A recent review article1 has asserted that the preferred material for daily disposable lens (DD) wear is silicone hydrogel (SiHy). The authors Hogan and Woo state SiHy DD wear is healthier than hydrogel DD wear. This article aims to provide a balanced perspective given that the world’s most sold DD brand is a hydrogel, with very many successful wearers.
The three main things practitioners look for when providing a contact lens are good comfort, good vision and safety. To be specific, in the following areas there is a strong evidence base in the peer-reviewed literature that supports comfortable, safe and long-term hydrogel DD lens wear. Key areas will be considered in turn, namely:
- Corneal oxygenation
- Limbal hyperaemia
- Corneal neovascularisation in long-term wear
- Safety profile
- Comfort
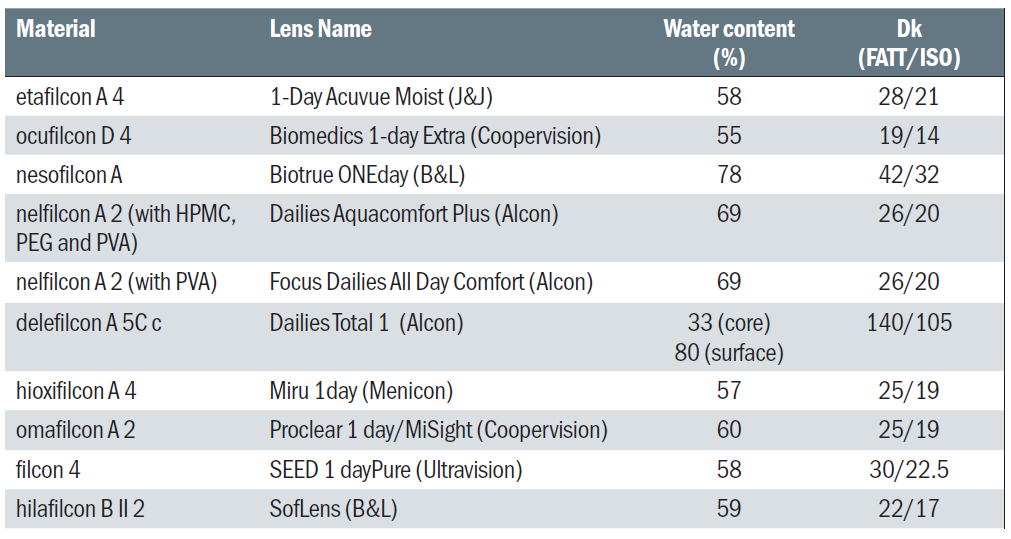
Table 1: Currently available hydrogel materials for daily disposable lenses in the UK
Corneal oxygenation
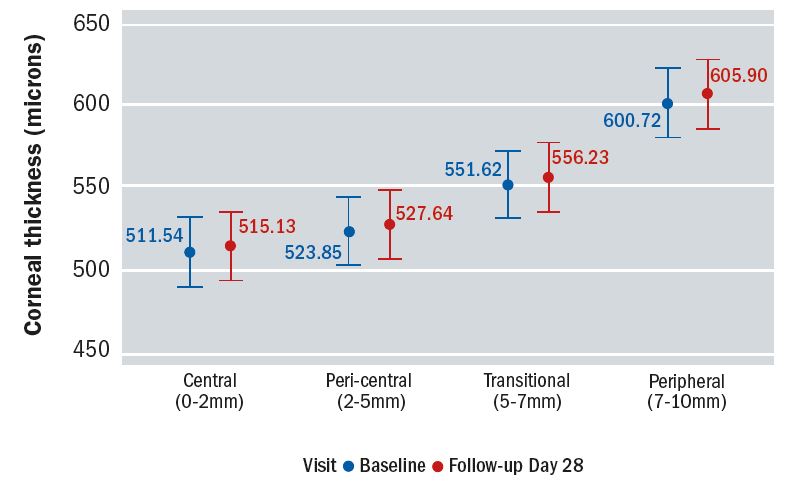
There is considerable evidence that market-leading high water content hydrogel lenses made of etafilcon A (1-Day Acuvue Moist) do not produce clinically significant levels of corneal oedema. The work of Szczotka-Flynn2 showed that there was no meaningful difference (≤0.85%) in central corneal oedema levels between etafilcon A and two SiHy lenses. This is supported by Moezzi et al,3 who measured central and peripheral corneal swelling in etafilcon A DDs compared to no-lens wear and found the difference centrally to be <1% and peripherally to be <1.5%, which was judged clinically equivalent (figure 1). In another study, where presbyopic SiHy wearers where refitted with etafilcon A DD multifocals, Moezzi et al showed no more than 0.9% difference in corneal swelling peripherally, which was also judged clinically equivalent.4
While there might be concern that these cited studies results do not reflect the level of corneal oedema after a full day’s wear, as the measurements were taken after six to eight hours of wear, the work of Holden et al5 shows that when subjects are exposed to the levels of oxygen present under a high water content hydrogel contact lens, that any corneal swelling peaks after two hours and remains stable thereafter. Thus, the time period over which these investigations into corneal oedema were carried out is more than sufficient.
