As healthcare providers, we should care not only about prescribing for a patient today, but we should pay attention to their long-term visual health. This is apropos when it comes to myopia. We all strive to provide a myopic patient with an optimal correction and offer multiple options be they spectacles, contact lenses, or surgical, but for young myopes we can now do so much more.
Background
There is growing interest in myopia and its control among optometrists and other eye care professionals. This arises from a number of factors. First, the prevalence of myopia is increasing around the world. It is predicted that by the year 2050, over half of the world’s population will be myopic.1 We already see prevalences of 80% and above in Taiwan and Japan.2 In the United Kingdom, the proportion of myopic children has doubled in the past 50 years.3 Furthermore, a recent study of the 1958 British birth cohort found that 49% of these individuals in their early forties were myopic.4 Second, we have become more and more aware of the sight-threatening consequences of higher levels of myopia,5 something that will be explored at length below. And finally, there is a growing body of evidence that we can slow myopia through a variety of clinical therapies including multifocal soft contact lenses,6,7 overnight orthokeratology,8 atropine,9 spectacles10 and increased time outdoors.11 In the United Kingdom, three different soft contact lenses have a CE mark for myopic control along with one overnight orthokeratology lens. Trials are ongoing of low concentration atropine which has been shown to slow myopia progression, although the ideal concentration is far from clear.12
Some sceptics may say myopia is myopia, has always been myopia, and trying to slow its progression is of little interest and has little benefit to the patient. Indeed, the College of Optometrists stated in their recent consensus statement:
‘There is... very little evidence about the long-term benefits and risks of the myopia control treatments available, or the effect on myopia progression following the cessation of treatment.’ (www.college-optometrists.org/the-college/policy/myopia-man- agement.html)
This perspective likely reflects that the field of myopia control is evolving rapidly with most of the evidence for its effectiveness having been published in the past decade. Our thinking needs to align with awareness of the public health issues and the increasing availability of treatment options, but what exactly are the benefits of myopia control?
Benefits of myopia management
Earlier this year my colleague Noel Brennan and I published an article in which we articulated three broad benefits of lowering a patient’s ultimate level of myopia.13
First, with less myopia, a patient is less visually disabled when not wearing their correction.14,15 As an ageing male, I find myself needing to visit the bathroom more frequently in the middle of night. As a 2-dioptre myope this is not particularly difficult, even when I am in an unfamiliar hotel room. A higher myope faces greater challenges because of their poorer uncorrected vision. Furthermore, there is a growing body of evidence documenting the relationship between degree of uncorrected myopia and reduced vision-related quality of life.16 We also know that higher myopes are more reliant on their correction and may take greater risks when it comes to wearing contact lenses, ignoring discomfort and redness.17 It is also important to note that even when corrected, the higher the myopia, the poorer the vision quality. We have documented that higher myopes have, on average, about a half line poorer visual acuity then low myopes. This cannot be explained completely by vertex distance and spectacle magnification. Higher myopes also suffer from poorer cosmesis when it comes to their spectacles. Not only will the spectacle lenses be thicker and heavier, but their eyes look smaller and less attractive due to their higher powered lenses.
Second, it is important to remember that the myopic child of today is the refractive surgery candidate of tomorrow. Our refractive surgery colleagues have a cliché that ‘the shorter putt is easier to sink’. In essence, they are saying that outcomes are better at lower levels of myopia and this has been documented frequently in the literature. The lower a patient’s myopia, the less residual refractive error they will, on average, experience following the procedure.
Less residual refractive error means better uncorrected visual acuity and less need for further surgical enhancements or touch-ups. Also, we have demonstrated that the vision quality after refractive surgery is better with lower levels of myopia.18 While high contrast visual acuity may be excellent even at high levels of myopia, low contrast visual acuity at lower light levels when the pupil dilates can be significantly poorer in patients with higher preoperative levels of myopia. Finally, higher myopes may have fewer options when it comes to the type of refractive surgery for which they are eligible. LASIK and other ablative procedures require a minimum amount of corneal thickness to ensure post-operative stability and to minimise the likelihood of corneal ectasia.19 Of course, the higher the myopia, the greater the amount of corneal tissue that needs to be removed. Thus, the patient with higher myopia, thinner corneas, or both will have limited options and may need to seek alternative surgical procedures such as phakic intraocular lenses and with their increased risks of complications associated with invasive ocular surgery.
