When we think of communication, we generally think about speaking. Before we get to our first birthday, we are able to say ‘mama’ or ‘dada’. By the time we were two we were forming two to four-word sentences and on graduating we probably had a vocabulary of some 10,000 words to choose from.
In optical practice we speak when we first meet our patients, we rely on speech to enquire about their history and symptoms. Treatment recommendations are generally given verbally. Understanding how speech is processed is critically important in being an effective communicator. In the next part of this series we will consider the impact that non-verbal elements, such as body language, have on understanding the spoken word, but this article will consider the use of language in effective communication.
How the spoken word is processed.
The mechanism by which sound waves are converted into electrical neural signals is well understood and documented.1 How those sounds are then processed by the brain is more complex and it has only really been since the advent of magnetic resonance imaging (MRI) that we have been able to really understand the mechanisms by which speech is processed. In the same way that signals from the eye pass through to the visual cortex, those from the ear pass firstly to the auditory cortex, located within the temporal lobes. Cells within the cortex are thought to be able to pick up specific sounds in terms of their pitch, intensity and tonality.
The interpretation of stimulus to the auditory cortex involves multiple areas of the brain across both hemispheres (see figure 1). In the 19th century Wernicke and Broca identified areas of the brain, named after them, which are responsible for processing speech. What MRI studies show is that specific words are processed by multiple different parts of the brain. Memories and associations with words are pulled from across the cerebellum and processed within the inferior parietal lobe and fusiform gyrus within the frontal lobe. The wide dispersion of the structures within the brain associated with language processing makes language, and more importantly language interpretation, highly susceptible to any structural disease or trauma.

Figure 1: Brain areas active when hearing, seeing and speaking words
The Paradigm and Accepted Patient Beliefs
A paradigm can be defined as a cognitive framework shared by members of any discipline or group. It is a belief system through which all new information is filtered and judged. In a sporting context a group of die-hard football fans may have the paradigm that the club they support is the best. Any challenge to the superiority of their club, be it from rival supporters, journalists or video assisted refereeing decisions, will be viewed as a direct affront to their beliefs. In business a retailer may have marketed itself as an exclusive, upmarket supplier with the consequence that the consumer sees them as being expensive. The customer’s paradigm with respect to that retailer is of high cost and, should the retailer wish to change this, then a ‘paradigm shift’ is required to alter those beliefs.
The extension of the paradigm into health care is the accepted patient belief (APB). The APBs are the statements of perceived fact that the patient has about their health, their treatment or any effectiveness that any intervention from a health care practitioner may have on them. Adherence (compliance) to anti-depressants is a function of the beliefs that the patient has on their needs and potential side effects.2 The same was found in diabetes, where disease and medication beliefs which were inconsistent with the chronic disease model were significant predictors of poor medicinal adherence.3
Understanding individual’s APBs plays an important role in effective communication. When a question is asked it is heard, processed and then the information compared against existing beliefs. The answer comes framed by that belief system (figure 2) which is in turn then processed by the practitioner’s belief system. So, as an example:
Practitioner (says): ‘How do your contact lenses feel at the end of the day?’
Patient (thinks): ‘I really want to keep wearing my contact lenses, I know they get sore at the end of the day, but that’s surely normal, if I tell my practitioner there is a problem, they may take the lenses from me.’
Patient (says): ‘They are fine, no problems’
An opportunity to improve patient satisfaction, and in this case potential future drop out is lost.
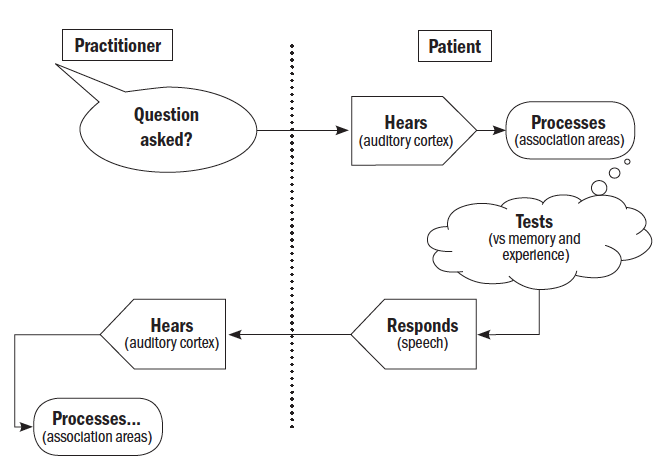
Figure 2: Accepted patient beliefs
Uncovering APBs and debunking those that are incorrect is critically important. Questions such as:
- ‘What do you know about …?’
- ‘How do you feel about …?’
- ‘What have people told you about …?’
- ‘Have you done any online research about …? What did you learn …?’
