The extracellular matrix (ECM) is a complex structure combining structural proteins, enzymes and soluble factors which interact with the surrounding cells and allow maintenance of tissue structure and homeostasis of the cellular environment. Damage to ECM through disease or trauma triggers a molecular response from components of the ECM which enhance tissue recovery and wound healing. One group of ECM components known to be essential to this wound healing process are the heparan sulphate (HS) glycosaminoglycans. In recent years, bioengineered structural analogues of HS have been introduced, known by the trademarked acronym RGTA, standing for ReGeneraTing Agents. In this article, we will look at the nature of RGTAs in general, their use in ocular disease, and show a case study illustrating their use.
Tissue Damage
The ECM in mammals has over 300 proteins associated with it. These include three major groups of central proteins:
- Collagens; the major structural elements of ECM
- Proteoglycans; the ‘filler’ substance existing between cells in an organism, forming large complexes to other proteoglycans, hyaluronan, and to collagen. They have attached glycosaminoglycans chains which sequester water and bind growth factors
- Glycoproteins; act as a reservoir for growth factors and contribute to ECM structure and intermolecular communication
Along with these are found a wide range of further proteins, such as enzymes, growth factors and cytokines, which all contribute major roles in homeostasis (maintenance of a stable cellular environment) and structural stability and re-modelling. The balanced ECM is disrupted by direct trauma and by a wide range of diseases, such as osteoarthritis and malignant disease, both of which cause disruption of the normal regulation of ECM components.
One important group of proteoglycans is the heparan sulphate proteoglycans (HSPGs) which comprise a protein core and one or more attached glycosaminoglycans chains of heparan sulphate. These chains play an important role in tissue homeostasis, namely:
- Structure; HSPGs bind matrix proteins such as collagens, fibronectin and laminin at specific ‘HS-binding sites’, protecting these proteins from proteolytic degradation and forming a scaffold around cells, thereby contributing to the spatial organisation of the ECM.
- Protection; HSPGs bind growth factors, cytokines and chemokines. They protect them from degradation and control their retention, thereby regulating their local concentration and signalling capabilities.
After extensive damage to tissue, haemostasis and inflammation result followed by cellular proliferation and tissue remodelling. During this process, cells involved in the inflammatory response (macrophages, neutrophils) and resident cells at the wound site (keratinocytes, fibroblasts and endothelial cells) release enzymes (heparanases and proteases) into the injured tissue. This triggers the following:
- Degradation of HS
- Destruction of the ECM scaffold
- Release of HS-bound communication polypeptides into the ECM, stimulating the rapid repair of tissue
- Resolution of the inflammatory response
Scarring or fibrosis occurs, a rapidly formed but less defined tissue which acts as a barrier to further infection and, to a degree, insult. In some chronic wounds, as with, for example, vasculitis or in diabetes, the damaged area remains in a state of inflammatory response with a continued degradation of the ECM.
Matrix Therapy
ReGeneraTing Agents (RGTAs) are heparan sulphate mimics, specifically designed to replace degraded HS in damaged tissue, so accelerating the speed and enhancing the quality of tissue repair.1 Although structurally and functionally analogous to naturally derived HS, one of the most crucial properties of RGTA is its resistance to enzymatic degradation. This allows RGTAs to retain their structure and activity even in the microenvironment of chronic wounds, characterised by unrestrained proteolytic activity.2,3
The action of RGTAs is outlined in figure 1. Note how excess RGTA may lead to inhibition of wound healing and so the appropriate RTGA level for any specific tissue needs to be established.
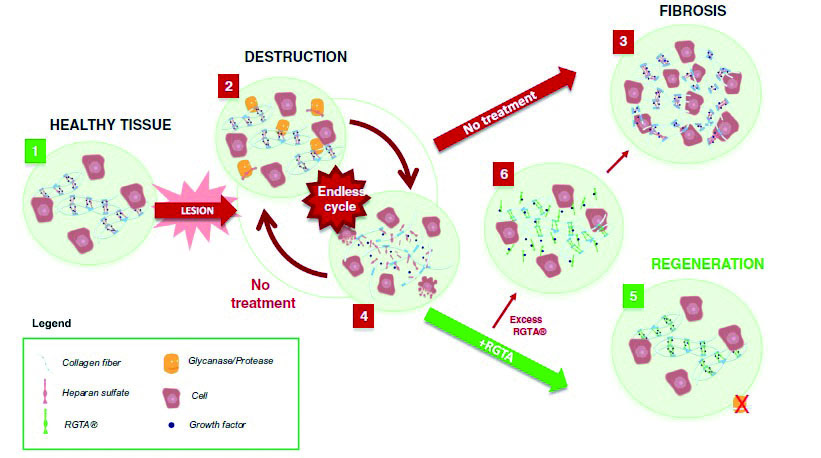 Figure 1: Action of RGTAs. 1: Healthy tissue and the organised ECM. 2: Tissue damage results in degradation of HS and destruction of the ECM. 3: Chronic wounds do not resolve and end in an inflammatory cycle of repair and destruction. 4: RGTA replaces HS and promote ECM scaffold repair and restoration of tissue to a healthy state.
