In the introductory article in this series (Optician 15.03.19), the hierarchy of sensory fusion was discussed (see figure 1). We can see that the first step towards binocularity is that both retinal images must be perceived, ie simultaneous perception. Once perceived, they need to be fused together into a single percept (flat fusion) in order to achieve binocular single vision. If flat fusion has been achieved, the binocular system is in a position to analyse any disparities between the two retinal images, with the possibility of extracting information about the relative depth of the objects in space that are generating these disparities. This form of depth perception, stereopsis (as opposed to depth perception due to monocular cues), is the pinnacle of the sensory fusion hierarchy and indeed is the raison d’être for forward-pointing eyes with overlapping visual fields. 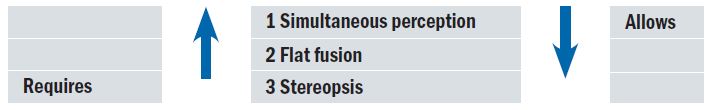
Figure 1: Increasing degree of heterophoria is likely to increase the chances of decompensation, leading to changes in severity, frequency and type of symptoms. However, it is not a simple linear relationship.
This position at the pinnacle suggests it would be a useful starting point in the investigation of sensory fusion. If good stereopsis is demonstrated, then flat fusion must be occurring (and therefore does not need to be demonstrated), and therefore simultaneous perception must be present (again, no direct demonstration is needed). In short, stereo testing can quickly demonstrate that sensory fusion is robust. This in turn demonstrates that motor fusion is occurring (the subject must be bifoveal to achieve good stereopsis) and if motor fusion and sensory fusion are both present and correct then the binocular system as a whole is working well.
The clinical usefulness of assessing stereo is therefore apparent. However, measuring stereopsis is only a snap-shot, not the whole picture. It is clinically important to understand not just the advantage of measuring stereo, but also of both the limitations of the tests that provide us with the measure and the significance of that measure. First, we need to understand retinal disparity and stereopsis.
How stereopsis works
Figure 2 gives a simple illustration of how a solid object, profiled in depth, results in a stereoscopic percept. The small spine of the book is closer to the viewer than the larger background wall: the hexagonal outline of the wall provides the frame of reference (2a). Closing each eye, in turn, will give two views of the book (2b), and it is immediately obvious that these two views, and hence the two retinal images, are not the same. Alternating between the eyes will generate the illusion that the spine of the book moves from side to side. This movement is because the spine of the book is in a different location on each retinal image, ie we have retinal disparity (2c). Because the spine is closer to the subject, it will fall on the temporal retina of each eye (2d).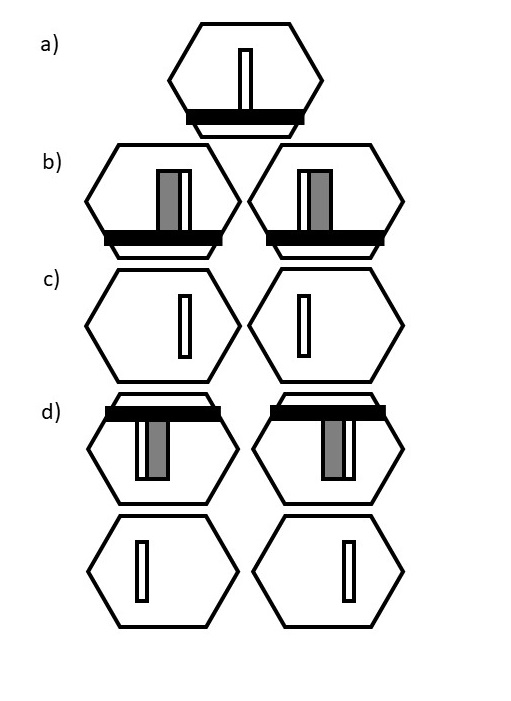
Figure 2: a) The binocular view of a book placed perpendicularly on a shelf, mounted on an hexagonal wall. b) The left and right eye views whilst focusing on the wall (as opposed to the book spine). Note the nasal displacement of the spine for each eye. c) The components of the binocular view of the book (ie the spine) that generate retinal disparity between the two retinal images. d) The retinal images corresponding to b) and c). Note the temporal displacement in the retinal images for the protruding spine. Any method of generating such a retinal disparity will generate the perception of nearness. (The synoptophore uses slides similar to the two views in c) to generate a stereoscopic percept, allowing for measurement of stereo thresholds).
