Nearly six million people worldwide die every year from various injuries, with projected figures of 8.4 million deaths in 2020.1 In the UK, ‘for every injury death there are 45 hospital episodes, 630 doctor consultations and 5000 to 6000 minor injuries.'2 It is very difficult, however, to get up-to-date statistics on overall injuries and most of the above numbers are already out of date.
Worldwide, there are 55 million eye injuries that leave approximately 1.6 million people blind, 2.3 million with bilateral visual impairment and 19 million with unilateral vision loss.3 Some older UK data suggest a cumulative incidence of ocular trauma of over 8% per 100,000 population annually,4 with trauma commonly accounting for between 10 to 27% of cases presenting in outpatient settings, 38 to 65% of presentations in emergency departments, and 5 to 16% of cases in specialist eye units.5 Most cases occurring in young, male population.6
Over the last century, the causes and patterns of ocular injury have markedly changed with changes in lifestyle, work and effective preventative strategies. Shifts from employment in heavy industry, introduction of national standards for eye protection and increased time for sport and leisure have meant that damage to the eye from penetrating trauma and intra-ocular foreign bodies has been supplanted by blunt injury as the primary cause of hospitalisation. Introduction of compulsory seatbelt wear and laminated windscreens in motor vehicles have almost eradicated the penetrating injuries previously caused by shattering glass, and currently the majority of injuries requiring hospital admission, approximately 30% of the total, occur in the home environment.7
While trauma and injury to the eye can be experienced by all age groups some sectors of the population appear more vulnerable. The incidence of eye trauma appears to have a bimodal trend with peaks in the people aged 15 to 29 years and those over 70 years.8 This is striking, considering that children under the age of five years may be more susceptible anatomically because of their flatter features, rendering eyes vulnerable at the front of the face and thus more exposed, and because their exploration of unfamiliar environments is not matched by maturity of motor skills. Yet, it is young adults and the elderly who are most likely to present for treatment. Indeed, ocular trauma is the primary cause of vision loss in adults under 25 years of age.9 In the younger cohort, this may reflect accidents while unsupervised, participation in higher-risk activities (such as sports), disinhibited behaviour after alcohol and/or drug use, and is also likely to relate to involvement in road traffic accidents (RTAs) which still account for over 50% of eye injuries. Indeed, worldwide around six million children sustain some form of ocular trauma every year and a quarter of a million of these cases require hospitalisation for a serious ocular injury.10
Ageing increases vulnerability to accidents more generally hence frequency of presentation in older adults. It has been suggested that the relationship between age and certain mechanical characteristics of the eye, in particular, those relating to the lens, lens capsule, and cornea, may play an important role.11
Ocular trauma
The College of Optometrists have published guidelines for dealing with ocular trauma.12 A range of symptoms are associated with traumatic injury. These include:
- Pain (from mild to severe)
- Epiphora
- Visual loss (variable)
- Photophobia
- Diplopia