Figure 1: Action of RGTAs. 1: Healthy tissue and the organised ECM. 2: Tissue damage results in degradation of HS and destruction of the ECM. 3: Chronic wounds do not resolve and end in an inflammatory cycle of repair and destruction. 4: RGTA replaces HS and promote ECM scaffold repair and restoration of tissue to a healthy state.
Clinical Use
RGTAs have been used to enhance tissue recovery in a wide range of tissues. These include:
- Cornea; a number of corneal diseases have been shown to respond well to RGTAs, as discussed later
- Skin; lesions such as necrotic ulcers and burn damage
- Oral and digestive tract; oral mucositis, periodonitis, some gastric lesions and colonic leakage
- Bones, joint and tendon; bone defects and tendonitis
- Muscle; animal studies have shown some benefit in assisting myocardial infarction recovery
- Others; use has been reported in assisting recovery in a wide range of conditions, including perforation of the ear drum and crushing of the sciatic nerve
Ocular Use
RGTAs as an agent promoting tissue recovery have been concerned primarily with the ocular surface and, in particular, the cornea. Their use has been shown to be effective in the management of two main groups of eye condition:
- Neurotrophic keratitis; is a rare degenerative corneal disease caused by an impairment of trigeminal corneal innervation, leading to a decrease or absence of corneal sensation. The corneal epithelium is the first target of the disease showing dystrophic changes and defects with poor tendency to spontaneous healing. The progression of the disease may lead to corneal ulcer, melting, and perforation. The incidence of neurotrophic keratopathy increases with age.4 Table 1 outlines some of the causes of neurotrophic keratitis.
- Persistent epithelial erosion or defect (figure 2); although most corneal epithelial defects heal quickly and without incident, under certain conditions the epithelial defect may be slow to heal, or sometimes not heal at all. When these defects do not heal within the normal time frame (usually defined in the literature as two weeks), they become known as persistent epithelial defects (PED).5 Practitioners will be aware of the PED patient reporting a sharp ocular pain after waking as the overnight epithelial regrowth is dislodged with blinking. Table 2 summarises some causes of PED. Management with non-preserved lubricants is appropriate for milder cases, while more severe and persistent cases usually need ophthalmological interventions.6
Figure 2: A persistent epithelial erosion.
There has also been cited some potential for RGTAs in the management of corneal ulcer and severe chronic dystrophy resistant to usual therapies.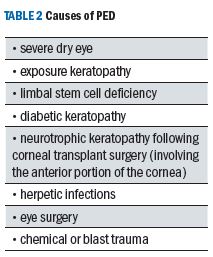
Cacicol
The RGTA available for ocular surface use is called Cacicol. Cacicol is a sterile preservative-free ophthalmic solution containing poly-carboxymethylglucose sulphate, a heparan sulphate analogue, and is licensed to Thea (UK distribution from MidOptic). It is supplied in single dose preservative-free units. As yet, specific treatment protocols have not been established. Interestingly, the agent is not classed as a drug but as a medical device. Cacicol should not be used on:
- •Patients under 18
- •Pregnant or breastfeeding patients
- •Where active infection is present
- •If a local antibiotic (from aminoglycosides group) is being used
- •With any solutions containing silver salts, iodine or copper
As yet, much of the effectiveness of Cacicol on corneal disease has been published on a case by case basis, but these tend to show positive results in an increasingly wide range of presentations.7-14
Case Study
In September 2018, patient DT, a 33-year-old chef and long-term patient of the practice presented with a report of trauma to his right eye. While at work, he had been hit in the eye with a piece of Tupperware.
