As soon as a contact lens is placed on to the eye, it is bathed in the already complex structure of the tear film. The ability of the tear film to maintain its integrity in the presence of a contact lens is crucial for successful contact lens wear. Tear film instability can lead to deficiencies in the lens/tear interface, and the wearer reporting symptoms of dryness and discomfort, which are arguably the most common reasons for contact lens drop out.1
The importance of the tear film in maintaining comfortable contact lens wear means that the contact lens practitioner must be able to carefully and accurately assess the tears, both before and during contact lens wear. This article will review the clinical examination of the tear film in contact lens practice.
The Tear Film
The tear film plays a multifunctional role in maintaining ocular surface health; it not only protects and moisturises the cornea, but also forms the first refractive surface for light entering the eye.2 It was previously believed that the tear film comprised of three distinct layers − a mucin, aqueous and a lipid layer.3 However, newer publications, such as the DEWS II Tear Film report,2 describe the tear film as a complex blended two-layer structure, comprising of a mucoaqueous layer and an outer lipid layer (figure 1).
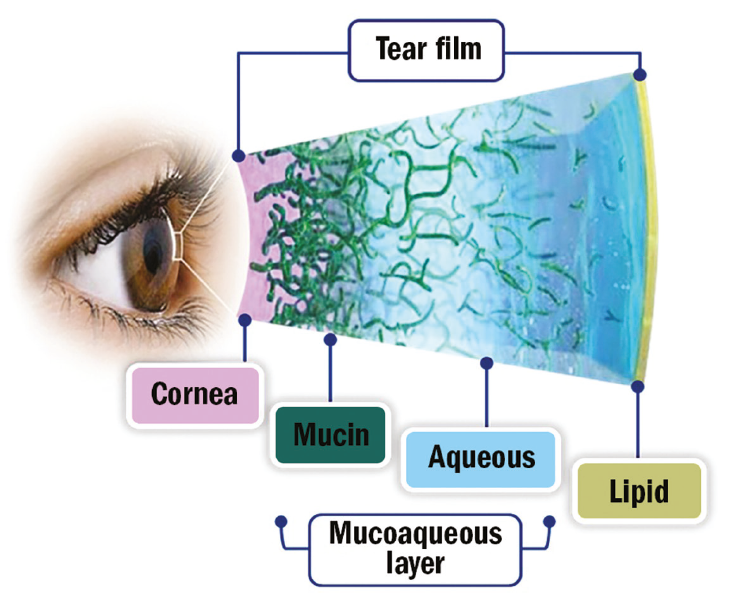
Figure 1: The structure of the tear film
This indicates that the mucin and aqueous layers are more of a continuum, with a higher concentration of mucin nearest to the ocular surface.3 It is currently understood that this complex continuum contains 20 types of mucins, approximately 1,800 proteins and other essential components such as inflammatory markers, ions, salts and electrolytes.2 Each of the different components of the tear film plays an important role (table 1); while the aqueous component provides hydration and flushes toxins, mucins bind to both lipid and water to help stabilise the tear film. The outermost lipid layer, understood to comprise at least 153 types of lipids, has the role of reducing evaporation and the surface tension of the thin film to avoid its collapse.2
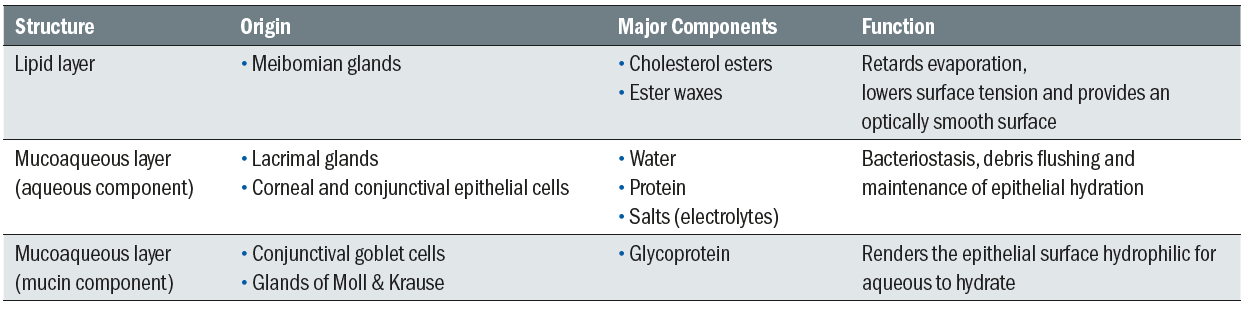
Table 1: The origins, major components and function of each structure of the tear film
Tear Film-Contact Lens Interactions
Modern soft contact lenses are estimated to be between 15-30 times thicker than the average tear film and therefore when a contact lens is inserted on the eye and becomes bathed in the tear film, it is vital that this delicate structure is maintained.
