The term cerebral visual impairment (CVI) is used to describe visual impairment as a result of brain damage before, during or after birth. However, the term is not exclusively used for this group of patients as brain damage can also occur later in life. The term ‘acquired brain injury’ (ABI) is used as a general term for brain damage incurred after childhood.1-3 Traumatic brain injury (TBI) is used as a term to describe injury to the brain from external force,4 such as concussion or penetrating injury. Examples of causes of non-traumatic brain injury include brain tumours, haemorrhages and stroke.
Just as in childhood CVI, ABI can lead to a wide range of visual impairments and it is important to seek these out in such patients5 as the visual aspects are often overlooked.6 In childhood CVI, visual impairment occurs before or during a time of general development and schooling. Therefore, habilitation (acquiring skills for the first time) is required. Patients with ABI usually have a memory of what the world used to look like before the injury occurred and therefore rehabilitation (adapting to the new situation) is required.
Hemianopia and hemi-inattention are features commonly seen in both childhood CVI and ABI. How does management differ in the presence of inattention? What other features may be encountered when inattention is present and how does this influence management? How does the age of the patient impact on management? These questions will be investigated by way of the various scenarios described in this article.
Visual Pathways
When assessing a patient, one needs to establish, whether the hemianopia is accompanied by inattention as this will impact on compensation strategies. Figure 1 shows a diagram of the visual pathways from the eyes to the primary visual cortex. The visual field defects are indicated as they correspond to the location of the lesion. For example, lesions of the occipital lobes tend to produce congruous homonymous hemianopia without inattention.7
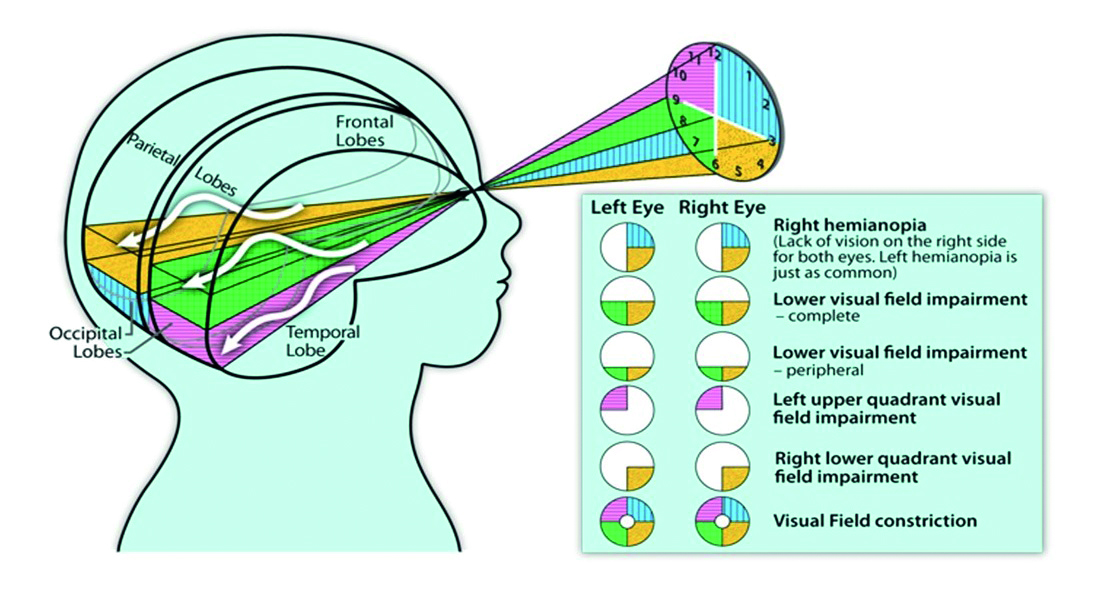
Figure 1: Visual pathway from eyes to primary cortex: a homonymous map through a ‘cyclopian eye’ 8
In contrast, lesions in the higher processing pathways tend to result in inattention, which means that the person is unlikely to pay any attention to that side of the body. Functional fields are assessed with both eyes open (figure 2), as described in the second article in this series (see Optician 10.05.19).

Figure 2: Functional field assessment with both eyes open
Scenario 1
This first scenario serves as an example of managing hemianopia due to a lesion in the primary pathway in childhood.