Initial assessment showed a deep corneal abrasion (figure 3), and the first line of management was:
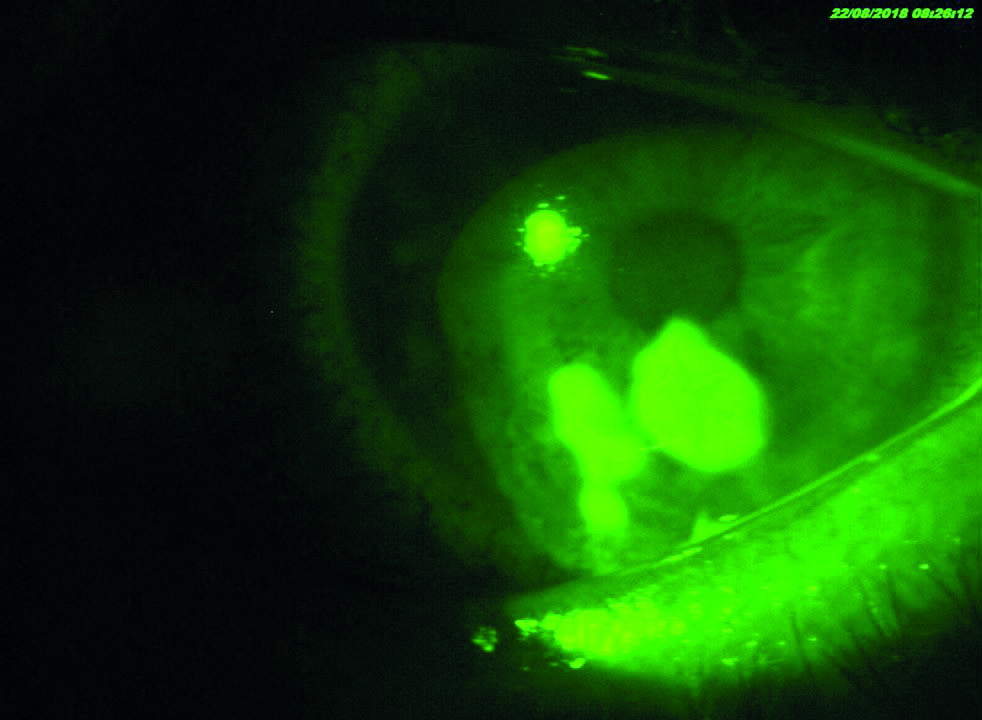
Figure 3: Cornea at first presentation.
- Cycloplegia for pain relief
- Bandage contact lens (BCL) for comfort
- Intense lubrication
For a bandage lens, a frequent replacement SiHy (‘off the shelf’) was preferred as this allowed easy replacement as necessary. Cycloplegia is good for relieving pain as it paralyses the ciliary body, so relieving ciliary spasm.
The aim of using a bandage contact lens is to:
- Offer mechanical protection and support
- Reduce pain
- Aid corneal healing
- Maintain corneal hydration
DT was advised to use the BCL as extended wear until his next review the following day.
Over the subsequent week, the cycloplegia was ceased and there appeared to be an improvement in comfort. Under the BCL, the cornea appeared to be healing, slowly.
In the second week, it became apparent that, on removal of the BCL, the epithelium also was removed. The BCL fit was felt to be sub-optimal; it appeared too flat with not enough sag leading to excessive movement and poor bedding of the newly established epithelium.
Menicon technical services were contacted (their base is near to the practice), and they were able to provide a large diameter hydrogel bandage lens; 8.7/ 16.5 Contaperm (75% water content). This lens provided good comfort, with excellent coverage.
Over a period of weeks, the cornea appeared to heal, but every time DT spent more than two or three days without the BCL, his symptoms would return (especially on waking). Also, if he wore the lenses for extended periods of time, he would present with CLARE. The corneal appearance over time is shown in figure 4.

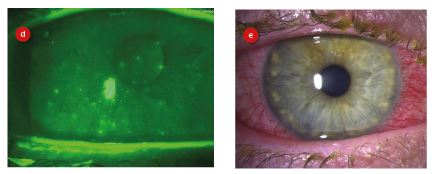 Figure 4: Corneal appearance at; (a) 14/10/28, (b) 30/10/18, (c) 29/11/18, (d) 28/01/18, (e) 11/02/19.
Figure 4: Corneal appearance at; (a) 14/10/28, (b) 30/10/18, (c) 29/11/18, (d) 28/01/18, (e) 11/02/19.
It appeared that DT had developed a recurrent or persistent epithelial defect (PED). To help with the apparent PED, 50mg doxycycline bd PO for 4/52, with gtt FML bd R for 4/52 were prescribed. This did not resolve DT’s symptoms and so alternative treatments were discussed. These included the following options:
- Anterior stromal puncture
- Alcohol delamination
- Epithelial debridement
- Diamond burr polish
- Phototherapeutic keratectomy
DT was reluctant to try any of these.