Material properties will undoubtedly play a part in the stability of the tear film, with different materials causing different interactions. For example, silicone hydrogel materials tend to deposit more lipid and less protein compared to high water content, ionic hydrogels.5 Deposits, whether protein or lipid, can affect the wettability of the contact lens and have an impact on both comfort and vision over time,4 therefore the presence of deposits should be noted and managed.
Assessing the tear film
Assessing the tear film accurately is made challenging in that it is transparent, small in volume (approximately 8µl) and relatively thin (between 2 and 5.5µm).2 Additionally, the tear reflex may be stimulated during assessment which may affect results.
Assessment of the tear film in practice can be achieved through a variety of methods. However, consistent with many aspects of contact lens practice, the slit lamp remains the instrument predominantly used by practitioners. Its high magnification and excellent optics allow detailed observation of the structures and integrity of the tear film. A keratometer, if available, can also be employed to assess tear stability by observing the clarity of the mires between blinks. With advances in dry eye diagnostic and treatment technology, more sophisticated instrumentation can be found in clinical practice which can provide invaluable information on the tear film. While mainly adopted for dry eye management, their use for a detailed analysis of the tear film in contact lens practice should also be considered. This article will consider techniques that can be easily fitted into routine eye examinations and contact lens appointments, while also considering the value of newer technology.
Tear film evaluation can be divided into two areas – assessment of tear quantity (volume) and tear quality (stability). Each shall be considered in turn.
Tear Quantity
Bearing in mind that stimulation of reflex tearing will affect any evaluations it is generally suggested to perform the least invasive techniques first. As the bright light source from the slit lamp will inevitably provoke a degree of reflex tearing, it is advisable to perform any non-invasive evaluations of quantity towards the beginning of the assessment. Measuring the inferior tear meniscus height (meniscometry) will give an indication of tear volume (figure 2). This is simple and quick to perform and can easily form part of any anterior eye examination, but is especially important during the pre-assessment of potential contact lens wearers.

Figure 2: Measurement of tear meniscus height using the slit beam width
To measure tear prism height, an illuminated slit set horizontally in alignment with the lower lid margin can be altered until it appears to match the height of the tear prism (figure 2). A value in millimetres can be obtained by using a horizontal slit beam and adjusting the slit width to match the tear meniscus height centrally along the lower lid.6 Guillon proposes a clinical routine to incorporate the measurement of the tear film prism height in these positions, enabling a more comprehensive assessment of tear volume:
- Immediately below the pupil centre
- 5mm nasally
- 5mm temporally.
It is generally accepted that a tear meniscus in normal eyes measures between 0.2 and 0.4mm.7
The above method of meniscometry depends on observer reliability, and therefore repeatability of results can vary. Newer instruments may allow a more accurate method of measuring the tear prism height by utilising reflective meniscometry to non-invasively measure the tear meniscus using integrated callipers, and has been shown to have accuracy of ±0.1mm.8 Optical coherence tomography (OCT), now widely available in optometric practice, has been recognised by the DEWS II Methodology 8 report as a quick and simple way to measure tear meniscus height (figure 3). Although it recognises that further development of validated measurement software is needed it recognises that it has shown to have good intra-observer and inter-observer repeatability.