This temporal displacement generates positive retinal disparity and is always associated with an object nearer than the fixation point (nasal/negative disparity relates to a more distant object than the fixation target). Specific disparity-sensitive cells have been demonstrated in the primary visual cortex (V1). Some of these cells respond to positive and the others to negative disparities. Within these two groups, cells are tuned to specific degrees of retinal disparity, with greater disparity signalling greater depth. Hence accurate judgements can be made about the direction and degree of depth.
Even for the most sensitive finely-tuned cells, there must be a finite amount of retinal disparity present, generated by a finite amount of depth within the visual scene. In other words, there is a stereo threshold. This minimum retinal disparity is calculated in terms of the angular displacement of the disparate retinal images, or the angular difference in direction between the front and rear of the object and is recorded in seconds (”) of arc. The fact that this occurs in V1 means that stereopsis occurs before, and therefore independent of, our conscious interpretation of the contents of the visual scene. It is therefore as fundamental a property of our visual system as any other.
How stereo tests work
Commercially available stereo tests come with their own set of instructions. Hence, the detailed performance of individual tests will not be dealt with here (but there is a summary of some key properties of commonly used tests in table 1). Instead, a general understanding of the underlying principles will be discussed as to how the stereo threshold is measured by ascertaining the minimum amount of change in depth that a subject can detect.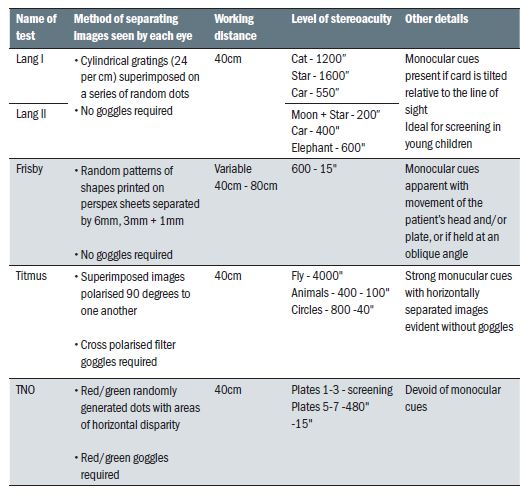
Table 1
The Frisby stereo test (figure 3) works very simply in this way, with parts of the visual scene printed on the front and back surfaces of a transparent plate of known thickness. The remotest distance at which the subject can detect the depth correctly, in combination with the thickness of the plate, can be transformed mathematically into a stereo value. The Frisby is one of only a few stereo tests that use real depth objects to generate retinal disparity and stereopsis.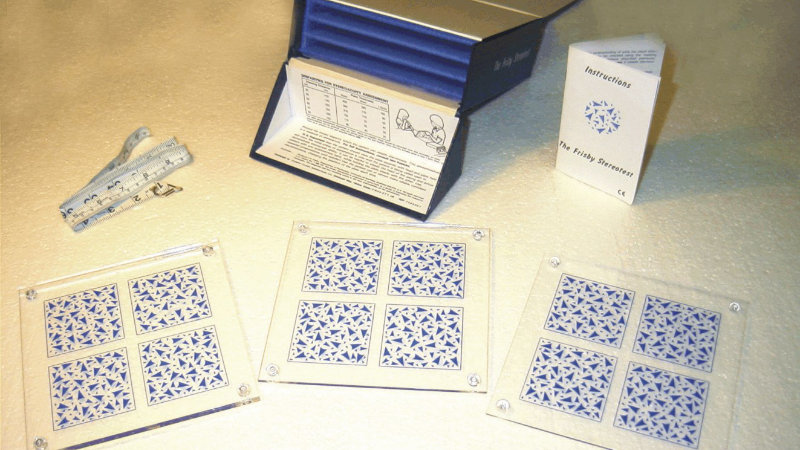
Figure 3: The near Frisby stereo test. On each plate, one of the squares has a circle printed on the reverse surface. No filters/goggles are required: good for young children.
