We recently published an article by Dr Doina Gherghel discussing ocular trauma and its potential to cause post traumatic stress disorder (http://fplreflib.findlay.co.uk/images/optician/pdf/022_OPT_170120_CET_PTSD.pdf). This article highlighted:
- The incidence of eye trauma appears to have a bimodal trend with peaks in the people aged 15 to 29 years and those over 70 years
- Ocular trauma is the primary cause of vision loss in adults under 25 years of age. In the younger cohort, this may reflect accidents while unsupervised, participation in higher-risk activities (such as sports), disinhibited behaviour after alcohol and/or drug use, and is also likely to relate to involvement in road traffic accidents (RTAs) which still account for over 50% of eye injuries
- Aging increases vulnerability to accidents more generally hence frequency of presentation in older adults
The College of Optometrists have published guidelines for dealing with ocular trauma.1 ABDO also offer guidance regarding the need for referral for dispensing opticians.3
A range of symptoms are associated with traumatic injury. These include:
- Pain (from mild to severe)
- Epiphora
- Visual loss (variable)
- Photophobia
- Diplopia
Signs vary depending upon the severity of the injury. Milder cases, where vision is typically unaffected, may show:
- Eyelid swelling (oedema)
- Ecchymosis (bruising)
- Conjunctival chemosis
- Subconjunctival haemorrhage
- Corneal abrasion
In more severe cases, where an associated loss of vision is likely, there are a whole host of possible signs, the nature and number of which are related to the extent, severity, location, duration and actual cause of the trauma.
Standards of Practice
A key component of the GOC Standards of Practice2 is the need for all staff in a practice to be able to manage appropriately any patient presenting. It is the responsibility of the registered professional in any practice to ensure that ancillary, support staff have adequate understanding of what may constitute a medical emergency and know to whom to refer, even when there may not be any registered professional in attendance at the time. In most cases, staff are trained to complete some form of triage document (figure 1) and then to contact the relevant professional as soon as possible. The training of staff in being able to undertake this appropriately is the responsibility of the registered staff member, and a range of training materials are available to help ensure this is undertaken (figure 2).

Figure 1: Triage document
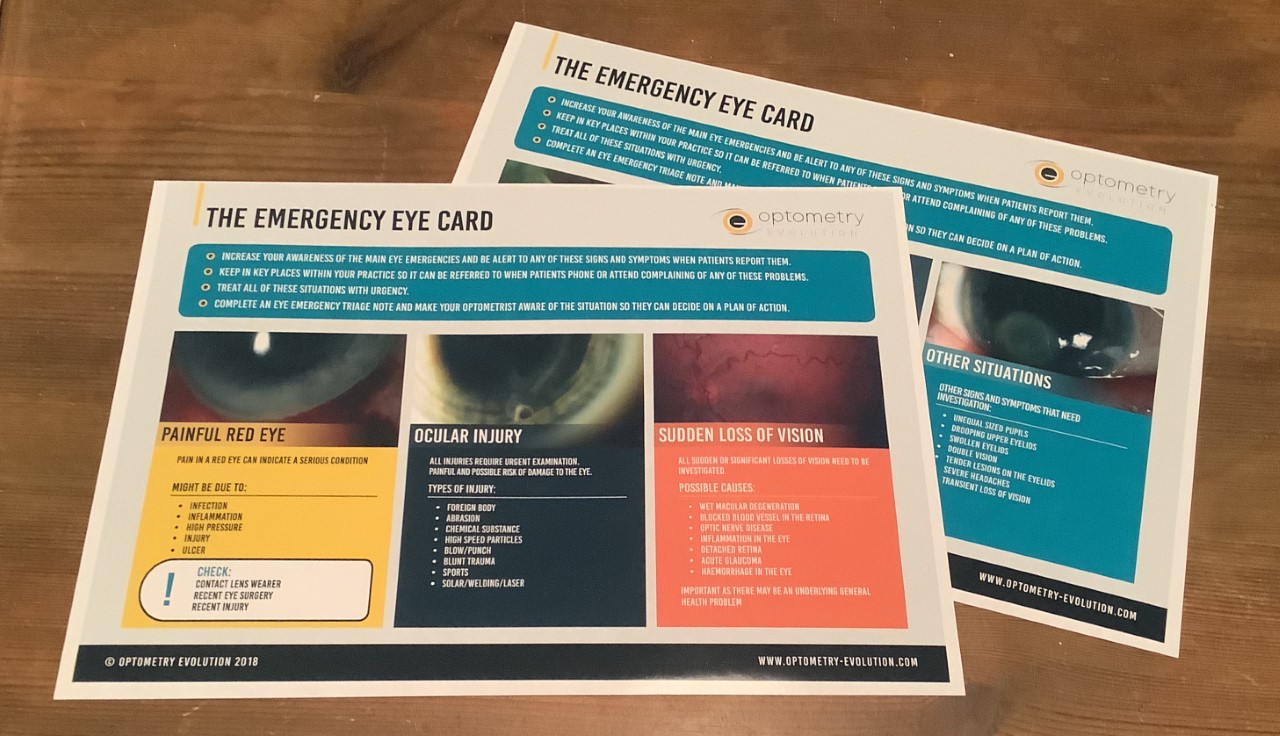
Figure 2: Training materials for support staff
Interactive Exercise
Our exercise centres on the best approach to managing a patient with a recent history of blunt trauma (they were elbowed in the eye at a rugby match the previous day) who attends in practice when no registered professional is present. They complain of photophobia and increasing discomfort and the eye looks red, lid oedema, watering... only naked eye assessment available.
After completing the six accompanying multiple choice questions, you will then need to discuss with a fellow registrant your views of the potential injury and what you would want the support staff member to do in this situation.
Remember:
- There is no one single answer for your discussion, but what is needed is a reflection of your discussion (which must be for a minimum of 10 minutes please) that is sufficient evidence of the various points having been covered.
- Go to opticianonline.net and click into the CET zone where you can select this exercise
- Read the source material available
- Complete six multiple choice questions to confirm you have grasped the main concepts
- Read the case scenario about which you are to confer with a registered colleague (for at least 10 minutes please)
- Confirm with us the name and GOC registration number of the colleague with whom you have discussed the case and also write some short notes on the outcome of your discussion
- At the end of the month’s active period we will confirm that your discussion outcome meets the requirement for an interactive point.
Stanley Keys is a hospital optometrist based in Inverness, Scotland.
• Look out for a published discussion based on all responses in a future issue of Optician.