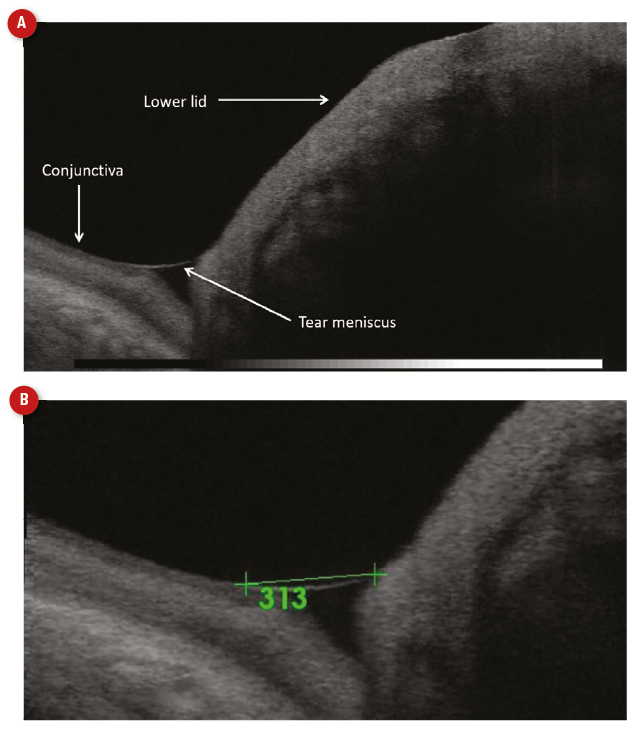
Figure 3: OCT visualisation (a) and measurement of (b) the tear meniscus height using integrated callipers
Although less commonly used in clinical practice, alternative invasive techniques for measuring tear volume include the Schirmer test and the Phenol Red Thread test.
The Schirmer test involves hooking an absorbent tear test strip of paper over the margin of the lower lid (figure 4). The length of wetting from the bend is measured in millimetres after five minutes. A normal tear film should produce a wetting length of more than 10mm. Dry eye is indicated where there is less than 5mm of wetting.10 The invasive nature of this technique results in excessive reflex tearing, limiting the value of the test in clinical practice. There appears to be a reluctance to discard this test, which is partly due to the fact that it is still the simplest, fastest and least expensive diagnostic test available for assessing tear production. DEWS II,10 while recognising the variability and invasiveness of the Schirmer test precludes it as a diagnostic test of tear quantity, recommended it as a test to confirm severe aqueous deficiency in conditions such as Sjögren’s syndrome.
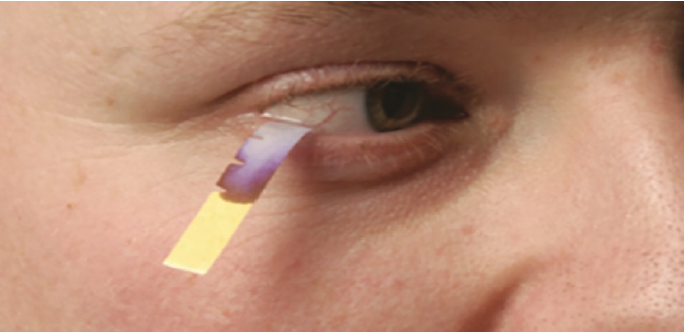
Figure 4: Schirmer Test to measure tear quantity using an absorbent strip
The Phenol Red Thread test (figure 5) has the advantage of being less invasive than the Schirmer test, utilising a two-ply cotton thread impregnated with phenol red dye. Phenol Red Thread is pH sensitive and changes from yellow to red when wetted by tears, due to the alkaline nature of tears (pH 7.6).9 The length of the colour change on the thread, indicating the length of the thread wetted by the tears, is measured in millimetres. Wetting lengths should normally be between 9mm and 20mm. Values of less than 9mm have been shown to correlate with subjective symptoms of dryness. DEWS II Methodology recognise the Phenol Red Thread test as a realistic measurement of resting tear volume.10
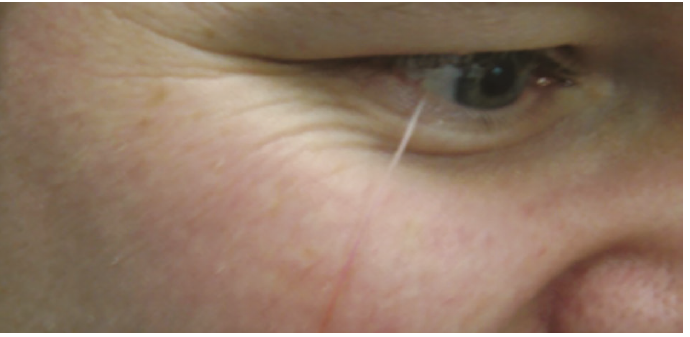
Figure 5: Phenol Red Thread test to measure tear quantity using a cotton thread with phenol red dye
Tear Quality
Tear quality can be assessed in a variety of ways. DEWS II suggests non-invasive tear break up time (NITBUT) as the preferred technique.10 This is the measurement, in seconds, of the time that elapses between the last complete blink and the appearance of the first discontinuity in the tear film. The one-position keratometer is the most commonly available instrument which can be employed to measure NITBUT in clinical practice. For measurement, the practitioner observes the keratometer mires and records the time taken from a complete blink until the mires begin to distort, and/or break up. One consideration which could affect measurement is that the keratometer is limited to assessing a small area, only providing information on tear break up in the central cornea.