Retinal disparity generated by any means will result in the perception of depth and this has been utilised in a number of familiar clinical tests. These tests must adopt some method of dichoptic presentation (where parts of the scene are visible to one eye only), usually by the use of appropriate filters.
One common example is the Titmus Fly test (figure 4). In this test, most of the visual scene is common to both eyes, but one component within each testing target is dichoptic (generated by cross polarisation), and this part is shifted inwards/nasally for each eye thereby generating the required positive retinal disparity for the component to appear to come closer.
Figure 4: The Titmus fly stereopsis test with polarised filters. Note the clearly ‘different’ buttons and animal in the top rows which can be seen monocularly.
Through the sequence of targets (1 to 9 or A to C) the disparity gets less, therefore the depth is more subtle, therefore a threshold can be attained. The subject simply needs to correctly identify which component is ‘coming out of the page’, or they can be asked to ‘push it back in’ or to pick up the fly by the wingtips. The fly has only one level of coarse stereopsis, therefore it cannot be regarded as recording a threshold, but it does allow for the demonstration of the presence of stereopsis in a young or non-communicative subject.
The synoptophore (figure 5) uses a similar stimulus approach to generating disparity within the two retinal images (the similarity between the Titmus diamond targets and the synoptophore hexagonal targets in figure 2c should be apparent) but uses a different dichoptic approach in that it places each of a slide pair in the right and left telescopic components. Although formerly a stalwart in hospital orthoptic departments, synoptophores are rarely found on the high-street and hence will not be discussed further in this article.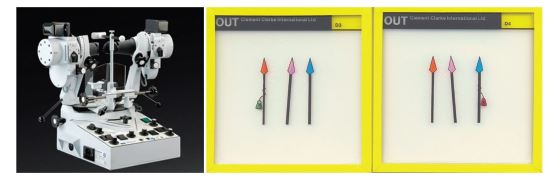
Figure 5: The synoptophore with a pair of slides that generate retinal disparity of the central spear, which is seen in depth.
A different approach is to use random dot stereograms. Figure 6 illustrates the basic principles involved. Two identical random dot arrays are presented dichoptically. Remarkably, the binocular system is able to fuse what appears to be two fields of noise: there is no discernible shape in either the right or the left retinal image. Within each array, an identically shaped and located patch of dots is displaced nasally, generating the desired positive retinal disparity.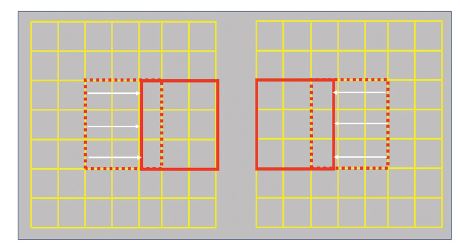
Figure 6: Random dot stereograms. Each grid is populated with the same pattern of random dots (black/white, or red/green are typical
combinations). The square of dots that has been displaced nasally for each eye will be seen as above the rest of the grid.
The disparity cells in V1 detect and process this disparity, and the shape suddenly becomes visible. The TNO (figure 7) is based upon this principle. It has a range of plates with decreasing disparity (the pie with a slice missing plates), hence a threshold can be recorded. It also has a number of screening plates, easy for children to use, which may not give an accurate threshold but can at least confirm the presence of stereo processing.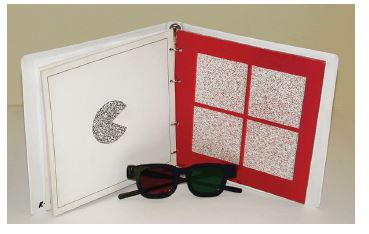
Figure 7: The TNO stereo test, showing the type of target that can be seen stereoscopically (the pie) but that is not visible without the red/green filters.