All give the patient an opportunity to explain their knowledge base and give the practitioner an opportunity to educate appropriately. Understanding the source of a patient’s (mis)information will also help in directing them towards the proof source data that they will find most compelling.
The concept of the accepted belief goes beyond interactions with patients. It is also important that within a practice team there is consistency about what constitutes success. Imagine a conversation along the lines of:
Practice manager (says): ‘How has the day been?’
Receptionist (thinks): ‘There is nothing worse than having the phone ringing all day, having to deal with lots of people and it has been lovely to have some time to myself’
Receptionist (says): ‘It’s been a great day, thank you!’
A quiet day with no patient interaction probably is not ideal for business.
Open and closed questions
Very few patients are excited about seeing any health care practitioner. They are in an unfamiliar environment on an irregular basis and may be nervous about the appointment. I have heard the most common response to a GP asking their patient how they are when they first enter the consulting room is often: ‘fine’, when clearly in most cases they would not be there if they were fine. It is the role of the practitioner and support staff to put the patient at ease, so information about how they feel about their vision can be efficiently, effectively and accurately taken.
Questioning technique plays a large part in this and it is important to understand the difference between open and closed questions. An open question is one which demands a sentence as an answer whereas a closed question can be answered with a single word, often ‘yes’ or ‘no’. A classic example of the difference between the two questioning techniques comes from contact lens practice; ‘Are your lenses comfortable?’ prompts a binary yes/no answer, whereas ‘Tell me how your contact lenses feel towards the end of the day,’ encourages the start of a dialogue and opens the opportunity for follow-up discussion and supplemental questions. In one controlled study the use of open-ended questions significantly increased the amount of information elicited from patients.4 Table 1 shows example of open vs closed questions.
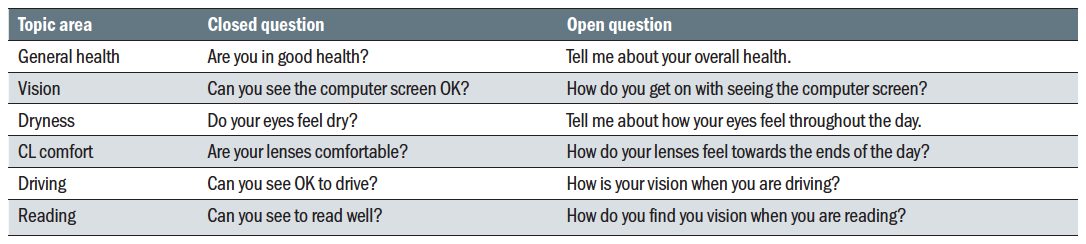
Table 1: Open vs Closed Questions
Active listening
Learning to listen well is as important as learning to speak clearly. The practitioner must make it clear to the patient that what they are saying is being understood and taken seriously. Not only is this important in making efficient diagnoses, but it is also important in managing practice time. If a patient does not believe that they are being listened to, they will tend to repeat the same point several times, taking up valuable chair time. Active listening also helps the practitioner concentrate on the matters in hand.
Active listening starts with the creation of an environment free from distraction. Mobile phones should not be out on the desk and should have any audible notifications switched off. Computer screens should only have information immediately relevant to the consultation showing. However interesting the live sports or news feed may be (and I know of instances when these have not been switched off) they are not helpful in indicating that you are interested in what the patient has to say.
Body language also plays a role in active listening and we will be covering this more in a future part of this series. At the very least, by sitting slightly forward with head tilted towards the patient, the practitioner is indicating an active interest in what is being said (figure 3). The use of hand movements to pause the patient or slow them down can also be effective. Sitting back, with arms and legs crossed, gazing in to the distance is not recommended.

Figure 3: Active listening, on the left, should encourage better rapport than closed behaviours (right)
By far the most effective technique in active listening is to stop the patient and paraphrase back what they told you before recording it in the notes. This can be especially effective with some nervous patients who may come in with a liturgy of symptoms that they want to share. Letting them voice their symptoms without interruption shows respect for what they have to say. Once finished, then the practitioner should recap what they have heard, noting the salient points and thanking the patient for the information. Allowing a patient to tell their story without interruption is a skill that is worth developing. In an often-quoted study, doctors were found to interrupt patients after just 11 seconds of listening to their history and symptoms.5
Impact of personality
Individual personalities have a major impact on how information is both transmitted and received.
In part one of this series we touched on the importance of understanding the practitioner’s own personality traits as a tool to become a better communicator. The perception of the spoken word is impacted by many structures within the brain and so the personality trait of the patient will play a major role in how information is understood.
Current psychology thinking proposes that there are five major personality traits (figure 4), each of which plays a varying part in making up an individual personality.6 Often referred to by the acronym OCEAN, these are:
- Openness to experience - A person’s willingness to try new experiences, experiment with new ideas and think creatively.