A girl in her early teens attended the Low Vision clinic with a history of right-sided hemianopia and profound hearing loss on the left side due to a tumour (grade 1 pilocytic astrocytoma) in her left temporal lobe. The mass had affected the left lateral ventricle and the circle of Willis and caused the chiasm to be displaced anteriorly (figure 3). She had undergone radiotherapy and chemotherapy, both of which aimed to control the tumour and preserve visual function and her condition had been stable for a couple of years since.
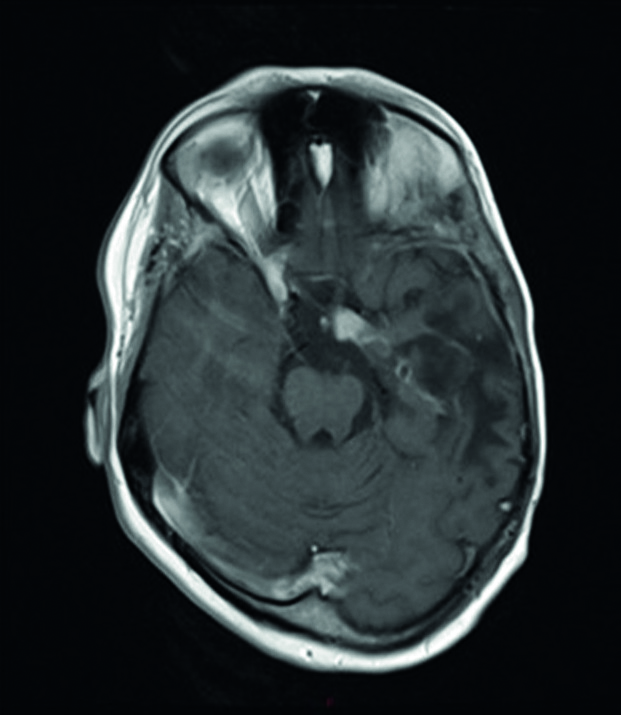
Figure 3: MRI scan for scenario 1. Tumour removed from left temporal lobe; involvement of optic tract and chiasm
Dislocation of the chiasm often leads to visual field abnormalities. The visual fields from a week prior to this visit can be seen in figure 4. Functional fields assessment confirmed a right hemianopia without inattention. Her best corrected vision was 0.10 logMAR and N8 in the right eye and 0.30 and N12 in the left eye. Left temporal lobe lesions can cause object agnosia, shape agnosia and alexia. 9 This girl has had difficulties naming objects and shapes since the tumour was initially diagnosed, but this has become less severe over time. She compensated by describing objects when she could not remember their name.

Figure 4 Visual fields (Octopus) for scenario 1, one week prior to the assessment, revealing a right-sided hemianopia
Her hemianopia and hearing impairment impacted upon access to information, both in terms of reading and in terms of ideal position in the classroom. It also impacted on mobility and visual search. Furthermore, Zihl and Dutton described the likely impact of visual impairment on social interaction,10 and these aspects will now be discussed along with some interventions.
Access to information: classroom set-up
This patient had just started mainstream high school. Compared to primary school, she found it harder to follow the lessons. Her teachers were unfamiliar with her disability and the classrooms were larger than in primary school. She needed to compensate for her right hemianopia and profound hearing loss in the left ear and wondered what the best position in the classroom would be. Is it the right-hand side (as she faces the front) in order to make full use of her seeing field on the left? Or is it the left-hand side (as she faces the front) to pick up the sounds with her right hearing aid?

Figure 5: Effect of hemianopia in classroom
A neat solution would be a voice amplifier, which connects with her hearing aid loop system. Examples of such gadgets include the Roger pen, Bellman Listening Systems and the Conversor Pro (figure 6). The gadget can be worn by the teacher or laid down on the teacher’s desk to pick up the voice (and cancel the background noise) and this sound will directly feed back to her hearing aid making it possible for her to hear the teacher’s instructions from anywhere in the classroom. The patient was advised to sit on the right-hand side of the classroom to make use of the seeing field once she had the voice amplifier.