Another example is the Lang stereo test (figure 8). This test achieves dichoptic separation by the use of interleaving random dot strips and horizontal bi-prisms, deviating one half of the strips to one eye, the other half to the other eye. Only a limited range of coarse targets are used, hence a true threshold cannot be established, but because it requires no filters, it is a very useful screening test for young or reduced-compliance subjects.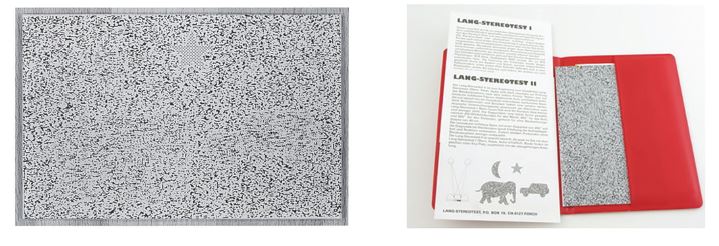
Figure 8: The Lang (version 2) stereo test. Note the monocularly visible star, there to demonstrate compliance. No other objects are clearly visible, but note areas of subtle irregularities in the randomness of the rest of the plate, giving clues to the location of the stereo targets. No filters required, and practitioner can watch over the top for objective confirmation of accurate fixation.
It is important to recognise that although all stereo tests rely on the generation of retinal disparity to assess stereopsis performance, the different tests achieve this in different ways. This can lead to poor agreement of results between tests, especially if the stereopsis is compromised. Therefore, where practicable, for consistency of results the same test should be used in follow-up visits. If this is not possible, comparison of results must be approached with caution.
Interpretation of results
As with any test, a critical approach must be taken as to the validity of any result before using it for diagnostic or management purposes. To gain reliable results, the test instructions should be followed correctly, or erroneous results can occur, either quantitatively (the accuracy of the threshold recorded) or qualitatively (the confirmation or denial of stereopsis when in a screening mode).
Testing distance is critical, as any change in the distance will affect the angles generated and hence will change the results. Testing too close makes it easier and gives falsely high thresholds, the opposite for being too remote. Tests should also be held perpendicular to the subject, and there should be no movement (especially side to side movements) particularly for the Frisby and the Lang. Tilting or movement can give clues to the presence of the stimulus even in the absence of stereopsis due to parallax or motion parallax respectively. Hence due to the monocular cues of parallax, a positive result could be obtained in a monocular patient: clearly a false positive result.
The Titmus can also give false positive results. It is clear from figure 4 that there is something different about the bottom button in the first diamond (and to the discerning viewer, diamonds 2 and 3 can also reveal a similar subtle difference), and similarly the cat in row A. When viewed through the filters monocularly (hence precluding any possibility of stereopsis) the relatively large lateral displacements of these coarse-stereo targets make them ‘different’ from those around them and the subject may identify this positional difference rather than a depth difference. Hence the top row of both diamonds and animals can give false positive results and should not be taken as convincing evidence of stereopsis. They should still be used, however, as they give a readily performable start to the test for the shy or reluctant subject. Any correct answers beyond the top rows can be considered as valid and truly indicative of stereopsis.
The TNO is immune to such false positives from monocular cues. The target is completely invisible in the monocular retinal image, therefore positioning or parallax are not relevant. Motion parallax in depth can occur if the test is moved, but the parallax only occurs once the object is perceived stereoscopically, so the appropriate level of stereopsis must be present. The same should be true of the Lang test, but the bi-prism method of partial dissociation is very prone to sideways motion cues. Also, from figure 8, the discerning viewer might not be able to identify the objects hidden in the stereogram, but they might detect some areas of ‘non-randomness’ in the test that could give a false positive result. A ‘borderline’ confirmation of stereopsis by occasional/intermittent fixing of the targets should therefore be treated with some scepticism, although concentrated fixing of the hidden targets should be taken as a true positive result.