In June of 2019, DT was directed to try one drop of Cacicol every other day for five instillations. Figure 5 shows the corneal appearance after three months. At the time of writing this case record, DT has not returned with further complication.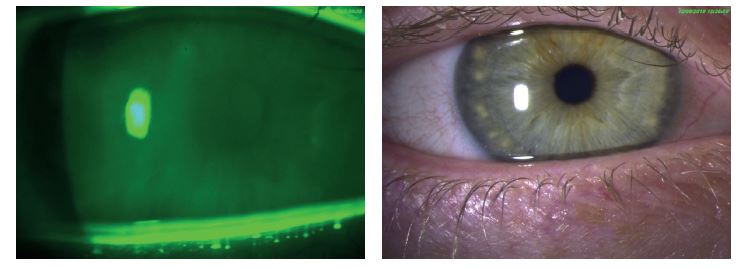 Figure 5: Appearance of cornea three months after the introduction of Cacicol; (a) blue light and fluorescein, (b) white light.
Figure 5: Appearance of cornea three months after the introduction of Cacicol; (a) blue light and fluorescein, (b) white light.
Although we have had limited experience with Cacicol, this case reports joins the growing bank of case reports suggesting an RGTA to be a suitable and effective option for patients who have been suffering persistent epithelial defects and who are not ready for surgical intervention.
Dr Keyur Patel is a therapeutic optometrist working in independent practice in Northampton.
References
- Barritault D, et al.. RGTA or ReGeneraTing Agents mimic heparan sulfate in regenerative medicine: from concept to curing patients. Glycoconjugate Journal, 2016, vol 33, (5), pp 693-838
- Eming, S.A., Krieg, T., Davidson, J.M.: Inflammation in wound repair: molecular and cellular mechanisms. J. Invest. Dermatol. 127(3), 514–25, 2007
- Ikeda, Y et al. Synthesis and biological activities of a library of glycosaminoglycans mimetic oligosaccharides. Biomaterials 32(3), 769–76, 2011
- Bonini S, Rama P, Olzi D, Lambiase A. Neurotrophic keratitis. Eye (Lond) 2003; 17 (8): 989-995
- Jeng BH. Treating the nonhealing epithelial defect. Cataract Refract Surg Today Europe 2011; 25-28
- College of Optometrists Clinical Management Guidelines. www.college-optometrists.org/guidance/clinical-management-guidelines/recurrent-corneal-epithelial-erosion-syndrome.html (accessed October 2019)
- De Monchy, I et al. (2012). Management of herpes zoster neurotrophic ulcer using a new matrix therapy agent (RGTA): A case report. J Fr Ophtalmol 35, 187.e1-6
- Aifa, A et al. (2012). Topical treatment with a new matrix therapy agent (RGTA) for the treatment of corneal neurotrophic ulcers. Invest. Ophthalmol. Vis. Sci. 53, 8181–8185.
- Hughes, L et al. (2015). Novel matrix ReGeneraTing Agent promotes rapid corneal wound healing. Clin. Experiment. Ophthalmol. 43, 391–392.
- Lazreg, S. and Renault, D. The use of corneal scrubbing associated with matrix therapy in the treatment of chronic ulcers. ARVO 2017 abstract 1399.
- Kymionis, G.D et al. (2014). Combined topical application of a regenerative agent with a bandage contact lens for the treatment of persistent epithelial defects. Cornea 33, 868–872
- Maringe, E. et al. (2013). Topical treatment with a new matrix therapy agent (RGTA) in combination with limbal allograft in ocular surface desease and corneal anesthesia. Acta Ophthalmologica 91, 0–0.
- Renault, D., Lazreg, S., and Abdellah, M.B.(2015) The use of matrix therapy in the treatment of corneal perforation. Invest. Ophthalmol. Vis. Sci. 56(7), 720–720.
- Labetoulle, M et al. (2014). Effcacy of heparin sulfate mimetic polymer in Cogan’s epithelial dystrophy. Invest. Ophthalmol. Vis. Sci. 55(13), 5519–5519.
- Kymionis, G.D et al. (2015). Effect of the Regenerative Agent Poly(Carboxymethylglucose Sulfate) on Corneal Wound Healing After Corneal Cross-Linking for Keratoconus. Cornea 34, 928–931.