High levels of myopia have long been associated with increased risks of ocular disease and these include cataract, glaucoma, and retinal detachment.20-22 Nonetheless, the greatest myopia-related cause of vision loss is myopic macular degeneration, which is also referred to as myopic retinopathy or myopic maculopathy. This particular retinal condition has no known treatment and is characterised by stretched blood vessels, atrophy around the optic nerve head, staphyloma, lacquer cracks in Bruch’s membrane, geographic atrophy of the retinal pigment epithelium and choroid, retinal haemorrhages, and ultimately choroidal neovascularisation.
Myopia and ocular diseases
Of course, the sight-threatening complications occur later in life, but the underlying myopia develops during childhood. Fricke et al23 recently estimated that 10 million people had visual impairment from myopic maculopathy in 2015 of whom 3.3 million were legally blind. By 2050, visual impairment will grow to 55.7 million (1 in 175), 18.5 million of whom will be blind. The risk of myopic maculopathy and its impact on public health are not limited to high myopes. In fact, myopes below 5 D contribute half of the cases of myopic maculopathy.24 Thus, myopia control has the potential to reduce the risk of widespread visual impairment in myopes.
In our recent publication,13 we reanalysed data from five large population-based studies of the prevalence of myopic maculopathy.24-28 Collectively, these studies represent data on over 20,000 patients, mostly 50 years and above. Figure 1 shows the prevalence as a function of degree of myopia. Each paper presented data for various ranges of myopia, so in constructing this figure the midpoint of each range was used. On the left, the figure shows prevalence or frequency as a function of level of myopia. The relationship is exponential, with pronounced increases at higher levels of myopia. When the exponential curves are replotted on a logarithmic scale, they have a very striking similarity. Data from all five studies are well fit by straight lines with a slope of around 1.67x per dioptre. It is really quite remarkable that data from five studies across three continents could have nearly identical trajectories. This 1.67 slope can be translated into the statement that ‘each dioptre is associated with a 67% increase in the prevalence of myopic maculopathy.’ Restated, each dioptre less of myopia is associated with a 40% reduction in the frequency of myopic maculopathy. A reasonable assertion is that, for every dioptre myopia we could prevent, we could lower the frequency of myopic maculopathy by 40%. Given that these lines are straight, this benefit accrues regardless of the level of myopia. So, whether a patient is destined to be a -7 or a -4 myope, slowing their progression by one dioptre during childhood should lower the risk of myopic maculopathy by 40% in both cases.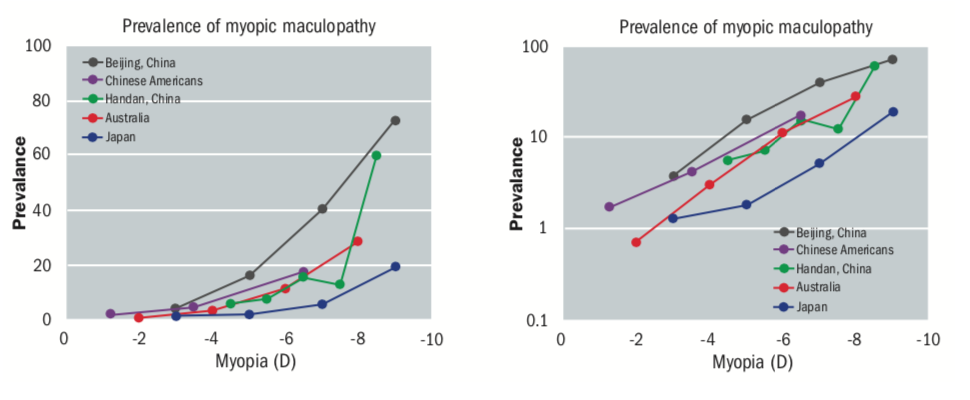
Figure 1: The prevalence of myopic maculopathy as a function of myopia plotted with both linear (left) and logarithmic (right) scales. The logarithmic scale emphasizes the similar trajectory of each dataset, the additional 67% risk associated with each dioptre