Dr Noel Brennan 6 calculated that when etafilcon A is compared to lotrafilcon A (the SiHy material with the highest Dk), there is no difference in the actual central corneal oxygen consumption and a modest difference in actual peripheral corneal oxygen consumption.
Brennan is quoted in the ‘Why SiHy?’ publication,1 referencing an on-line forum from 14 years ago. In that time our understanding of the relevance of oxygen to contact lens performance has changed significantly and Brennan’s current thinking (along with that of the researchers mentioned previously), is reflected in another publication that appeared recently in Optician.7
Interestingly, a recent publication by Del Aguila-Carrasco et al8 demonstrated greater corneal swelling with a SiHy DD (Clariti 1-Day) than a hydrogel (1-Day Acuvue Moist). While counter-intuitive, this perhaps illustrates that there may be unknown factors that influence corneal swelling beyond oxygen supply alone.
Limbal Hyperaemia
Any small amount of peripheral corneal oedema may potentially induce some level of limbal hyperaemia. In the studies mentioned above, there was either no difference (see figure 2) or clinical equivalence, with the maximum difference in grading being 0.2 on a 0-4 scale.2
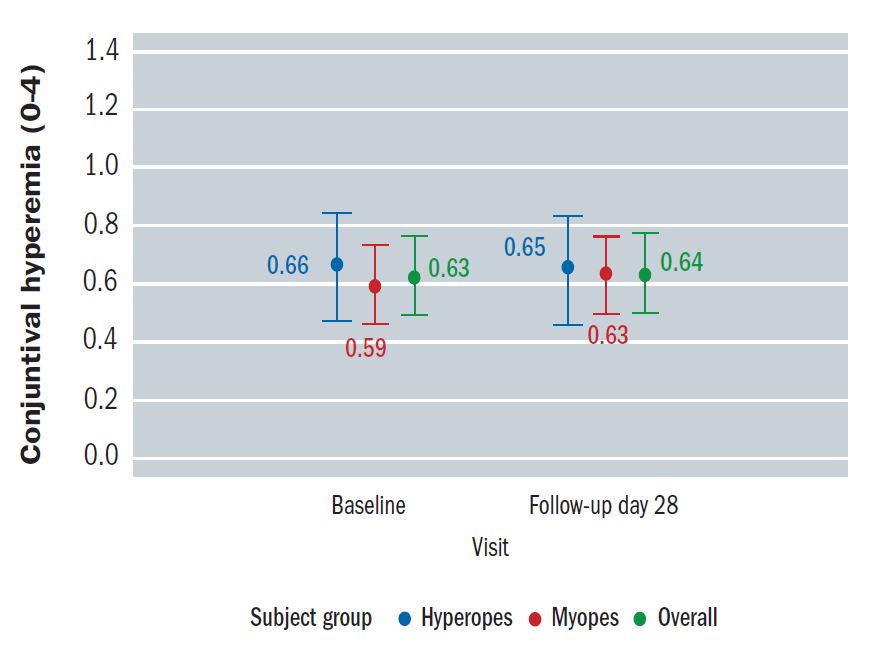
Furthermore, in the study of Diec et al,9 etafilcon A was compared to two SiHy lenses and the mean difference was also 0.2. Other studies10 have shown slightly greater differences (approximately 0.4) in grading of limbal hyperaemia between daily wear hydrogel and SiHy wear. It is generally accepted that a difference of 0.5 is clinically significant. In general, limbal redness resolves quickly on lens removal11 and is observed more as a potential aesthetic concern rather than an indication of significant corneal stress.