Signs vary depending upon the severity of the injury. Milder cases, where vision is typically unaffected, may show:
- Eyelid swelling (oedema)
- Ecchymosis (bruising)
- Conjunctival chemosis
- Subconjunctival haemorrhage
- Corneal abrasion
In more severe cases, where an associated loss of vision is likely, there are a whole host of possible signs, the nature and number of which are related to the extent, severity, location, duration and actual cause of the trauma. Signs listed in the College guidelines include the following:
- Infraorbital nerve anaesthesia (lower lid, cheek, side of nose, upper lip, teeth) may indicate orbital floor fracture
- Disturbance of ocular motility, either by muscle restriction due to oedema or compression, as in a blow-out fracture
- Enophthalmos (a possible indication of orbital fracture)
- Nosebleeding (direct trauma, or could indicate skull fracture)
- Corneal oedema or laceration
- Anterior chamber activity
- Fixed dilated pupil
- Iridodialysis (tearing of iris from its attachment to ciliary body)
- Crystalline lens damage. This may include subluxation, opacification, or capsule damage
- Intraocular pressure changes. IOP may rise in cases of angle blockage due to blood, inflammatory cells or pigment. IOP may drop if the globe is perforated
- Vitreous haemorrhage (figure 1)
- Commotio retinae
- Retinal detachment or dialysis (figure 2)
- Traumatic macular hole (figure 3)
- Relative afferent pupillary defect

Figure 1: Vitreous haemorrhage
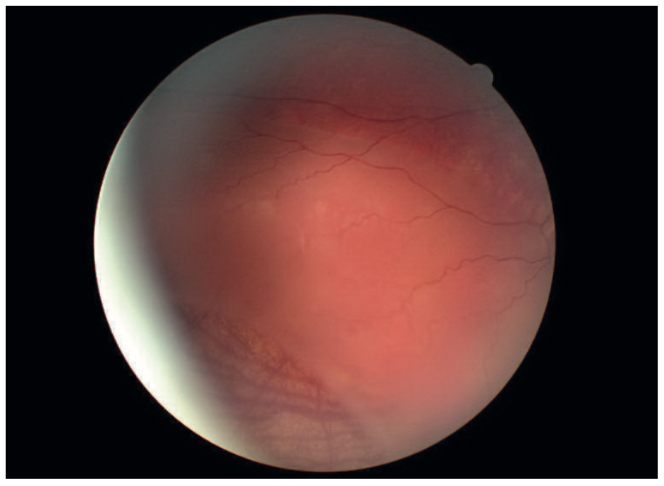
Figure 2: Retinal dialysis after trauma

Figure 3: Traumatic macular hole
Psychological response to ocular trauma
Although causes of ocular trauma have shifted and those incurred tend to be less severe than in previous decades, eye trauma remains both common and potentially disastrous, with millions of people rendered blind in one or both eyes by their injuries. This has a significant personal, social and economic impact. An overwhelming focus on the physical consequences of eye trauma and, in some instances, a justifiable focus on emergency treatments, has meant that the emotional consequences have been, somewhat, neglected. Nevertheless, there is clear evidence that those who experience ocular trauma can experience substantial and enduring distress and for a lengthy period after the injury itself.13
Post-traumatic stress disorders (PTSD) can occur after various types of traumatic events, including eye injuries. Indeed, following the introduction of PTSD into the Diagnostic and Statistical Manual of Mental Disorders in 1980,14 it has also been recognised that the traumas of daily life are also potent sources of psychopathology and problems of adjustment.15 PTSD usually occurs in individuals that have experienced or witnessed an event that involved actual or threatened death or serious injury, or a threat to the physical integrity of the self or others. The individuals should also have experienced an immediate response involving intense fear, helplessness or horror. Damage to the eye is also likely to cause significant distress, leading to symptoms of agitation, intense feelings of fear, a numbing of emotional reactions, mood change and even impaired cognition.
Optometrists will not be able to assess if their patients suffer of PTSD due to ocular traumas. In addition, distinctions will need to be made between psychological issues that might have existed for the patient prior to the eye trauma and those that have been caused by or magnified by the trauma itself and this is beyond the current optometric practice. It is of note that patients more vulnerable to developing PTSD after an ocular injury are those with previous psychiatric history, predisposition to labile mood or having difficulty making sense of events around the trauma.13 Full diagnostic criteria for PTSD, identified by the American Psychiatric Association in their diagnostic manual, are shown in table 1.16