Figure 6: Audio aids; (a) Roger pen, (b) Bellman Listening System, (c) Conversor Pro
Access to information: reading
Her reading speed was reduced compared to her peers, despite normal intelligence. This could be due to the hemianopia, but there may have been an element of alexia. It had become more problematic once required to read larger pieces of text with smaller print size. She was keen to explore compensatory strategies. With her visual field defect on the right-hand side, she found it difficult to see the next word and to gauge if she had come to the end of a line. She made searching eye movements and lost the place in the text completely. It is common for people with hemianopia to have difficulties with reading. Rowe et al11 documented this in relation to field defects after stroke. One way to overcome the problem is to rotate the text through 90º and read from top to bottom (figure 7).8 She was encouraged to try this at home. Some patients have found the use of typoscopes beneficial.11 Others have found it helpful to follow along with the finger. A bar magnifier with a reading line was found useful in clinic for this patient, and so was supplied. She has been using it daily ever since. A vertical line at the right- and the left-hand side of the column can be helpful too.
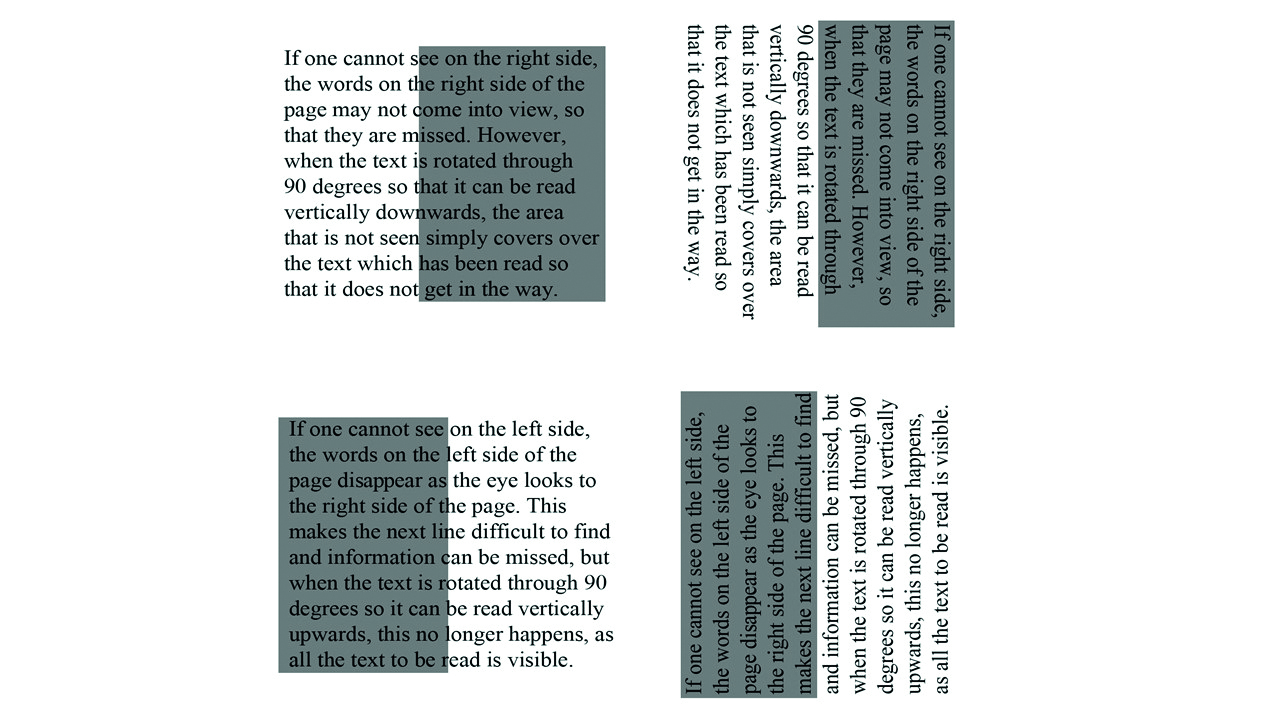
Figure 7: Reading with hemianopia 8
There are various tools and programs to explore different text presentations and improve reading speed, such as LOOK and Readright 1999-2012. All these strategies were tried and mentioned in clinic. Information was also given about mobile phone apps and local technology support services. For her computer, a Zoomtext trial disc was given.