Neovascularisation in long-term wearers
Etafilcon A disposable contact lenses were introduced in 1987, leading to more than 30 years of clinical experience with millions of wearers worldwide. Regulatory authorities and practitioners around the world have not raised any concerns about corneal neovascularisation resulting from these market-leading high water content hydrogel lenses. In the study cited in the review article by Yeung et al,12 the definition of neovascularisation was vessel extension of 0.5mm or more. This is very significantly below the upper threshold of <1mm that constitutes grade 1 (no clinical concern) in the Efron Grading Scale and no data is presented as to how many individuals studied showed levels that would be greater than grade 1. This study contradicts previous work that showed the level of Dk/t to avoid corneal neovascularisation fell below that provided by modern high water content daily disposables.13
Exceptional safety profile
The implication made in the Hogan and Woo publication is that hydrogel DD lens wear is less safe than SiHy DD wear. Published peer reviewed evidence refutes this. In the largest registry study ever involving DD lens wear, conducted over 12-months, involving 570 patients, the etafilcon A lens (1-Day Acuvue Moist) was associated with no symptomatic corneal infiltrative events or other serious adverse events and only three non-serious events (0.6%/year).14*
This finding is supported by an independent, retrospective analysis that looked at 28 lens/solution combinations, each tested on approximately 40 patients wearing lenses on a daily wear basis for a three-month period.15 Lenses were frequent replacement and DDs, hydrogels and SiHys. Solutions included hydrogen peroxide and multipurpose. The overall adverse event (AE) rate was 3.6 events per 100 participant-months. Rates were low for the four DD lenses tested and significantly lower in DDs compared with reusable daily wear lenses. The only lens in the study that did not have any reported AEs was a hydrogel DD (1-Day Acuvue Moist) made of etafilcon A.
A two-year case control study identified new cases of contact lens-related microbial keratitis (MK) in wearers using DDs.16 A total of 963 DD wearers were identified, from which 67 MK cases and 374 controls were sampled. The study found that risk varied with DD lens type and certain DDs had lower rates. Etafilcon A had the lowest risk of all the lenses evaluated. The absence of any significant benefit arising from SiHy wear in MK rates during daily or overnight wear has been confirmed by several studies,17-20 so assuming the higher Dk/t of SiH DD will reduce the risk of MK in a patient who non-compliantly sleeps or naps during wear is not supported by any evidence.
In CooperVision’s three-year study looking at myopia progression in paediatric hydrogel DD lens wearers,20 the authors state ‘No safety concerns were evident for this population of children who started daily disposable soft contact lens wear between eight and 12 years of age.’ This should provide further reassurance to practitioners that they are not doing any harm in fitting hydrogel DD lenses.
In fact, there is absolutely no evidence that hydrogel DDs are less safe to wear in any respect than SiHy DDs.
Comfort
Finally, turning to comfort, the factor that is most linked to drop out from CL wear.22,23 There are studies that were not cited in the Hogan and Woo review that challenge the perception that all SiHy lenses are as or more comfortable than hydrogel lenses.24,25 Additionally, a recently published study with three SiHy DDs and two hydrogel DDs from three manufacturers, making lenses distributed in all major global markets, shows one of the hydrogel DD CLs to be significantly more comfortable than one of the SiHy DD CLs.26 The authors deemed the difference to be clinically significant. The hydrogel lens brand in question (brands are not revealed in the publication) was shown to deliver comfort levels similar to those experienced by non-lens wearing emmetropes.
Conclusion
To conclude, we continue to believe that practitioners should always select the best contact lens for patients based on overall comfort, visual performance, safety and clinical need. Oxygen has very little impact on any of these, suggesting that an evidence base does not exist to support the notion that Dk/t should be used as the primary basis for the selection of lens type.
There may be occasions where consideration of oxygen access may be important for patients who are, for example, predisposed to vascularisation with the thicker designs of some toric lenses or higher spherical refractive errors. There is no doubt that some SiHys can offer comfort and vision benefits due to lower coefficient of friction and tear lens stability.27 However, for many patients, hydrogel DDs continue to play an important role as part of the portfolio of products that practitioners can offer and, in many cases, will be more comfortable and result in very low adverse events. To suggest otherwise is failing to acknowledge the considerable evidence base.
David Ruston is director global professional education and John Meyler is senior director global professional education at Johnson & Johnson Vision.
References
- Hogan C, Woo S. Why SiHy? Optician, 2019; 260 (6709): 28-32
- Szczotka-Flynn LB, Raghupathy S, Debanne S et al. Daily wear central corneal swelling with etafilcon A is non-inferior to two silicone hydrogel lens types. Optom Vis Sci 2015; 92.
- Moezzi A, Varikooty J, Schulze M et al. Corneal swelling with cosmetic etafilcon A Lenses versus no lens wear. Optom Vis Sci 2016;93,6:619-628.
