A properly conducted ACT should guarantee a minimum of five to six seconds of constant occlusion, enough time to allow an increasing phoria to become evident. This increase in size is clinically important, as it suggests that the phoria is more problematic than its initial size suggests, and that the vergence mechanism is struggling to keep it under control.
Thirdly, comparison of the speed of fixation for each eye can give valuable information about the quality of vision and the potential presence of amblyopia in each eye. This can help in building up a more complete history of the patient, and in deciding whether the correction of a tropia is likely to improve the sensory status. If a deviation is apparent in any of the above situations, then neutralising the deviation by identifying the value of prism that eliminates movement on the ACT gives a more accurate assessment of the size of the deviation, important in deciding treatment options. This is the prism cover test.
Once the combination of CT, ACT and PCT have been completed, the type, direction and size of the deviation will be known. For a phoria, the state of compensation can be judged by the speed of the recovery movement. For a tropia, dominance can be established and the possibility of poor vision / amblyopia can be judged. However, these statements are only true if the deviation is large enough to be seen ie at least 2 to 4 Δ. If no movement is seen, then the presence or absence of fusion, and therefore binocularity, has not been established. In these cases, supplementary tests can help.
Supplementary tests to the cover test
When there is no movement seen on the cover test, fusion has not been confirmed, and hence alternative investigations need to be considered. Subjective tests, such as Maddox rod or wing, can help detect the presence of a small deviation, but because they are dissociative, they cannot differentiate if the deviation is a phoria or a tropia.
Stereotests or dichoptic tests (such as the Mallett unit) can establish the level of sensory fusion, which indirectly supports the presence of motor fusion, but tend to require high levels of understanding and communication. Where compliance is limited, motor fusion can easily be confirmed by the criminally overlooked 10Δ test. This involves introducing a 10 base out prism while fixing a near target, effectively inducing a 10 exo-deviation. It should be performed in an identical manner to the cover/uncover test, replacing the occluder with the prism. The practitioner looks for the 10Δ convergence movement that should automatically occur on insertion of the prism. Observation of this movement (and/or the 10 divergence movement required when the prism is removed) confirms objectively the presence of fusion, but in addition the speed of the movement gives an estimate of the robustness of fusion, just as the recovery movement does in the cover test. This makes it an excellent addition to the cover test where a small phoria, which does not give a significant challenge to the vergence mechanism, is found.
If fusion fails and there are no vergence movements, the subject was (or has temporarily become) tropic. In this case, they will keep the dominant eye on the target by the use of version movements. Hence, they mimic the patterns of movements seen for a heterotrope on the cover test. A sluggish fusion response or a tropic response are indicative of a struggling / failing vergence mechanism. The 20PD test, identical in all but size, gives a bigger challenge to the vergence mechanism and hence is more sensitive in picking up poor or absent fusion. This is particularly important for screening young children who are still at risk of developing tropias and/or amblyopia. This could be extended to measuring fusional reserves and indeed this may be necessary when considering prescribing prism for decompensating phorias. A further additional test would be the near point of convergence (NPC). This is another quick and simple test that any fusing patient should automatically comply with to some extent.
Conclusion
The cover test is an essential tool in the optometrist’s armoury. It gives crucial information about binocular status in both adults and, crucially, young children, but only if conducted properly. Good technique is essential in gaining reliable results. Even if conducted properly, the cover test does not give the complete picture of the vergence mechanism, and has limitations in its ability to detect or assess small deviations adequately. Therefore, the role of supplementary or alternative instigations must also be understood for the benefit of good patient management.
Dr Fergal Ennis is a Senior Lecturer (Teaching and Scholarship) at Cardiff University.