Mobility and visual search
In terms of road safety, she was advised to move her head to scan the surroundings for visual information (particularly towards the right non-seeing side) and to listen for traffic sounds (particularly towards the left non-hearing side). Information was given about mobility training from the RNIB and ‘My Guide’. Peli prisms were briefly discussed, but she was not motivated to try these.
Around the house, some tips were given to optimise her surroundings, such as de-cluttering and adopting a systematic approach to organising toys, clothes and other items which can help to make it easier to find things. The use of contrast, lighting and highlighting was discussed as well. Frequently bumped-into door-frames could be highlighted and the family was encouraged to make sure doors are not kept half open. When out and about, the patient’s mother was used to warning her about obstacles.
Social interaction
She found team sports very challenging as she had no overview and was unable to see the balls coming. She was interested in finding out more about sports opportunities for people with a visual impairment. Information sheets were given about ‘Goalball UK’ and ‘Disability Sports’.
She was generally coping well, and did not feel the need for peer support at this time. Information about Haggeye, RNIB after school club and Blind Children UK was given to the mother in case this becomes of interest at a later stage. She had contact with her local Sensory Impairment Centre and knew that she could contact them about any other needs.
A report was sent to the GP and a copy was sent to the patient and her parents, as well as to the pupil support coordinator. Contact details for Deaf Action were issued. A few months after this encounter, the girl had been linked up with a visiting teacher for the deaf and she has been provided with a (very basic) voice amplifier. Her mum is planning on getting a more advanced one (via Deaf Action) in the near future.
This case has shown that some simple adaptations can enhance learning and independence. Including the parents in the management and informing the teaching staff are key factors in assuring that this child can reach her maximum potential.
Scenario 2
This scenario serves as an example of the complex nature of parietal lobe involvement in a stroke patient and the consequences for employment.
A man in his late 40s attended for an eye examination some nine months post stroke and complained about problems with reading. He also tended to bump into things. He could not say what part of the brain had been affected, but he knew that he was missing his left visual field. He wondered if a new spectacle prescription would help. He has stopped working on a building site and is on unpaid leave as he feels unsafe in this environment now.
The UK counts over 1.2 million stroke survivors (Stroke Association 2018). Visual field impairment is common after stroke with an initial prevalence of 57% in the first month post-stroke, diminishing to 8 to 25% long term. Hemianopia accounts for two thirds of VF loss post-stroke.12 Such statistics concerning disordered primary visual processing are readily available. However, statistics on associated disorders of higher visual processing and their impact are hard to come by as this topic has yet to be fully researched. Both basic and higher visual processing dysfunction can have a serious impact on quality of life (QoL) and functioning.11,13,14 It can also lead to negative economic impact in the working age group. Stroke survivors in the working age population are two to three times more likely to be unemployed eight years post-stroke (Stroke Association 2018).
The optometrist confirmed left homonymous hemianopia with increased visual field with left body-turn, which is in keeping with a right posterior parietal lobe lesion (figure 8).15 A right posterior parietal lobe lesion tends to result in significant lack of attention on the left side and intermittent inattention on the right side.17 It is therefore not surprising that this man frequently bumped into lamp posts, wheelie bins and people, particularly on the left side. He also noticed difficulty with reading since the stroke. This is a common problem and is usually related to low vision, eye movements and field impairment post-stroke.3 This man’s vision was reduced to 0.76 logMAR (6/36) and N16 in the right eye and 0.50 (6/19) and N10 in the left eye.

Figure 8: MRI scan for scenario 2: Stroke affecting right parietal lobe. This image was taken shortly after the stroke occurred
The various interventions we employed were as follows:
Mobility
First of all, explanation was given about the need of a body-turn, rather than an eye-turn or head turn for complete scanning of his surroundings. Specific coping strategies were discussed (table 1). On a subsequent visit, he was tried with Peli prisms to alert him about obstacles on the left. Peli prisms have been found to improve the detection of blind-side hazards 17 and obstacle avoidance.18 The principle of a Peli prism is to superimpose an image from the blind side at the top and bottom of the seeing side in one eye by using a base out prism on the spectacle lens of the hemianopic side. In the author’s experience, these prisms only work in a select group of patients and it is essential that the patient fully understands the principles of its use for it to be successful. This man found it helpful and stated a few weeks later that he had fewer collisions since he was fitted with the Peli prisms. He used them successfully until he had an epileptic fit three months later.