These analyses can be repeated on the other published data sets. Figure 2 shows the relation between the frequency of cataract, glaucoma and retinal detachment and myopia. For example, when the prevalence of posterior subcapsular cataract is plotted as a function of the level of myopia, we can see that the slopes of these lines at close to 1.2x. In other words, each additional dioptre of myopia increases the frequency of this particular type of cataract by 20%.29-32 For primary open-angle glaucoma, the prevalence again increases by around 20% for each additional dioptre of myopia.33-36 Finally, the incidence of retinal detachment increases by 30% for each dioptre of myopia.37,38
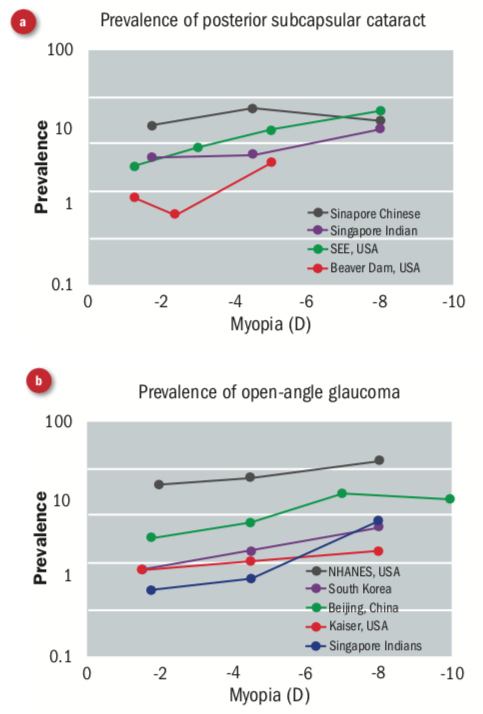
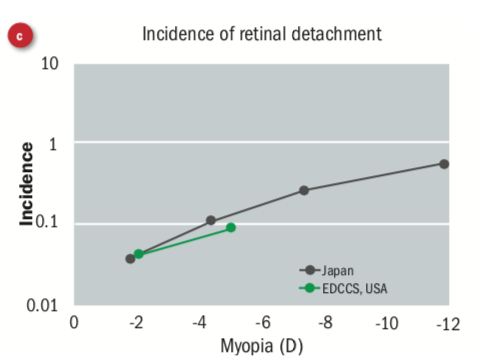
Figure 2: The relation between level of myopia and the prevalence of (a) posterior subcapsular cataract, (b) the prevalence of primary open-angle glaucoma, and (c) the incidence of retinal detachment. The logarithmic scale emphasizes the additional risk associated with each dioptre
This approach can be also be applied to data on visual impairment. Figure 3 shows data from a cluster of population studies in the Netherlands.39 The cumulative risk of visual impairment is plotted as a function of level of myopia for patients aged 75 years and above. Again, the data follows an exponential function, that is rendered linear by converting to a logarithmic scale. The slope of this line is around 1.25x. In other words, each dioptre increase of myopia is associated with a 25% increase in risk visual impairment. Turning that around again, each dioptre that we could prevent might lower the risk of visual impairment by 20%. This would be a huge public health benefit.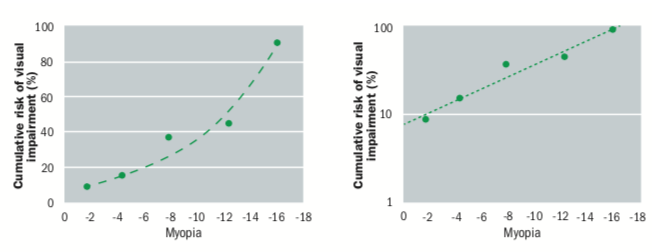
Figure 3: The prevalence of visual impairment as a function of myopia plotted with both linear (left) and logarithmic (right) scales. The logarithmic scale emphasizes the additional 25% risk associated with each dioptre
We do not have much long-term data for myopia control, but there is strong evidence that 1 D of slowing is achievable. 9,40,41 Collectively, the above body of work demonstrates the increasing frequency of eye disease and visual impairment associated with each additional dioptre of myopia. These data are summarised in figure 4. In his seminal paper, Ian Flitcroft encouraged us to the rethink the common terminology of physiological myopia.42 The above data support his assertion that there is no safe level of myopia that does not carry an increased risk of ocular disease. Nonetheless, it is important to acknowledge that not all eye disease is associated with myopia. One common error is the statement that myopia increases the risk of age-related macular degeneration (AMD). If anything, increasing myopia is associated with a decrease in the risk of AMD.43 Likewise, the frequency of diabetic retinopathy is lower in higher myopes.44,45
Table 1