Many naïve subjects find random dot stereograms a little difficult at first (the TNO in particular) so time needs to be given for the subject to get to grips with the task before recording a negative result. Once they have seen the first target, speed for subsequent targets rapidly increases, and on repeat testing this learning effect seems to be retained. But the practitioner must be wary of ‘failing’ the subject too soon as this could give a false negative result. Indeed, false negatives are a risk with all stereo tests. They are all subjective and in some ways are a little abstract. This can make it difficult for the inexperienced subject, who may then withdraw from the process. Therefore, a complete failure to detect stereo should not automatically be interpreted as an absence of stereo, it should be repeated and considered in the light of other binocular vision findings.
Use of stereopsis results in heterophoria
Once we have evaluated the validity of the results, we need to consider how to use them in patient management. Stereopsis is most relevant in heterophoria, where it has a role in evaluating the state of compensation. The role is indirect in that we are using sensory fusion data in order to infer, rather than directly assess, the state of motor fusion.
In orthophoria and in a fully compensated phoria good stereopsis is to be expected. By definition the subject is bifoveal and can maintain this position with ease, hence we would expect the motor status to have no negative impact on the sensory status. As the phoria begins to decompensate, bifoveality becomes harder to maintain. This can lead to a reduction in stereopsis. As things get worse, a central suppression scotoma may develop in order to avoid central diplopia. This loss of bifoveality will have a much more significant impact, with only coarse levels of stereo now possible. Further decompensation will lead to heterotropia and diplopia, with no stereo at all as flat fusion is no longer present. So as the state of decompensation worsens, so does the stereopsis. However, decompensation is not the only cause of poor stereo.
There may have been developmental issues as a child which impacted upon the binocular development, or there may be an idiopathic reduction or absence of stereo. Reduced visual acuity, particularly monocularly, can also interfere with stereopsis. Therefore, when reduced stereo is found, other evidence for decompensation should be sought. Decompensating phoria as the cause can be confirmed by the introduction of a relieving prism, ie a prism that reduces the size of the phoria and therefore the demand on the vergence mechanism. An exact amount of relieving prism may be suggested by fixation disparity or fusional reserves results, but a sensible estimate would be sufficient. If the relieving prism improves stereo, this is firm evidence that the phoria is decompensating and requires investigation and management. Identification of the minimum amount of relieving prism that yields the maximal stereo performance can be considered a method of establishing the amount of prism that should be considered for prescribing. If no improvement is found, then the reduced stereo cannot be considered as evidence of decompensation. Either way, the stereo result needs to be viewed in the light of other test results that relate to the state of compensation.
Use of stereopsis results in heterotropia
Some would argue that testing stereopsis in a tropia is pointless as motor fusion has broken down and therefore sensory fusion must also have broken down. This is not quite true. If a tropia has recently developed in an adult, either as a result of disease or trauma or from decompensation of a pre-existing phoria, diplopia is almost certain to occur and stereopsis will fail. However, in early onset heterotropia (in young children within the plastic/sensitive periods) adaptations to the tropia can develop such that peripheral binocular may persist and hence coarse stereopsis is possible. These adaptations persist into adult life, and hence any patient with an early onset tropia may have residual binocular function and testing for stereopsis can confirm its presence. This is clinically valuable, as it suggests the tropic eye is not being ignored and therefore needs to be considered in the overall patient management.
Conclusion
As the pinnacle of sensory fusion, stereopsis is a relatively quick and easy way to establish how well the eyes work together from a sensory point of view, with a good result confirming good sensory fusion and indirectly suggesting good motor fusion. Quantitative measures can aid in the detection and management of decompensating heterophoria, and qualitatively it can establish the presence of some level of binocular function, even in the presence of heterotropia.
However, there are sources of error that can lead to false positive or false negative results. Therefore, the practitioner needs to understand how their test works and the implications of correct or incorrect implementation. As a subjective test, there is always going to be a possibility of false negative results due to non-understanding or non-compliance in some patients. Therefore, a diagnosis of absence of stereopsis should be confirmed either by repeat testing or by consideration of other sources of evidence. Indeed, as with any test of the complex binocular vision system, interpretation of results in isolation is unwise, and a full picture should always be aimed for before a diagnosis is made and a management plan formulated.
Dr Fergal Ennis is a Senior Lecturer (Teaching and Scholarship) at Cardiff University.