Reading
This patient had difficulties finding the beginning of the next line due to the left hemianopia. His reading speed was also slowed down due to his reduced vision. Various magnifiers were tried and different reading strategies were discussed (table 1).
Driving, registration and employment
In the UK, people with hemianopia are not eligible to drive and this man was advised accordingly. Hemianopia qualifies a person to be registered as Sight Impaired (Dementia and Disabilities Unit, 2017). For registration, a referral to an ophthalmologist is indicated. The ophthalmologist certifies the patient as sight impaired (SI) or severely sight impaired (SSI) and the social services register the patients. Visually impaired people who are in employment are protected through the Equality Act (UK Government 2013).
Support for stroke patients varies widely across the country. As this patient lived outside the catchment of the stroke unit near the eye hospital, his referral was delayed as the author needed to find out what services were available in the patient’s own area. He was also referred to an employment service from the RNIB. However, before he got to these places, he had a major set-back.
Follow-up
After six months, he had an epileptic episode, for which he was hospitalised for several weeks. When he came back to the Low Vision clinic, his logMAR acuity had dropped to 1.68 either eye and 1.08 binocularly. Although no brain scan was available, his symptoms suggested that further brain damage had occurred as follows:
Simultanagnosia/ field impairments
He had now lost the ability to see an entire scene despite the ability to see single elements (simultanagnosia). For example, he could not scan in traffic situations or search for items on a shelf or in a cupboard or fridge. He reported accidentally pouring juice into his coffee when he thought he had picked up the milk from his fridge. Searching for items around the house, such as the remote control, had become a real challenge. He also could not cope in environments where several conversations are happening at once. Sitting in a waiting room with people talking made him feel very uncomfortable. He reported frequent meltdowns as a result of daily frustrations. Bumping into objects has become a hazard and has caused him to avoid busy places, such as supermarkets. In his own home, he bumped into furniture and fell over objects on the floor. His inferior field was severely impaired to the extent that he did not process any visual information below waist level. He frequently knocked over cups, glasses, bottles or anything else on the table. He failed to realise that there was more food on the table or on his plate and instead thought he had served himself a rather tiny portion when his plate was, in fact, still half full. Only when he started clearing the table did he realise that there was still more food on the table or on his plate (seeing it from a different angle).
Dyskinetopsia
He could not see fast moving traffic or a ball rolling towards him when he tried to play with his grandson. He often got a fright when something popped out of nowhere.
Dorsal stream dysfunction
He experienced great difficulty with floor boundaries and patterned carpets and needed to feel the ground ahead of him. He could no longer accurately reach for objects and needed to feel his way around. He also found it difficult to concentrate and stay on task.
Other features
He got lost in (previously) familiar places (topographic agnosia). He was also getting visual hallucinations and sometimes continued to ‘see’ things that he was no longer looking at.
The deterioration of his functioning has led to voluntary redundancy from his job. He missed the daily routine and now suffered from depression, anxiety, sleeplessness and loneliness. He wondered if he could get support to deal with his emotions and to implement meaningful volunteering in his last work place.
Interventions
The focus of this appointment was to characterise the impairments so that it could be explained to the patient. Understanding the CVI empowers patients to develop compensation strategies. The compensation strategies from the first visit were reinforced and new strategies were discussed. For example:
- The use of a balloon (slow moving) or a ball with a bell when playing with his grandson; search strategies and further de-cluttering
- The use of a penfriend to find objects in a cupboard
- Tactile guidance was further explained and he was encouraged to use a cane or hiking pole.
During this appointment, he was registered as SSI, which entitled him to more support. The RNIB was asked to arrange a social care assessment and benefits check. The RNIB also arranged counselling to deal with the negative emotions. Furthermore, the RNIB offered support in establishing structured volunteering in his last work place. His GP was also informed about his anxiety, loneliness, sleeplessness and stress and asked to further assess this.
As we have seen from this case, stroke and epilepsy can have a serious impact on a person’s functioning. Furthermore, the optometrist needs to be prepared to deal with the changing needs if a condition changes and leads to further visual loss. Initially, some simple advice along with magnifiers and a Peli prism were helpful and appropriate. As his visual functioning deteriorated, the focus was more on rehabilitation strategies, financial support, emotional support and developing an understanding about his condition.