Now a sceptic might say that we need to first conduct studies demonstrating that lowering the level of myopia has these long- term health benefits. Such studies will never be conducted, because we would need to intervene in children and then measure any benefit that will be accrued in later life. The time span between intervention and benefit is 50 to 70 years and even the youngest and most optimistic among us will not be around to see those results. I believe that it is a reasonable inference to take the association between level of myopia and serious eye disease and to infer that the frequency of disease can be lowered by controlling a child’s ultimate level of myopia. The analogy I use is that if when a patient walks into the consulting room with wet shoes and trousers and carrying an umbrella, it is a reasonable inference that it is raining outside. We do not need to go outside to establish this.
Practitioners who are interested in incorporating myopia interventions into their clinical practice will have questions, for example, regarding the assessment, fitting and follow-up of myopia control contact lenses and how the process might differ from that for conventional contact lenses. While the fitting of myopia control contact lenses is similar to conventional adult soft lens fitting, some clinicians express reservations about fitting younger children. Children eight years and younger can manage contact lenses,46 although it always will depend on the child and their parents. Soft contact lens wear in young children is safer than in adults, so there should be no increased concern about infections and less serious adverse events.47
Practitioners who want to understand more about myopia and myopia control should access the International Myopia Institute white papers on the topic. These were published in Investigative Ophthalmology & Visual Science and are available for free.48 Summaries of the comprehensive reports can also be found elsewhere (www.myopiainstitute.org). Researchers based in the United Kingdom and Ireland account for around 10% of the contributors to this impressive body of work, supplemented by a few expatriates.
Indeed, UK optometry has a long history of myopia research and have twice hosted the International Myopia Congress. Aston University was a clinical site for the pivotal MiSight clinical trial,7 and several institutions are participating in ongoing investigations of the effectiveness of low concentration atropine for myopia control. A number of the stars of UK myopia are featured in the British Contact Lens Association’s Myopia Management Certificate series, so there is no shortage of expertise and education available. So now that you know the benefits of myopia control and where to earn more, why not step out of your comfort zone and make 2020 the year when you become more involved in myopia management? There are few more effective ways to grow your practice than to take good care of children. Make a difference and you will have them and the rest of the family for life.
Dr Mark Bullimore is adjunct professor at the University of Houston College of Optometry.
Disclosures
Mark Bullimore is a consultant for a number of companies including Alcon Laboratories, Inc (Fort Worth, TX, USA); CooperVision, Inc (Victor, NY, USA); Essilor of America (Dallas, TX, USA); Eyenovia, Inc (New York, NY, USA); Genentech, Inc. (San Francisco, CA, USA); Johnson & Johnson Visioncare, Inc (Jacksonville, FL, USA); Novartis Pharma AG (Basel, Switzerland).