Placido disc topographers, use white illumination and Placido discs to visualise the tear film. These instruments allow visibility of the majority of the corneal surface and can automatically detect and record the time of first break up (figure 6).
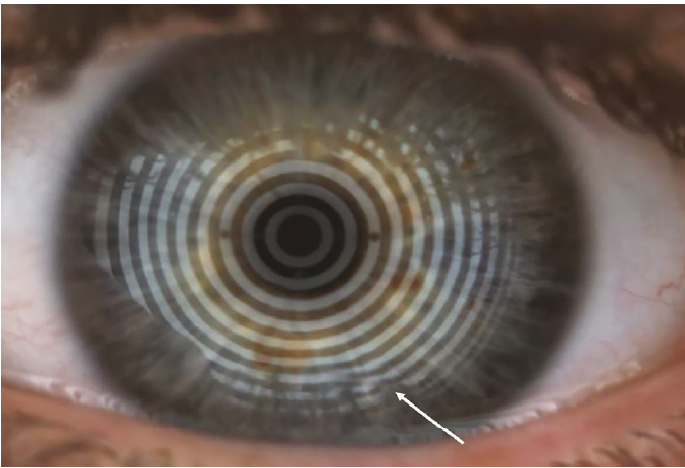
Figure 6: Assessment of NITBUT. Break up time is automatically recorded but can also be observed as break-up of the Placido rings (white arrow)
Observation of the lipid layer
The lipid layer can be viewed by utilising the technique of specular reflection on a slit lamp. Viewing the first Purkinje image with a narrow slit beam, lipid interference patterns can be observed (figure 7). As a general rule the brighter the coloured fringes appear, the thicker the lipid layer, whereas a dull, grey appearance may indicate a thinner layer. While a useful technique, the observer is limited to viewing a small area at a time, and the practitioner should be cautious that the heat of the slit lamp does not produce artificial drying.
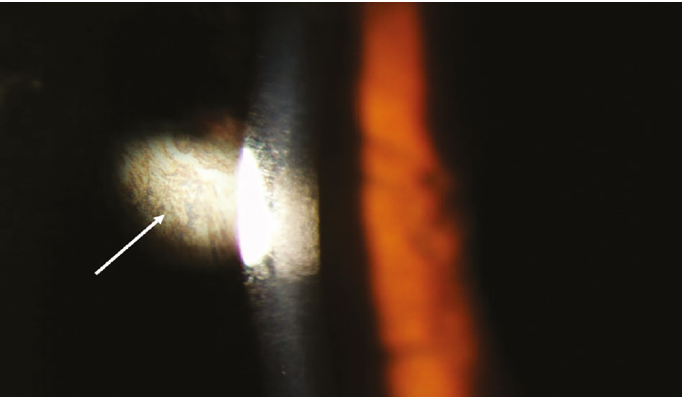
Figure 7: Observation of the lipid layer coloured fringes (white arrow) using specular reflection
Lipid layer interferometry can also be employed to assess the lipid layer thickness and many of the dry eye diagnostic devices include this feature. This is a more advanced examination method, giving practitioners an accurate and quantitative measurement of this delicate layer (figure 8), with a healthy lipid layer thought to be approximately 40nm thick.10 Considering the importance of the lipid layer in maintaining tear film stability, interferometry can be a useful tool for practitioners wanting to examine the lipid layer in greater detail.