- Moezzi A, Varikooty J, Luensmann D et al. The short-term physiological impact of switching reusable silicone hydrogel wearers into a hydrogel daily disposable multifocal. Clin Ophthalmol. 2019;13:1193–1202.
- Holden BA, Sweeny DF, Sanderson G. The minimum precorneal oxygen tension to avoid corneal edema. Invest Ophthal & Vis Sci 1984;25:4 476-480.
- Brennan NA. Beyond flux: total corneal oxygen consumption as an index of corneal oxygenation during contact lens wear. Optom Vis Sci 2005;82:6 467-72.
- Brennan N, Ruston D. New insights into the long-term success of etafilcon A daily disposable contact lenses. Optician, 2018; 257: 6645, 20-22.
- Del Aguila-Carrasco A, Dominguez, V, Perez-Vives C. Assessment of corneal morphological changes induced by the use of daily disposable contact lenses. Cont Lens Anterior Eye. 2015 Feb;38(1):28-33.
- Diec J, Lazon de la Jara P, Willcox M et al. The clinical performance of lenses disposed of daily can vary considerably. Eye Contact Lens 2012;38:5 313-8.
- Maldonado-Codina C, Morgan PB, Schnider CM et al. Short-term physiologic response in neophyte subjects fitted with hydrogel and silicone hydrogel contact lenses. Optom Vis Sci 2004;81:911-21.
- Holden BA, Sweeney DF, Swarbrick H, Vannas A, Nillsson KT, Efron N. The vascular response to long-term extended contact lens wear. Clin Exp Optom 1986;69:112-19.
- Yeung KK, Yang HJ, Nguyen AL et al. Critical contact lens oxygen transmissibility and tear lens oxygen tension to preclude corneal neovascularization. Eye & Contact Lens 44: S291-S295, 2018
- Chan WK, Weissman BA. Corneal pannus associated with contact lens wear. Am J Ophthalmol 1996;121:540–546.
- Chalmers RL, Hickson-Curran S, Keay L et al. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci 2015;56:654-663.
- Diec J, Papas E, Naduvilath T et al. Combined effect of comfort and adverse events on contact lens performance. Optom Vis Sci 2013;90:7 674. *This observational/surveillance registry relied on patient reports of symptomatic adverse events that led them to seek clinical care. These results should be considered in conjunction with other clinical results on the safety and efficacy of daily disposable etafilcon A contact lenses, which also generally show low rates of such events. Although no symptomatic infiltrative events were reported in this study, such events can occur with daily disposable lenses, including 1-Day Acuvue Moist, as noted in the product labelling.
- Stapleton F, Naduvilath T, Keay L et al. Risk factors and causative organisms in microbial keratitis in daily disposable contact lens wear. PLoS ONE 2017;e0181343.
- Schein OD, McNally JJ, et al. The incidence of microbial keratitis among wearers of a 30-day silicone hydrogel extended-wear contact lens. Ophthalmology 2005;112(12):2172-9.
- Dart JK, Radford CF, et al. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology 2008;115(10):1647-54, 1654 e1-3.
- Stapleton F, Keay L, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology 2008;115(10):1655-62.
- Stapleton F, Keay L, et al. The epidemiology of microbial keratitis with silicone hydrogel contact lenses. Eye Contact Lens 2013;39(1):79-85.
- Chamberlain P, Peixoto de Matos S, Logan N. et al. A 3-year randomized clinical trial for MiSight lenses for myopia control. Optom Vis Sci 2019;96(8):556–567.
- Young G, Veys J, Pritchard N et al. A multicentre study of lapsed contact lens wearers. Ophthal Physiol Opt 2002;22:516-52.
- Weed K, Fonn D, et al. Discontinuation of contact lens wear. Optom Vis Sci 1993;70(12s):140.
- Guillon M. Are silicone hydrogel contact lenses more comfortable than hydrogel contact Lenses? Eye & Contact Lens 2012; 39.
- Maissa, C, Guillon, M, Garofalo, R. Contact lens-induced circumlimbal staining in silicone hydrogel contact lenses worn on a daily wear basis. Eye & Contact Lens: Science & Clinical Practice. 2012: 38(1):16-26.
- Lazon de la Jara, P. Diec, J. Naduvilath, T. et al. Measuring daily disposable contact lenses against non-wearer benchmarks. Optom Vis Sci 2018;95:1088–109.
- McParland M, Pall B, Schnider C. New lens for demanding days. Optician 2016 251; 6555: 24-28.