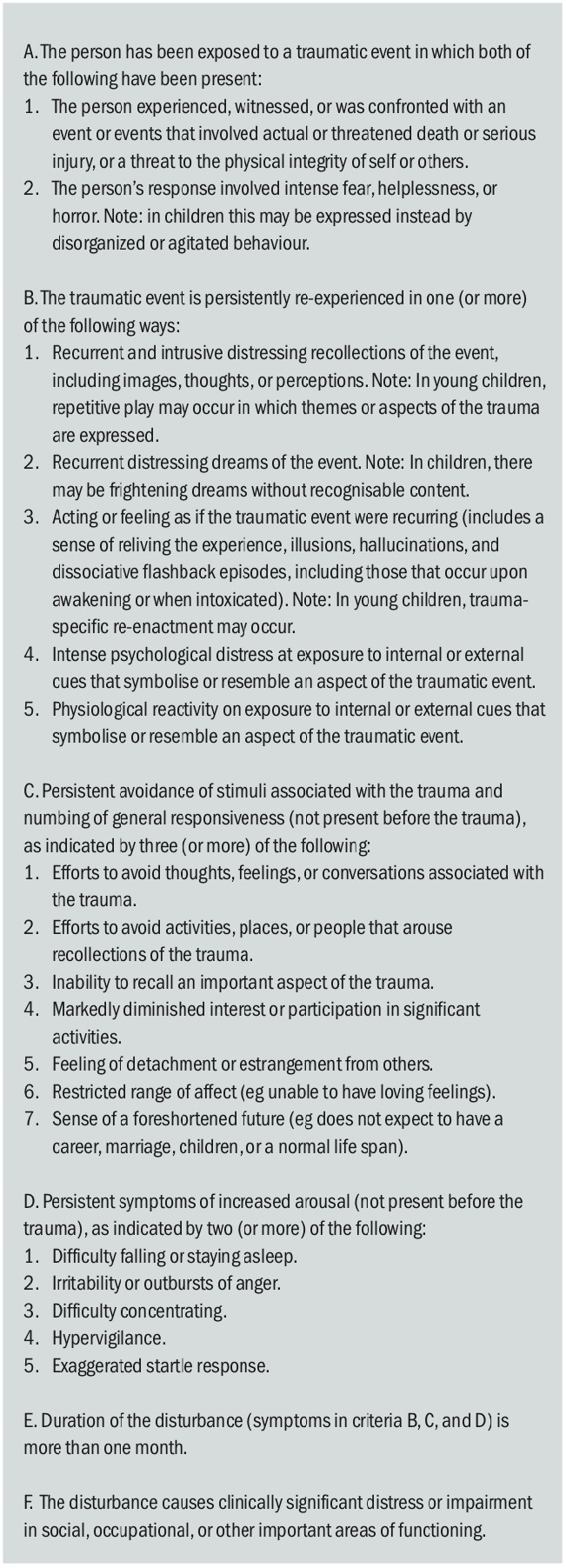
Table 1: DSM-IV-R criteria for the diagnosis of post-traumatic stress disorder (PTSD)
Although the optometrists are not involved in the diagnosis of PTSD after ocular trauma, the below case study will help to understand the psychological effects that a major incident can have on our patients.
Case study
Dan is a 42-year-old man who worked as a lorry driver. On an early afternoon, he was forced to pull his lorry on to the hard shoulder. Having stopped the vehicle, he moved over to the passenger seat, opened the door and sat on the edge of the seat dialling the recovery services on his mobile phone. As he made the call, he noticed movement reflected in the wing mirror of the open door and realised a lorry was moving at some speed towards him. He remembered thinking to himself that ‘this lorry’s not going to pull up in time – it’s going to hit me’. He disclosed his mounting horror as the lorry continued on its path, looming darkness and the sound of metal crumpling and a smell of burning tyres.
Dan had little detailed memory of the subsequent events, believes he was knocked out and, on regaining consciousness, was aware of a searing pain across his forehead, eye and jaw and wetness, which he later realised was blood. He was in partial darkness and was pinioned between the cab of his vehicle and the embankment at the side of the road. Dan’s story (which he managed to recall over a number of therapy sessions and with considerable initial distress) follows: ‘I was terrified. I couldn’t see very well. I was in agony and I was trapped. I was frightened that the cab would roll further or that the fuel tank would go up. The worst bit was waiting for help. I could hear voices that sounded a bit panicky and someone saying they thought I must be dead. All I could imagine was that I’d die without seeing my children again and I couldn’t see anything. I felt so frightened.’
Dan was eventually freed from his lorry and taken by air ambulance to hospital where he remained for almost two weeks, having fractured an arm and ribs, and with a penetrating injury to his left eye and severe lacerations to his face. He reported feeling: ‘A bit spaced-out, detached-like. I couldn’t talk to the wife and all my friends said I was lucky to have got off lightly. When I tried to think about it, I started to feel shaky and sick. I couldn’t go back to work because I couldn’t drive, and I couldn’t go near a car, dreaded it, even as a passenger, never mind going near the accident. My head felt as it would explode I was so tense and wound up.’ Dan also reported nightmares, intrusive images and flashbacks over the next few weeks. He became frightened of falling asleep because the dreaming left him nauseous, sweating profusely and very alert. Dan also found that fractured sleep made him irritable and fatigued during the day, and without his usual routine he became depressed and began to increase his alcohol use to help him sleep. His changed and labile mood and behaviour began to sour his relationship with his wife and both withdrew from one another. At the time he was referred to the psychologist, Dan’s symptoms had been present for almost seven months.