References
- Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036-42.
- Lin LL, Shih YF, Tsai CB, et al. Epidemiologic study of ocular refraction among schoolchildren in Taiwan in 1995. Optom Vis Sci 1999;76:275-81.
- McCullough SJ, O’Donoghue L, Saunders KJ. Six Year Refractive Change among White Children and Young Adults: Evidence for Significant Increase in Myopia among White UK Children. PLoS One 2016;11:e0146332.
- Rahi JS, Cumberland PM, Peckham CS. Myopia over the life- course: prevalence and early life influences in the 1958 British birth cohort. Ophthalmology 2011;118:797-804.
- Verkicharla PK, Ohno-Matsui K, Saw SM. Current and predicted demographics of high myopia and an update of its associated pathological changes. Ophthalmic Physiol Opt 2015;35:465-75.
- Cheng X, Xu J, Chehab K, et al. Soft Contact Lenses with Positive Spherical Aberration for Myopia Control. Optom Vis Sci 2016;93:353-66.
- Chamberlain P, Peixoto-de-Matos SC, Logan NS, et al. A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci 2019;96:556-67.
- Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trialized Clinical Trial. Invest Ophthalmol Vis Sci 2012;53:7077-85.
- Chua WH, Balakrishnan V, Chan YH, et al. Atropine for the treatment of childhood myopia. Ophthalmology 2006;113:2285-91.
- Cheng D, Woo GC, Drobe B, Schmid KL. Effect of Bifocal and Prismatic Bifocal Spectacles on Myopia Progression in Children: Three-Year Results of a Randomized Clinical Trial. JAMA Ophthalmol 2014.
- Wu PC, Chen CT, Lin KK, et al. Myopia Prevention and Outdoor Light Intensity in a School-Based Cluster Randomized Trial. Ophthalmology 2018;125:1239-50.
- Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (LAMP) Study: A Randomized, Double-Blinded, Placebo-Controlled Trial of 0.05%, 0.025%, and 0.01% Atropine Eye Drops in Myopia Control. Ophthalmology 2019;126:113-24.
- Bullimore MA, Brennan NA. Myopia Control: Why Each Dioptre Matters. Optom Vis Sci 2019;96:463-5.
- Atchison DA, Smith G, Efron N. The effect of pupil size on vis- ual acuity in uncorrected and corrected myopia. Am J Optom Physiol Opt 1979;56:315-23.
- Smith G, Jacobs RJ, Chan CD. Effect of defocus on visual acuity as measured by source and observer methods. Optom Vis Sci 1989;66:430-5.
- Lamoureux EL, Saw SM, Thumboo J, et al. The impact of corrected and uncorrected refractive error on visual functioning: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci 2009;50:2614-20.
- Chalmers RL, McNally JJ, Schein OD, et al. Risk factors for corneal infiltrates with continuous wear of contact lenses. Optom Vis Sci 2007;84:573-9.
- Bailey MD, Olson MD, Bullimore MA, et al. The effect of LASIK on best-corrected high-and low-contrast visual acuity. Optom Vis Sci 2004;81:362-8.
- Twa MD, NicholsJJ, Joslin CE, et al. Characteristics of corneal ectasia after LASIK for myopia. Cornea 2004;23:447-57.
- Hsu WM, Cheng CY, Liu JH, et al. Prevalence and causes of visual impairment in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology 2004;111:62-9.
- Iwase A, Araie M, Tomidokoro A, et al. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology 2006;113:1354-62.
- Liang YB, Friedman DS, Wong TY, et al. Prevalence and causes of low vision and blindness in a rural chinese adult population: the Handan Eye Study. Ophthalmology 2008;115:1965-72.
- Fricke TR, Jong M, Naidoo KS, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol 2018;102:855-62.
- Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology2002;109:704-11.
- Liu HH, Xu L, Wang YX, et al. Prevalence and progression of myopic retinopathy in Chinese adults: the Beijing Eye Study.Ophthalmology 2010;117:1763-8.