Back to the community optometrist
This article has shown that hemianopia and hemi-inattention cannot be managed with a ‘one fits all’ approach as the needs of each individual patient are unique. Many factors play a role in each person’s life. In children, the focus is often the school environment and the involvement of the parents and carers who support the child in learning and developing. In people of working age, the implications can be financial and social. Elderly patients may benefit from their carer’s understanding of the condition in order to plan adaptations to their living environment. Severity of visual impairment and visual dysfunction varies widely and a person’s needs can change depending on changes in clinical picture or other life changes. The optometrist can play a role in offering strategies and by getting familiar with local referral pathways and charities.
Cirta Tooth is a hospital optometrist based in Edinburgh with a special interest is low vision and functional vision.
Acknowledgements
- Figures 1 and 7 were reproduced from: Lueck, Amanda H.; Dutton, Gordon N. (Eds.) (2015). Vision and the Brain: Understanding Cerebral Visual Impairment in Children. New York: AFB Press (with permission from Dutton GN.)
- The patients that are described have given their permission to be included in this publication and consent has been obtained from the NHS for the release of data
References
- Gottlieb, D.D. et al. 1998. Neuro-optometric facilitation of vision recovery after acquired brain injury. Neurorehabilitation 11(3), pp. 175-199
- Edmans, J. 2009. Vision, perception and cognition: a manual for the evaluation and treatment of the adult with acquired brain injury. British Journal of Occupational Therapy 72(9), p. 415
- Rowe, F.J. et al. 2011. Reading difficulty after stroke: ocular and non ocular causes. International Journal of Stroke 6(5), pp. 404-411
- Armstrong, R.A. 2018. Visual problems associated with traumatic brain injury. Clinical and Experimental Optometry 101(6), pp. 716-726
- de Vries, S.M. et al. 2018. Screening of visual perceptual disorders following acquired brain injury: a Delphi study. Applied Neuropsychology- Adult 25(3), pp. 197-209
- Berthold-Lindstedt, M. et al. 2017. Visual dysfunction is underestimated in patients with acquired brain injury. Journal of Rehabilitation Medicine 49(4), pp. 327-332
- Kedar et al. 2007. Congruency in homonymous hemianopia. American Journal of Ophthalmology 143(5), pp. 772-780
- Lueck, Amanda H.; Dutton, Gordon N. (Eds.). 2015. Vision and the Brain: Understanding Cerebral Visual Impairment in Children. New York: AFB Press.
- Dutton, G.N. 2015. Disorders of the brain and how they can affect vision. In book: Lueck, A.H. and Dutton, G.N. 2015. Vision and the Brain: Understanding Cerebral Visual Impairment in Children (p78). New York: AFB Press.
- Zihl, J. And Dutton, G.N. 2015. Cerebral Visual Impairment in Children. Wien: Springer-Verlag.
- Rowe, F.J. et al. 2013. A prospective profile of visual field loss following stroke: prevalence, type, rehabilitation and outcome. Biomedical Research International Article number: 719096
- Bunce, C. et al. 2017. Sight Impairment registration due to stroke—A small yet significant rise? Brain and Behaviour 7.
- Gall, C. et al. 2010. Vision-related quality of life in first stroke patients with homonymous visual field defects. Health and Quality of Life Outcomes 8, Article number 33
- Sand, K.M. et al. 2016. Vision problems in ischaemic stroke patients: effects on life quality and disability. European Journal of Neurology 23. Special issue. Supplement 1, pp. 1-7
- Roberson G. Visual fields – 1. Defects caused by neurological disease. OPTICIAN 09.08.19.
- Ting, T.S.J. et al. 2011. Visual neglect following stroke: Current concepts and future focus. Survey of Ophthalmology 56(2), pp. 14-134.
- Houston, K.E. et al. 2018. Driving with hemianopia VI: peripheral prisms and perceptual-motor training improve detection in a driving simulator. Translational Vision Science and Technology 7(1), Article Number 5.
- Bowers, A.R. et al. 2014. Randomized crossover clinical trial of real and sham peripheral prism glasses for hemianopia. Journal of the American Medical Association Ophthalmology 132(2), pp. 214-222