Dan’s case illustrates three key clusters of symptoms that typify presentations of PTSD17 (as summarised in table 2). These were:
Avoidance. With Dan this was most obvious in his unwillingness to talk or think about what had occurred. It also characterised his behaviour, avoiding car travel wherever possible and complete avoidance of the crash site, to such an extent that he would insist on driving longer routes.
Arousal. After this traumatic accident Dan presented with a hyper-aroused physiological state, always alert for something awful to occur, sleeping badly with erratic and irritable behaviour.
Re-experiencing. For Dan, as with others with PTSD, re-experiencing included intrusions through dreams and nightmares, flashbacks (where he felt himself back in his lorry cab and in imminent danger), and intrusive thoughts. Intrusions can occur either spontaneously or as a consequence of deliberate rumination.

Table 2: PTSD - symptom clusters17
In addition to these three key clusters of PTSD symptoms, the eye care practitioner should be aware of other psychosocial consequences (table 3).

Table 3: Other possible psychosocial consequences of ocular trauma
Conclusion
The main role of eye care professionals resides in preventing ocular injuries through appropriate education, which will increase people’s knowledge about avoiding and protecting themselves against risks. Nevertheless, it seems that the role of education on its own is limited.18 In addition, it is also possible to deal with a recent eye injury, first hand. The College of Optometrists has published guidelines for dealing with ocular trauma.12 When it comes to the psychological effects, however, recognising the possible warning signs and working with an appropriate multidisciplinary team for the benefit of the patient, might be the best approach.
Dr Doina Gherghel is an academic ophthalmologist with spe- cial interest in inter-professional learning for optometrists. She also leads the Geriatric Optometry module at Aston University. For further information, go to pgadmissions@aston.ac.uk.
References
- Murray CL, Lopez AD: Alternative projections of mortality and disability by cause 1990–2020. Lancet 1997, 349:1498- 504
- British Medical Association: Injury prevention BMA: London; 2001
- MacEwen CJ. Ocular injuries. J R Coll Surg Edinb. 1999 Oct;44(5):317-23
- https://www.ncbi.nlm.nih.gov/pubmed/8795369
- Negrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiology, 1998; 5:143–69
- https://www.ncbi.nlm.nih.gov/pubmed/24097120
- https://academic.oup.com/jpubhealth/article/29/1/72/1584816
- https://www.ncbi.nlm.nih.gov/pubmed/8795369
- Negrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiology, 1998; 5:143–69
- Tielsh JM, Parver L, Belavadi S. Time trends in the incidence of hospitalized ocular trauma. Arch Ophthalmol., 989;107(4):519–23
- McGwin G, Jr, Hall TA, Xie A, Owsley C. Trends in eye injury in the United States, 1992–2001. J Vision. 2006;47:512–27
- https://www.college-optometrists.org/guidance/clinical-management-guidelines/trauma-blunt-.html
- Abbott J, Shah P. The epidemiology and etiology of pediatric ocular trauma. Surv Ophthalmol. 2013;58:476–485
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217536/
- https://www.ncbi.nlm.nih.gov/pubmed/11316717
- https://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596
- Greaves I, Porter K, Burke D, Alexander DA (1997) Psychological aspects of trauma. in Key topics in.eds Greaves I, Porter K, Burke D(Bios Scientific Publishers, Oxford), pp 249–257
- https://www.ncbi.nlm.nih.gov/books/NBK83241/
- https://www.ncbi.nlm.nih.gov/books/NBK207191/box/part1_ch3.box16/
- Shah A, Blackhall K, Ker K, Patel D. Educational interventions for the prevention of eye injuries. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No. CD006527.