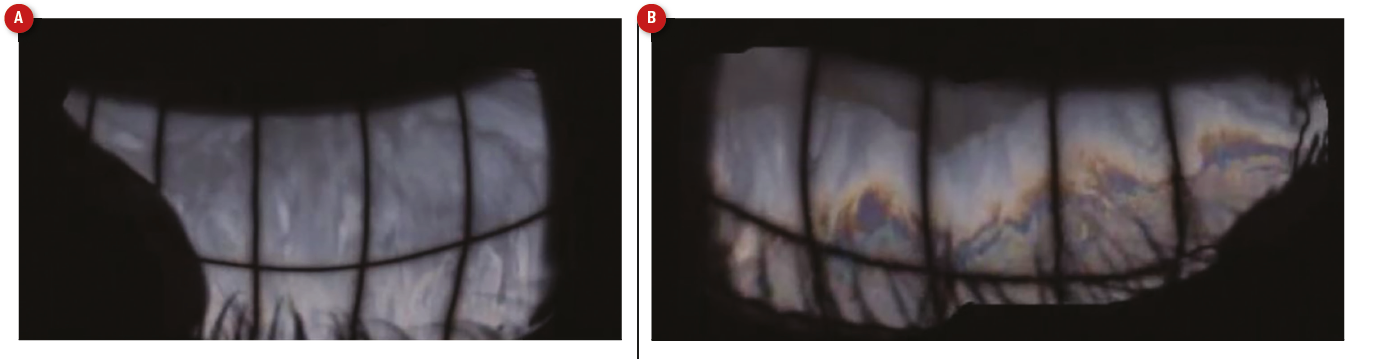
Figure 8: Examination of the lipid layer using interferometry. Few coloured fringes can be seen when the lipid layer is thin (a) compared to when it is thicker (b)
Fluorescein Tear Break Up Time
Traditionally, tear break-up time has been measured by staining the ‘transparent’ tears with fluorescein to assist with observing and viewing the tear film under cobalt blue light (figure 9). Additional use of a yellow ‘Wratten’ filter further improves observation of fluorescence. The stain is usually applied by wetting a fluorescein-impregnated strip with saline, then shaking off any excess liquid and gently touching the conjunctiva with the strip tip. Touching the eye with the paper strip will induce a degree of reflex tearing and instilling too much fluorescein may swamp the normal 8µl tear film, destabilising it. Furthermore, the addition of fluorescein to the tear film alters the physical interactions between its layers, which reduces the surface tension and, hence, affects the break up time value.11 It should be noted that while this technique is invasive, it is still widely used as a method of tear film assessment in practice. Studies have shown that when care is taken to instil a minimal amount of fluorescein that results are comparable with non-invasive techniques.11 Using this technique, a value of less than 10 seconds is typically considered abnormal.12
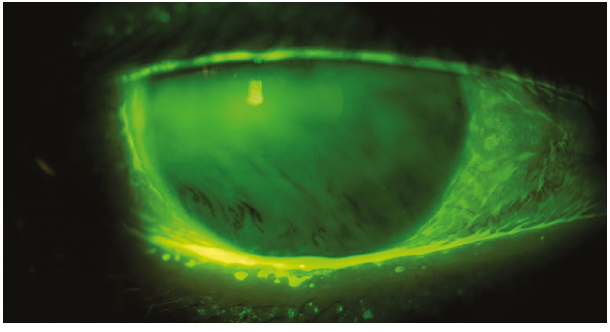
Figure 9: Fluorescein tear break up time, observed as the time taken from a blink to the observation of the first break up, shown here inferiorly as black streaks
Lids, lashes and blinking
The lids and blinking play an important role in the formation and maintenance of a healthy tear film,13 therefore careful observation should be included in a full tear film assessment. Blinking frequency can be observed during slit lamp examination with diffuse illumination, or during history and symptoms. A typical blink pattern should be approximately one blink every three to four seconds, ie between 15 and 20 blinks per minute.14 The tear film is maintained and formed through blinking, and so a reduced blink rate or impartial blink can have a detrimental effect on tear film stability.
It is important not to forget that the lipid layer comprises lipids produced by the meibomian glands and so once any non-invasive methods of assessing the tear film quantity and quality have been carried out, the other ocular surface structures that contribute to the stability of the tear film should also be evaluated. This slit lamp assessment should begin with diffuse illumination to achieve a general overview. Lashes, lid margins, the inner and outer canthi and meibomian glands should all be examined. Traces of make-up and blepharitis will impact tear film stability.