- Conscientiousness - Having a high level of self-control and discipline, working within the rules and planning each activity carefully.
- Extroversion - A person who draws their energy from interacting with others, outgoing with high levels of sociability and self-confidence.
- Agreeableness - People with a strong desire to get on with others, polite and sensitive who do not want to ‘cause a scene’.
- Neuroticism - The level of confidence and comfort that a person has with themselves, a tendency to be pessimistic, anxious and lacking in self-confidence.

Figure 4: Personality traits
By listening carefully to the way that a patient expresses themselves and responds to questions, the practitioner should be able to develop a sense of which the dominant personality trait of the patient is. Table 2 maps out some ‘dos’ and ‘do nots’ in speaking with patients with each dominant trait.
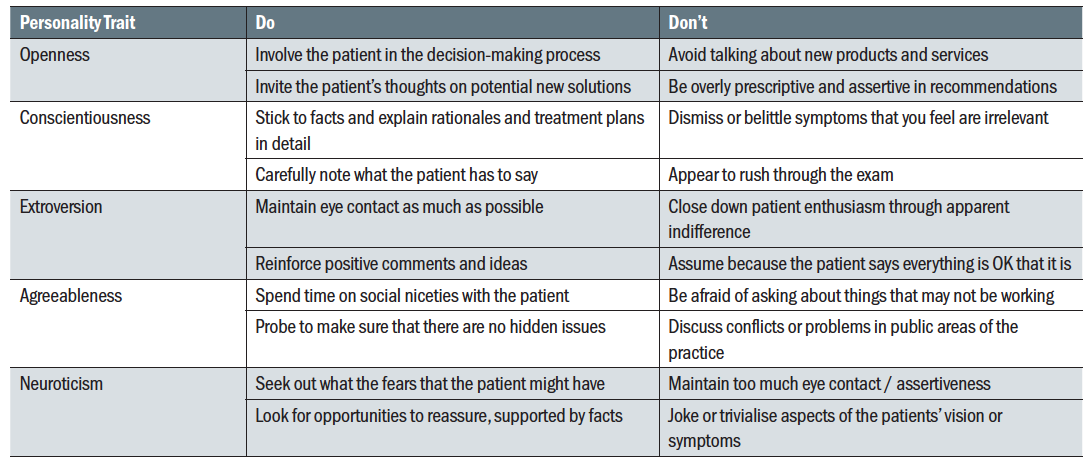
Table 2: Questioning techniques for different personality traits
The autistic patient
Just over 1% of the UK population has autism, or more correctly, sit on the autistic spectrum. Autism is defined by the National Autistic Society as a lifelong developmental disability that affects how people perceive the world and interact with others. The extent by which the condition impacts the individual is variable (hence the spectrum definition) and, in most cases, there are no visible signs of the condition.
Autistic people often find the world overwhelming and many have a literal understanding of language, struggling to interpret verbal and non-verbal communication, despite often having a higher than average intelligence. Autistic patients in practice will be helped with an uncluttered environment and sudden loud noises should be avoided. Clarity in speech is important and, in direct contradiction to earlier comments on open vs closed questions, autistic patients may require a more directive approach. A question such as ‘Tell me how your vision is at school?’ can be confusing and a series of closed questions such as: ‘Can you read the words on the screen from your desk?’ maybe easier to understand. Jokes and light-hearted attempts to put the patient at ease may not be understood in the way that they were intended and should be used with care.
Summary
Effective verbal communication involves many structures within the brain and so is impacted by many factors. Personality, existing beliefs and past experiences all impact on what a patient hears when asked a question. The use of carefully constructed open questions and the ability to engage in active listening are both critical in getting points made. In the next article I will look at the impact of non-verbal communication.
Ian Davies is an optometrist now working as an independent motivational speaker, coach and business consultant.
References
- Abbott D (2016) What brain regions control our language? And how do we know this. Available at https://theconversation.com/what-brain-regions-control-our-language-and-how-do-we-know-this-63318
- Aikens JE, Nease DE, Nau DP et al (2005) Adherence to maintenance – phase medication as a function of patient beliefs about medication. Ann Fam Med 3(1) 23-30.
- Mann DM, Ponieman D, Leventhal H et al (2009) Predictors of adherence to diabetes medications: the role of disease and medication beliefs. J Behav Med 32:278.
- Takemura Y, Sakurai Y, Yokoya S et al (2005) Open-ended questions: are they really beneficial for gathering medical information from patients? Tohoku J Exp Med 206(2):151-4
- Rhoades DR, McFarland KF, Finch WH et al (2001) Speaking and interruptions during primary care office visits. Fam Med 33(7):528-32.
- Ackerman CE (2019). Big Five Personality Traits: The Ocean Model Explained. Available at http://positivepsychology.com/big-five-personaility-theory/