- Gao LQ, Liu W, Liang YB, et al. Prevalence and characteristics of myopic retinopathy in a rural Chinese adult population: the Handan Eye Study. Arch Ophthalmol 2011;129:1199-204.
- Asakuma T, Yasuda M, Ninomiya T, et al. Prevalence and risk factors for myopic retinopathy in a Japanese population: the Hisayama Study. Ophthalmology 2012;119:1760-5.
- Choudhury F, Meuer SM, Klein R, et al. Prevalence and Characteristics of Myopic Degeneration in an Adult Chinese American Population: The Chinese American Eye Study. Am J Ophthalmol 2018;187:34-42.
- Pan CW, Cheung CY, Aung T, et al. Differential associations of myopia with major age-related eye diseases: the Singapore Indian Eye Study. Ophthalmology 2013;120:284-91.
- Chang MA, Congdon NG, Bykhovskaya I, et al. The association between myopia and various subtypes of lens opacity: SEE (Salisbury Eye Evaluation) project. Ophthalmology 2005;112:1395-401.
- Wong TY, Foster PJ, Johnson GJ, Seah SK. Refractive errors, axial ocular dimensions, and age-related cataracts: the Tanjong Pagar survey. Invest Ophthalmol Vis Sci 2003;44:1479- 85.
- Wong TY, Klein BE, Klein R, et al. Refractive errors and incident cataracts: the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci 2001;42:1449-54.
- Shen L, Melles RB, Metlapally R, et al. The Association of Refractive Error with Glaucoma in a Multiethnic Population. Ophthalmology 2016;123:92-101.
- Qiu M, Wang SY, Singh K, Lin SC. Association between myopia and glaucoma in the United States population. Invest Ophthalmol Vis Sci 2013;54:830-5.
- Chon B, Qiu M, Lin SC. Myopia and glaucoma in the South Korean population. Invest Ophthalmol Vis Sci 2013;54:6570-7.
- Xu L, Wang Y, Wang S, et al. High myopia and glaucoma susceptibility the Beijing Eye Study. Ophthalmology 2007;114:216-20.
- Risk factors for idiopathic rhegmatogenous retinal detachment. The Eye Disease Case-Control Study Group. Am J Epidemiol 1993;137:749-57.
- Ogawa A, Tanaka M. The relationship between refractive errors and retinal detachment-analysis of 1,166 retinal detachment cases. Jpn J Ophthalmol 1988;32:310-5.
- Tideman JW, Snabel MC, Tedja MS, et al. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol 2016;134:1355- 63.
- Hiraoka T, Kakita T, Okamoto F, et al. Long-term effect of over- night orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci 2012;53:3913-9.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Long-term Efficacy of Orthokeratology Contact Lens Wear in Controlling the Progression of Childhood Myopia. Curr Eye Res 2017;42:713-20.
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res 2012;31:622-60.
- Verhoeven VJ, Wong KT, Buitendijk GH, et al. Visual consequences of refractive errors in the general population. Ophthalmology 2015;122:101-9.
- Man RE, Gan AT, Gupta P, et al. Is Myopia associated with the Incidence and Progression of Diabetic Retinopathy? Am J Ophthalmol 2019.
- Wang Q, Wang YX, Wu SL, et al. Ocular Axial Length and Diabetic Retinopathy: The Kailuan Eye Study. Invest Ophthalmol Vis Sci 2019;60:3689-95.
- Walline JJ, Jones LA, Rah MJ, et al. Contact Lenses in Pediatrics (CLIP) Study: chair time and ocular health. Optom Vis Sci 2007;84:896-902.
- Bullimore MA. The Safety of Soft Contact Lenses in Children. Optom Vis Sci 2017;94:638-46.
- Wolffsohn JS, Flitcroft DI, Gifford KL, et al. IMI - Myopia Control Reports Overview and Introduction. Invest Ophthalmol Vis Sci 2019;60:M1-M19.