While slit lamp examination will only allow clear observation of the meibomian gland orifices, use of infrared meibography will allow observation of the whole gland (figure 10). As well as allowing practitioners a more detailed view of the meibomian glands, the images can be a useful tool for educating patients on the management of their tear film and/or symptoms.
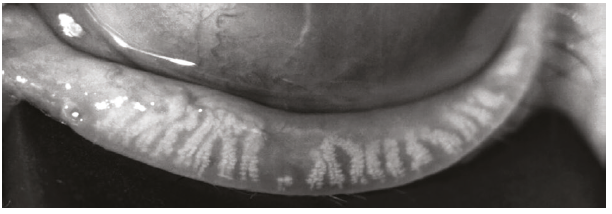
Figure 10: Observation of the inferior meibomian glands using infrared interferometry. Glands are seen as white stalks extending from the lid margin. Here the glands are shortening, with almost complete loss of a gland centrally
Conclusion
Examination of the tear film is one of the most important aspects involved in the fitting and aftercare of contact lens patients. The very nature of contact lens wear results in a tear film that is thinner and less stable than the undisturbed tear film. The transparency of the tears makes it difficult to examine, and the challenge to the practitioner is in developing skills to visualise the structure without causing disruption. Use of non-invasive, or minimally invasive techniques increases the accuracy of tear film assessment and should be employed where possible. No one test is enough, and a combination of tests to assess both tear film quality and quantity is recommended. In addition, consideration of patient symptoms is critical in the overall clinical assessment in both selecting an initial contact lens material, and for continuous care.
Marie-Therese Hall is an optometrist and a paid consultant faculty member for the Johnson & Johnson Institute, UK and a Professional Affairs Consultant for Johnson & Johnson Vision. Dr Rachel Hiscox is a professional education & development manager, UK & Ireland for Johnson & Johnson Vision Care.
This article is part of a revised and updated ‘Essential Contact Lens Practice’ series, originally authored by Jane Veys, John Meyler and Ian Davies. This article was produced without further input or review from the original authors.
References
- Sulley A, Young G et al; Retention Rates In New Contact Lens Wearers. Eye Contact Lens, 2018;44:S273-S282.
- Wilcox M, et al. TFOS DEWS II Tear Film Report. Ocul Surface, 2017;15(3):369-406
- Dilly PN. Structure and function of the tear film. Adv Exp Med Biol, 1994;350:239–247.
- Craig JP, Willcox M, ArgÜeso P, Maissa C, Stahl U, Tomlinson A, Wang J, Yokoi N, Stapleton F. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens interactions with the tear film subcommittee. Invest Ophthalmol Vis Sci 2013;54:TFOS123-56
- Mann A and Tighe B. Contact lens interactions with the tear film. Experimental Eye Research 2013;117:88-98
- Guillon JP and Guillon N. The role of tears in contact lens performance and its measurement. In Contact Lens Practice, (London: Chapman and Hall Medical), 1994; 453-483.
- Osbourne G, Zantos S, et al. Evaluation of tear meniscus heights on marginal dry eye soft lens wearers. Invest Ophthalmol Vis Sci, 1989;30: S501
- Wolffsohn J, et al. TFOS DEWS II Diagnostic Methodology Report. Ocul Surface, 2017; 15(3): 544-579
- Fischer FH, Wiederholt M. Human precorneal tear film; terar film pH measured by microelectrodes. Graefes Arch Clin Exp Ophthalmol, 1982;218(3):168-70
- King-Smith PE, Hinel EA, Nichols JJ. Application of a novel interferometric method to investigate the relation between lipid layer thickness and tear film thinning. Invest Ophthalmol Vis Sci, 2010;51:2418–23
- Mooi JK, Wang MTM, Lim J, Müller A, Craig JP. Minimising instilled volume reduces the impact of fluorescein on clinical measurements of tear film stability. Cont Lens Anterior Eye. 2017 Jun;40(3):170-174
- Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommitte of the International Dry Eye WorkShop. Ocul Surface, 2007;5:108-152.
- Knop E, Knop N, Schirra F. Meibomian glands. Part II: physiology, characteristics, distribution and function of meibomian oil. Ophthalmologe, 2009:106(10):884-92
- Bron A, et al. TFOS DEWS II Pathophysiology Report. Ocul Surface, 2017;15(3):441-515
